A hematoma is an accumulation of blood in the tissues of the human body, and its occurrence is caused by damage due to falls and blows. In some cases, the appearance of a hematoma is not associated with physical effects, but is explained by the presence of a specific disease in a person.
In most situations (this applies to small hematomas), serious consequences do not occur, and the inflammation itself disappears after some time. However, there are often cases that require medical consultation and qualified treatment. Ignoring a bruise can lead to the formation of a cyst or tissue necrosis.
Why it is not recommended to treat a hematoma on the leg at home
If there is large accumulation of blood under the skin, it must be removed. There are enough videos and articles on the Internet describing this procedure at home, but you absolutely cannot follow such advice. Firstly, a person risks damaging his leg even more and disrupting its normal functioning, even to the point of disability. Secondly, and more likely, you can introduce an infection into the body and provoke even greater inflammation. Thirdly, only an experienced doctor using special equipment will do this carefully, but independent attempts can permanently disfigure the skin and leave unaesthetic scars on it.
Reasons why bruises often appear on the legs
The appearance of bruises on the legs without a blow or injury is an alarming sign indicating health problems. Most often they occur suddenly and may be accompanied by bruising. In this case, you should not delay a visit to the doctor, since if the blood vessels are in normal condition without injury, hemorrhage does not occur in the upper layers of the skin. In case of injuries, they can remain on the legs for quite a long time and this is a type of norm that does not require special treatment.
Among them may be:
- Vitamin deficiency, in which due to a lack of vitamins C, K, P, the elasticity of the walls of blood vessels decreases and their fragility increases. If you adjust the menu and replenish it with rose hips, black currants, chokeberries, then the lack of vitamins can be compensated. Most often, such bruises appear in the spring, when the manifestations of vitamin deficiency are most severe.
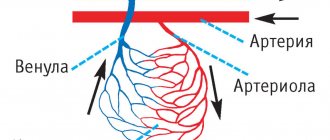
- Reduced strength of the connective tissue that protects the capillaries. In this case, the appearance of bruises on the legs without a contusion becomes possible with the slightest pressure. This needs to be diagnosed (which is only possible in a specialized center). If the diagnosis is established, sometimes the fragility of blood vessels can be eliminated by taking special medications.
- Lack of platelets, in other words, a blood disease in which there are problems with blood clotting. The localization of bruises is not limited to the legs alone; they also appear on other parts of the body.
- Varicose veins, which not only cause bruising, but also spider veins. The appearance of bruises in this case may be accompanied by a feeling of heaviness in the legs, swelling, and bloating of the veins. As a treatment, the doctor will prescribe you: taking special medications that increase the tone of the veins; sclerotherapy (bonding of blood vessels through subcutaneous administration of drugs); wearing special knitwear that maintains muscle and vein tone).
- Hemorrhagic vasculitis. The reason for the appearance of this disease lies in the fact that the immune system fails and the cells of the blood vessels are perceived as foreign. The IS begins to produce antibodies that destroy the walls of blood vessels. This leads to inflammation, and as a result, the appearance of hematomas.
- Yellow bruises may indicate ruptured blood vessels. This is typical for people actively involved in sports. Under heavy load, capillaries under the skin of the extremities inevitably burst. As a result, bruises appear. Therefore, if after a fitness class your legs hurt a lot and bruises appear, we recommend reducing the level of stress during training.
- The appearance of bruises on the body may be a consequence of developing diabetes, because contrary to popular belief, this disease does not only affect blood sugar levels. Diabetes causes a metabolic disorder that affects blood circulation. Bruises appear, seemingly for no apparent reason, because the vessels become more fragile and brittle, and blood clotting worsens.
- Another reason for the appearance of bruises under the knee at the back, most often is a tendon sprain, varicose veins or internal arterial thrombosis.
- Also, if bruises appear on their own, seemingly for no apparent reason, this may be a reaction to the use of analgesics, antidepressants and anti-inflammatory drugs. The fact is that the components of these drugs reduce blood viscosity, which in turn leads to the appearance of hematomas.
You should start by diagnosing the causes, for which you should visit a phlebologist to rule out problems with the blood. If many small bruises appear on the body, we are talking about a blood disease. By taking tests, the number of platelets in the blood is determined and if a deficiency is detected, appropriate treatment is prescribed. If everything is normal according to hematology, you cannot do without examining the blood vessels to find out why bruises often appear on the body and legs: on the foot, on the inside of the thigh, on the knees, on the calves.
As preventive measures, it is advisable (even in the absence of problems with blood vessels) to wear comfortable shoes, dose physical activity, avoiding stagnation on the one hand, but also without straining it excessively, on the other, adjusting the diet. At the first signs of varicose veins, it would be a good idea to take special medications that strengthen the walls of blood vessels, but only a specialist can say about the advisability of taking them, as well as recommend a specific drug and its dosage. And then the problem that women often develop bruises on their legs for no reason will not bother you.
