Types of acquired red moles on the body
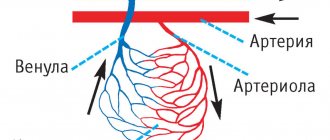
- Simple (capillary). Proliferation of newly formed capillaries, small venous and arterial vessels. Looks like a red spot.
- Cavernous. A spongy cavity with blood - a red or bluish nodule. Often forms under the skin.
- Branched (racellose). A plexus of tortuous dilated capillary trunks. They pulsate, noise and trembling are detected. It is rare and occurs on the extremities or face. If injured, life-threatening bleeding may occur.
How to identify hemangioma? Press on top of it and it should fade or disappear.
Treatment of spider veins
Spider veins tend to progress: an increasing number of neighboring capillaries are involved in the process, and entire “networks” are formed. The easier it is to get rid of “stars”, the smaller the area they occupy.
Removal of spider veins is carried out using various conservative and surgical methods: sclerotherapy, ozone therapy, radio wave and laser methods.
1
Sclerotherapy in MedicCity
2 Sclerotherapy in MedicCity
3 Sclerotherapy in MedicCity
The radio wave method (Surgitron) is the removal of an enlarged capillary using a thin electrode without damaging surrounding tissues and healthy vessels. An ideal method for removing single spider veins on the face, which does not leave scars.
1 Laser removal of spider veins in MedicCity
2 Laser removal of spider veins in MedicCity
3 Laser removal of spider veins in MedicCity
Removal of spider veins with a laser (laser coagulation) is used in the presence of widespread vascular network. The laser beam is selectively absorbed by the pathological vessel forming the spider vein and heats it. At high temperatures, the walls of the vessel stick together, and the vessel is irreversibly damaged.
Sclerotherapy (introduction of a sclerosant into the lumen of the vessel, which causes adhesion of the vessel walls) is effective against fairly large telangiectasias, located mainly on the legs.
You can learn how sclerotherapy is performed from the video. The procedure takes place on an outpatient basis, before our eyes: thanks to a simple injection, the patient gets rid of spider veins on her leg.
Spider veins may appear again. To prevent relapse, it is necessary to take medications to strengthen blood vessels and use compression stockings.
1 Before and after removal of spider veins using sclerotherapy in MedicCity
2 Before and after removal of spider veins using sclerotherapy in MedicCity
3 Before and after removal of spider veins using sclerotherapy in MedicCity
4 Before and after removal of spider veins using sclerotherapy in MedicCity
5 Before and after removal of spider veins using sclerotherapy in MedicCity
Are red moles dangerous?
In themselves, these formations are harmless and are not precancers.
If you have a lot of red moles on your body, the cause may be a serious liver or pancreas disease. Pay attention to this - this is a reason for examination.
Problems may arise in case of traumatization of hemangiomas. Even fairly small formations threaten heavy bleeding, which is not easy to stop.
Clinical case
Patient L, 26 years old, presented with a traumatized mass in the axillary region. According to her, she tore off a convex hemnagioma with the edge of a rigid corset of a wedding dress almost a few minutes before the start of the wedding ceremony. The hemangioma bled very heavily and a large blood stain appeared on her white dress. She had to wear the witness's jacket over her wedding dress. It was in such a strange outfit that the wedding took place.
Why blood vessels burst in the legs: reasons
Fragility of capillaries and small veins can be caused by endogenous (internal) and exogenous (external) factors. In the first case, we are talking about the following reasons:
- Phlebeurysm. Disruption of the valvular apparatus of the veins leads to a change in blood flow: the diameter of the veins increases, they become more tortuous, and their walls become thinner. As a result, there is an increase in the severity of the vascular network, the person complains of a feeling of heaviness and fullness in the lower extremities, swelling and cramps appear. In the later stages of the development of the disease, a violation of the trophism of soft tissues is possible, accompanied by the appearance of dark spots and difficult-to-heal ulcers on the skin.
Expert opinion
One of the first symptoms of varicose veins is the appearance of telangiectasias on the lower extremities - vascular “stars” and “webs” of a reddish, purple or bluish color. If telangiectasias occur, it is recommended to consult a phlebologist and, if necessary, begin treatment. Since they appear at a very early stage of varicose veins, these changes usually respond well to conservative treatment. However, if taking venotonics does not give the desired result, it is possible to remove telangiectasia using minimally invasive surgical methods - for example, laser coagulation or sclerotherapy.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
- Endocrine disorders. This primarily concerns diabetes mellitus: if the disease is not treated, diet is not followed, lifestyle changes and blood sugar levels are controlled, diabetes can lead to a number of serious complications, one of which is vascular disorders. In particular, this applies to peripheral capillaries and veins: with diabetes, veins often burst and bruises form on the legs, tissue trophism is disrupted, and poorly healing ulcers can occur.
