Amyotrophic lateral sclerosis - symptoms and treatment
Amyotrophic lateral sclerosis ( ALS ) is a steadily progressive disease characterized by the death (degeneration) of motor neurons, which leads to impaired muscle movement, including respiratory muscles, up to paralysis and muscle wasting.
To understand the essence of the disease, it is necessary to touch upon the structure and functions of the brain and spinal cord. In the structure of the spinal cord along its entire length and partially in the brain stem, there are cells that send nerve impulses directly to the muscle fibers. They are called lower motor neurons , since their impulses set the muscles in motion. Grouped in the anterior part of the transverse section of the spinal cord, the lower motor neurons form the so-called “anterior horn”.
The spinal cord also functions as a connecting nerve “cable” between the brain and parts of the body. Normally, the spinal cord is subordinate to the brain. This means that if an impulse from the brain tells the muscle to raise the arm, and an impulse from the spinal cord tells it to lower, the arm will rise.
The brain has a complex structure, but in this article we need to pay attention to upper motor neurons . They are grouped in the area that responds to the initial generation of motor impulses in the body - the cerebral cortex and the brain stem. The impulses, in turn, travel down the spinal cord to the aforementioned lower motor neurons, and from there to the muscles, causing them to move. It is this pathway that is affected in amyotrophic lateral sclerosis.
ALS was first described in 1869. In the literature you can find the following synonyms for ALS: motor neuron disease, motor neuron disease, Charcot's disease (named after the pioneering doctor, although this disease was discovered by Charles Bell [1]), Lou Gehrig's disease (named after the famous baseball player who died of ALS in 1938 ). Many people now call it Stephen Hawking's disease because he lived with ALS for over 50 years.
Amyotrophic lateral sclerosis is a representative of the group of motor neuron diseases, i.e. diseases of the motor neurons. In addition to ALS, this group includes: primary lateral sclerosis, progressive muscular atrophy and progressive bulbar palsy.
Scientists have identified two causes of ALS : 90-95% are a sporadic cause (in other words, an accident) and 5-10% are a genetically inherited mutation [2].
Over the course of many years of research, non-genetic modifiable lifestyle factors have been found that predispose to ALS :
- Cigarette smoking is the most consistent nongenetic risk factor for ALS [8].
- Contact with agricultural fertilizers: pesticides, herbicides, insecticides and formaldehyde [8]. It is worth mentioning that formaldehyde is found in tobacco smoke in everyday life, so passive smoking should also be avoided.
- Lead released into the environment during professional activities, for example, when welding metals [10].
- Microtraumas of the head in professional sports [9]. This means that Lou Gehring, being a baseball player, probably caused ALS and early death 2 years later through his profession.
To summarize the above, ALS develops as a result of the combined influence of genes, environmental factors and lifestyle factors. This gene-time-environment model suggests that the development of ALS is a multistep process in which genetic defects are only one of several steps that ultimately lead to ALS.
There are approximately 10-12 thousand patients with ALS in our country. The disease is more common in men than in women (1.5 times), and the age range is from 20 to 80 years. The rate of its progression is directly proportional to age. The presence of a genetic mutation (in 5-10% of cases) also increases the rate of development of severe symptoms [14].
What is motor neuron disease
Motor neuron disease (MND) is a progressive neurodegenerative disease that affects motor neurons in the brain and spinal cord. The gradual death of cells in the nervous system leads to steadily increasing muscle weakness, affecting all muscle groups.
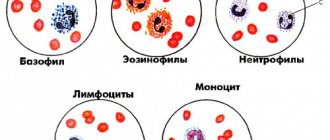
Motor neurons
The brain neurons that control movement (upper motor neurons) are located in the cerebral cortex. Their processes (axons) descend into the spinal cord, where they contact the spinal cord neuron. This contact is called a synapse. In the area of the synapse, a brain neuron releases a chemical substance (transmitter) from its process, which transmits a signal to a spinal cord neuron.
Spinal cord neurons (lower motor neurons) are located in the lower parts of the brain (bulbar) and in the cervical, thoracic, or lumbar spinal cord, depending on which muscles they send their signals to. These signals travel along the spinal cord neuron processes (axons) to the muscles and control their contractions. Bulbar neurons are responsible for contracting muscles associated with speech, chewing, and swallowing; cervical spine - for contraction of the diaphragm, arm movements; thoracic region - for body movements; lumbar region - for leg movements.
Manifestations of motor neuron damage
- When neurons in the spinal cord are damaged, muscle weakness increases, muscles lose weight (atrophy), and involuntary twitching (fasciculations) appears in them. Fasciculations don't just feel like twitching, they can also be seen. This is similar to subcutaneous muscle fluttering.
- If the neurons of the brain are affected, the muscles become weak, but at the same time stiffness (spasticity) appears, that is, muscle tone increases and it becomes difficult to relax.