At the Antireflux phlebological center, our specialists will help you identify the true causes of bruises on your legs and body. After conducting the necessary tests and diagnostic studies, the necessary medications and treatment regimen will be selected according to the cause of the bruises.
Watch our video about why bruises can form for no reason:
Treatment of hematoma on the leg
Typically, a hematoma on the leg after a bruise is treated by two methods: conservative and surgical. The first category includes: cold and warm compresses, pressure bandages, taking analgesics, applying ointment, physiotherapeutic manipulations.
The second group involves performing a puncture - surgical removal of accumulated blood from the site of a bruise with the application of a suture and an aseptic bandage.
Treatment of a serious hematoma on the leg must be carried out under the guidance of a doctor; this will speed up the healing process and prevent unpleasant consequences.
Treatment
Modern treatment for the appearance of blue spots and formations of the lower extremities is complex. It involves the use of conservative therapy or surgical intervention, the choice of which is made after the causes of the pathological process have been diagnosed. Conservative therapy includes the use of various medications that improve the functional state of hemostasis, as well as the strength of the walls of venous vessels and microcirculatory structures. Surgical treatment is carried out to remove vessels with irreversible changes in their walls.
If blue spots appear systematically for no apparent reason, you should consult a phlebologist (a medical specialist who deals with the problems of vein diseases), who will prescribe additional research and appropriate treatment.
Symptoms
A bruise on the skin is always clearly visible. At first it has a purplish-blue color, and then begins to “bloom”, acquiring yellow and green colors. If a sufficiently large amount of blood accumulates under the skin, a protruding lump forms. At first it is very painful to feel, but later the pain goes away.
The outpouring of blood into the internal organs and into the substance of the brain is preceded by trauma. The main symptom is pain. In this case, the hematoma is not visible externally. If bleeding continues, the victim becomes pale, weak, and dizzy. With chronic internal bleeding, anemia comes to the fore. Bleeding in the brain is especially dangerous. Compression of brain structures may occur, sometimes leading to death.
Soft tissue hematomas
Soft tissue hematomas are divided into 3 types:
- Lungs - appear 24 hours after injury and are accompanied by mild pain. No special treatment is required.
- Medium - appear within 5-6 hours and are accompanied by pain and swelling. The motor function of the limb deteriorates. Consultation with a traumatologist is required.
- Heavy - formed within 2 hours after tissue damage. The function of the limb is impaired, acute pain and diffuse swelling are observed. You should immediately consult a doctor to determine a treatment strategy.
Immediately after the injury, swelling appears, and the skin acquires a purplish-bluish tint. After 5 days, the skin takes on a green tint as hemoglobin breaks down. Gradually, the hematoma resolves and “flows” down.
If there are no complications, the hematoma will resolve on its own. In the worst case, a hard area appears that causes discomfort and impairs motor function. When an intramuscular lump forms, external symptoms are rarely observed, but the limb swells significantly and an area forms inside, the touch of which causes severe pain.
Note! For chronic intramuscular hematomas, an MRI is prescribed to determine the location and extent of tissue damage.
When large lumps form, surgical intervention is required. Treatment is carried out by a traumatologist. The opening of infected seals is performed by a surgeon after a comprehensive diagnosis. The operation is performed on an outpatient basis, but for large hematomas hospitalization is required. An autopsy is performed, during which blood clots are removed and washing is carried out. Drainage and suturing are required. Sutures are not applied only for infected hematomas. Antibiotics are often prescribed in combination to eliminate the infection.
— What causes thrombocytopenia?
— The pathology in any case is caused by an imbalance between the formation of platelets and the rate of their decay. This is a condition when the bone marrow is either not sufficiently formed, or their amount in the circulating blood decreases.
It should be noted that in some cases, insufficient production of platelets in the bone marrow and rapid breakdown in the circulating blood occur simultaneously.
A decrease in platelet products is most often associated with bone marrow damage or metaplasia (degeneration), as well as the development of osteomyelofibrosis, which leads to a decrease in the number of megakaryocytes (giant cells of the bone marrow); Occurs in the following diseases or conditions:
- Aplastic anemia (when the body is unable to produce enough new blood cells);
- Myelodysplasia (a group of diseases in which we encounter malformed, dysfunctional blood cells);
- Leukemia and myeloma diseases;
- Radiation and toxic effects on the hematopoietic system.
Increased destruction of platelets occurs in the so-called thrombocytopenia of consumption (during DIC syndrome) and deposition (during hepatolienal syndrome, portal cirrhosis of the liver, Budd-Chiari syndrome), as well as some cardiovascular anomalies and diseases (aneurysm, defects, stenting).
It should be noted that immune thrombocytopenia occurs most often, when the rapid breakdown of platelets is associated with the destruction of the immune system. This group includes primary immune thrombocytopenia (idiopathic thrombocytopenic purpura), a disease when the immune system, due to the destruction of the immune system, produces antibodies against its own platelets.