- Cardiovascular diseases. Any pathology affecting the heart, large veins and arteries automatically affects the condition of small peripheral vessels.
- Pregnancy and lactation. The appearance of spots and bruises on the lower extremities, strengthening of the vascular network, increased capillary fragility - all these are quite common phenomena that accompany the period of bearing a baby and breastfeeding. Most often, their occurrence is triggered by changes in the hormonal balance of a woman’s body, as well as an increase in her body weight.
- Systemic lupus erythematosus. This autoimmune disease is characterized by damage to the microvasculature.
- Hormone replacement therapy and oral contraceptives. Estrogen-containing drugs provoke a decrease in the elasticity of veins and capillaries, increase blood clotting and slow down the speed of blood flow. This is one of the reasons why blood vessels in the legs burst more often in women than in men.
- Taking anticoagulants. One of the complications of therapy using blood thinning drugs is increased fragility of capillaries and small veins. As a result of this, blood vessels burst on the patient’s body (in particular on the lower extremities) and bruises appear.
Expert opinion
If you are taking warfarin, an indirect anticoagulant that blocks blood clotting factors, you need to have your blood tested regularly (about once a month). The results of the study make it possible to quickly change the dose of the drug to prevent the appearance of bruises, subcutaneous hemorrhages and bleeding.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
- Allergic reactions. One of the symptoms of allergies is redness of the skin due to the expansion of capillaries and increased permeability of their walls. In particular, their fragility increases - most often the vessels burst on the lower extremities, chest, back and face.
- Smoking and alcohol abuse. Alcohol and nicotine cause an increase in heart rate, increased blood pressure, the release of adrenaline into the blood, provoke blood thickening and impede blood flow. Due to this, the load on the veins gradually increases, leading to their deformation and fragility.
- Overweight and obesity. The higher a person’s body weight, the greater the load placed on the lower limbs. In addition, overweight people are more likely to have hypertension, which causes a decrease in the elasticity of blood vessels.
- Unbalanced nutrition, hypo- and avitaminosis. Insufficient intake of magnesium, potassium, Omega-3 and Omega-6 fatty acids, ascorbic acid, B vitamins, coenzyme Q10 and other substances necessary for the normal functioning of the cardiovascular system leads to fragility of veins and capillaries.
- Elderly age. As the body ages, the permeability of capillary walls may increase, and their elasticity may decrease. This leads to small blood vessels in the lower extremities often bursting in older men and women.
Vessels burst in the legs: causes
Vessels in the legs and arms can burst due to the following exogenous factors:
- Injuries. Bruises, compression, abrasions and other mechanical damage provoke a violation of the integrity of capillaries and veins.
- Exposure to ultraviolet radiation. Prolonged exposure to direct sunlight or in a solarium leads to vasodilation, provoking the development of ultraviolet erythema - a hyperemic, painful and swollen area of the skin. In addition, prolonged UV exposure is accompanied by loss of fluid from the body, which makes the blood thicker and more prone to blood clots.
- Excessive or insufficient physical activity. If a person leads a sedentary lifestyle and moves little, any physical activity is stressful for the body. This also applies to stress on the lower extremities - with prolonged walking, running or standing, the vessels of the lower extremities of an untrained person can expand and burst. The same applies to excessive physical activity in trained athletes.
- Mechanical impact during cosmetic procedures. Acid and mechanical peels, massage, laser hair removal, sugaring, waxing - all this can negatively affect the condition of the vessels of the lower extremities, especially in the presence of concomitant pathologies (for example, varicose veins, diabetes, cardiovascular diseases, etc.)
Artificial
Artificial spots on the skin are spots that appear when dyes are artificially introduced into the skin. Such spots include tattoos and contour makeup.
Any spots on the skin require close attention. They can change over time, become malignant and become life-threatening. This is especially true for so-called moles. Therefore, specialists at the Dermatology Clinic advise you to be on guard with spots and if they transform - enlargement, changes in shape and color, or itching - immediately consult a dermatologist.