- When neurons in the brain and spinal cord are simultaneously damaged, these signs can occur in different combinations. That is, muscle weakness can be accompanied by both fasciculations and muscle loss, as well as stiffness.
- Depending on which parts of the brain and spinal cord are affected, these signs may appear in the muscles responsible for the movements of the arms, legs, breathing or swallowing.
4.Treatment
To date, only one drug has been synthesized, rilutek/riluzole, that can at least briefly slow down the progression of amyotrophic lateral sclerosis. The main role is still played by adequate palliative therapy, aimed at mitigating the symptoms that dominate in a particular case. However, the very fact of the introduction of Rilutek into clinical practice (1995) is of fundamental importance. The appearance of a drug with a weak, but proven and confirmed effect indicates that ALS can, in principle, be excluded (and therefore will be excluded in the foreseeable future!) from the list of incurable diseases.
What should you be wary of?
It is extremely important to identify the diagnosis as early as possible, as this gives a greater chance of preserving a person’s functionality longer, prescribing treatment correctly and avoiding complications. Look out for persistent symptoms that last for weeks or months. Particular attention should be paid to symptoms that relate to changes in muscle strength:
- awkwardness of movements;
- weakness;
- weight loss;
- difficulty performing normal activities.
For example, a person begins to hold the key incorrectly, it is difficult for him to open the door, the pen falls out of his hands when writing, his handwriting has changed, it is difficult to write letters, his foot slips or his sock catches when walking, complaints about “mess in the mouth.” Such conditions may be accompanied (or preceded) by cramps in the limbs or muscle twitching (fasciculations), especially at night.
It is important to pay attention to motor deficits that persist for weeks or months, changes in gait, weakness in the limbs, changes in speech, wasting, most often of the hands, as well as the patient’s accompanying weight loss and the appearance of increased fatigue.
3. Symptoms, diagnosis
The clinical picture of ALS is determined by the predominant localization of the atrophic process and is often specific for several similar processes at once, which significantly complicates diagnosis. In most cases, in the initial stage there is muscle weakness, spastic twitching, and disorders of visual-motor coordination; in approximately a quarter of patients where the medulla oblongata is affected by neurodegeneration, the so-called bulbar symptoms - disturbances in the articulatory components of speech, swallowing, palatal, chewing, and respiratory reflexes.
Muscle atrophy gradually progresses, leading to complete motor inability, severe depressive disorders (intelligence does not suffer), inability to feed independently, and respiratory failure. The course and development of ALS quickly disables patients who, in the later stages, require total care, artificial feeding and mechanical ventilation (artificial ventilation). The process ends fatally, usually 4-6 years after the onset of manifest symptoms. Cases of stabilization and arrest of motor neuron degeneration in Stephen Hawking, as well as in virtuoso guitarist Jason Becker - where the diagnosis of ALS is beyond doubt - to date remain an inexplicable casuistry.
Methods for unambiguous instrumental and/or laboratory diagnostics have not yet been developed (even tomographic methodology is uninformative and has only auxiliary value). At the same time, it is necessary to differentiate clinically (according to anamnesis, complaints, state dynamics, reflexological examination data) from a number of etiologically related processes - which can be done at the stage of formation of a pathognomonic (inherent only to ALS) symptom complex.
Motor neuron disease as an independent process should be distinguished from motor neuron syndrome, which accompanies some other diseases (for example, tick-borne encephalitis).
About our clinic Chistye Prudy metro station Medintercom page!
Course of the disease
The disease is progressive. Muscle weakness increases and spreads to different regions of the muscles of the limbs, trunk, bulbar and respiratory muscles. One of the most vulnerable forms is bulbar (patients suffer from speech impairment). People note that it has become more difficult for them to sing, they cannot sing notes, and they pronounce words poorly. Someone notices that speech has become slower, its sonority has changed, and a nasal tone has appeared. The bulbar form is dangerous because in addition to changes in speech, swallowing disorders quickly occur. In this situation, in order to ensure normal nutrition for the patient and prevent aspiration (entry into the respiratory tract when inhaling liquid or solid substances), it is necessary to carefully select the diet.
2. Reasons
In the world's research centers, the etiopathogenesis of neurodegenerative diseases is being studied very intensively. Regarding ALS, more and more specialists are inclined to the point of view according to which this disease is actually a group of etiologically heterogeneous processes with the only common factor - damage and death of motor neurons of the brain and/or spinal cord. Thus, a hereditary nature is detected only in 5-10% of cases (the exception is the clearly familial form of the disease on the island of Guam). The metabolic (metabolic), autoimmune, and especially broadly viral hypothesis is also discussed, in which ALS is considered as a slow neuroinfection.
To date, no reliable risk factors that can promote or provoke the onset of motor neuron degeneration have been identified.
Visit our Neurology page