The secondary immune form develops when immune complexes are produced during other autoimmune diseases (systemic lupus erythematosus, antiphospholipid syndrome, lymphoproliferative diseases), as well as during non-autoimmune diseases (gestational thrombocytopenia, infectious diseases, viral infections, including the chronic type) .
Contributing factors:
- Infections (especially viral);
- Pregnancy;
- Surgical intervention;
- Strong physical activity;
- Vaccination.
Intracranial hematomas
Intracranial hematomas are divided into the following types:
- Epidural.
- Subdural.
- Intracerebral.
- Intraventricular.
Epidurals appear in 1-3% of cases and are due to injury to the middle meningeal artery. Pathology is often observed with skull fractures or depressed fractures. A hematoma develops in 2-3 hours or within 24 hours. Lack of treatment leads to coma. The first symptoms are confusion and weakness. Children rarely lose consciousness after a severe blow. Significant swelling of the brain does not lead to the detection of a light gap (which is rare in adults).
Subdurals appear in 1-7% of cases and pose a threat to human life, since death occurs in 60% of cases. There is an acute, subacute and chronic form of the pathology. Bleeding occurs due to a rupture of a vein or artery in the damaged area. People report nausea and severe headaches. Symptoms characteristic of compression of the brain stem are often observed. Lack of treatment and worsening symptoms lead to coma.
Intracerebral are observed extremely rarely with severe traumatic brain injuries. The light gap is not visible, the development of pathology occurs quickly. Hemiplegia or hemiparesis often occurs, as well as extrapyramidal symptoms.
Intraventricular diseases are rarely diagnosed due to the serious condition of patients. There are acute disturbances of consciousness, an increase in body temperature, a decrease in heart rate, and an increase in blood pressure. To establish a diagnosis, a survey of close people is carried out, since the patient is unconscious. To establish the location of the hematoma, MRI is used. In the most severe cases, lombal puncture is used.
Pediatrician appointment prices:
| TYPES OF MEDICAL SERVICES | Cost, rub. |
| Examination of a child by a pediatrician to obtain a certificate + certificate | 1950 |
| Visit of a pediatrician, consultation at home (Moscow) | 5400 |
| Consultation with a pediatrician at home for the second child | 1950 |
| Patronage for a newborn / gymnastics and swimming at home (1 session, pediatrician Kapina A.V.) | 6300 |
First aid for bruises
To provide proper first aid, it is necessary to provide a home and camp first aid kit with special means. First of all, it is important to relieve the severity of inflammation. To do this, you need to provoke a spasm of damaged blood vessels. The cold can do this, so the essential items in the first aid kit are:
- hypothermic package;
- elastic bandage for organizing a pressure bandage;
- bruise remedies for topical use.
As a last resort, non-steroidal anti-inflammatory drugs can be used, a single oral dose of which can reduce the severity of pain.
The hypothermic bag is a soft polyethylene package with two circuits containing reagents isolated from each other. In order for the package to be able to cool damaged human tissues, it is necessary to destroy the internal partition between the reagents with a blow from the back of the hand and shake the contents well. You can buy such a package at any pharmacy. The product is not in short supply, so it is always in stock. The cost of the hypothermic package is low. You can inexpensively fill your home and travel first aid kits with an important component in order to promptly provide first aid to a bruised victim.
An elastic bandage should also always be in the first aid kit, since after cooling and mobilizing the bruised area, it is necessary to apply a tight pressure bandage, which will become another mechanism that stops hemorrhage, and therefore the severity of the hematoma.
Signs of bruise
A bruise is a closed injury, the presence of which can be judged with confidence only after some time has passed. If a cut, abrasion or bite is immediately visible - bleeding appears or ichor appears, then the bruise may not show itself in the first minutes or even hours. The first signs of a bruise are:
- pain at the site of injury;
- when you try to move, the bruised area hurts more;
- tissue swelling appears;
- the skin at the site of the bruise changes its color - it takes on a shade from red to purple.
The color of the bruised area is affected by the degree of subcutaneous hemorrhage. The greater the number of vessels that are damaged, the more pronounced the hematoma. Tears in muscle fibers cause the most pronounced swelling and pain. At the same time, it is important to remember that the larger the damaged vessel, the more pronounced it will be manifested by subcutaneous hemorrhages.
Classification of hematomas
In modern medicine, when classifying hematomas, the following are taken into account:
- Relation to the vessel - pulsating and non-pulsating hematomas.
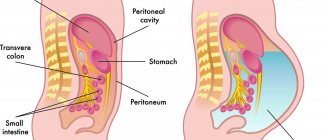
- Localization - in the cranial cavity, internal organs, under the skin or mucous membrane.
- The state of the blood in the affected area is suppurated, clotted, fresh, infected.
- Symptoms – limited, encysted, diffuse.
There are hematomas that do not fall into this classification. For example, intracerebral, intracranial, intraventricular. They are of the epidural or subdural type and cause serious complications.