Atherosclerosis is a pathological process in blood vessels that is chronic. Danger of atherosclerosis: over time, this disease causes serious circulatory problems. There is a disruption in both fat and protein metabolism in the human body.
Atherosclerosis must be treated without fail, otherwise it can lead to such serious diseases as heart attack, stroke, aortic aneurysm, coronary heart disease, cerebral ischemia, inflammatory processes in the gastrointestinal tract, renal failure and others.
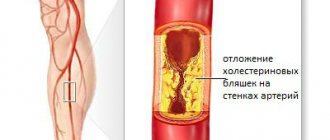
The disease process is as follows:
- There is a violation of fat/protein metabolism. There is an increased amount of lipids in the blood.
- “Excess” amounts of lipids remain on the walls of the arteries.
- After this, overgrowth with fibrous tissue occurs.
- The vessel narrows and ceases to supply the organs and tissues with blood in the required volume.
This disease is mostly related to age: most often it affects men - 40-60 years old, women - 50+ years old. However, there is an alarming trend in the number of sick people and the age under 40 years of age. This is largely caused by improper and unbalanced nutrition and the worsening environmental situation.
Atherosclerosis “strikes” the arteries, including the aorta, carotid arteries, arteries of the brain, and heart. For this reason, this disease is one of the most common causes of myocardial infarction and coronary heart disease, stroke, and circulatory problems.
Types of atherosclerosis
There are different types of atherosclerosis. The classification of the disease is based on the site of origin of the process and, accordingly, on which organ receives insufficient blood circulation. The following types of atherosclerosis are distinguished:
- heart vessels (coronary atherosclerosis);
- cerebral vessels (cerebral atherosclerosis);
- aorta (in the abdominal/thoracic cavity);
- renal arteries;
- arteries of the lower extremities;
- arteries of the upper extremities;
- atherosclerosis of the penile arteries.
Treatment of renal artery stenosis
Until recently, when there was stenosis of the renal arteries, the organ was removed. Now there are effective treatment methods (both surgical and conservative).
With drug therapy, the choice of drugs depends on the stage of the disease. The doctor may prescribe diuretics, antihypertensive drugs, anticoagulants, statins, fibrinolytics, ACE inhibitors and angiotensin receptor blockers.
Changing your lifestyle is important - quitting smoking and drinking alcohol, following a low-carbohydrate diet, losing excess weight.
In difficult cases, surgery is indicated:
- endarterectomy – blood clot is removed;
- angioplasty - dilates the artery using a balloon;
- stenting - a stent is placed inside the vessel to expand and strengthen the walls;
- shunting - with the help of shunts they create a bypass for blood;
- prosthetics – part of the renal artery is removed and replaced with a prosthesis;
- nephrectomy – kidney resection.
Primary appointment (examination, consultation) with a cardiovascular surgeon
1850 rub.
Sign up
Stages (stages) of disease development (pathogenesis of atherosclerosis).
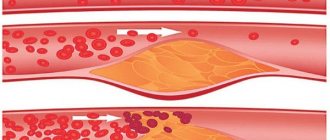
Fat streak stage.
Small lipid spots (only one or two millimeters) are immediately present on the walls of the vessel. Then they grow and “unite” with each other. Macrophages destroy them and transform into foam cells, from which fatty stripes appear. This is a normal process, the presence of which does not in any way indicate that a person may develop atherosclerosis in the future.
Stage of fibrous plaques.
The growth of connective tissue develops from fatty stripes, from which fibrous plaques are subsequently “born”. Initially, they are not solid and can be dissolved - with early detection and assistance provided to the patient. Later, fibrous plaques harden as calcium salts are deposited in them.
Stage of complex disorders.
The next stage is a violation of the integrity of fibrous plaques: cracks and tears appear on them. Platelets attach to such a plaque, causing partial or complete blockage of the vessel.
General information
Atherosclerosis is a chronic focal lesion of the arteries on which atherosclerotic plaques have formed.
They block the lumen of the arteries, resulting in a chronic, slowly increasing insufficiency of blood supply to the organs. In most cases, it is atherosclerosis that serves as the impetus for the development of various cardiovascular pathologies - ischemia, heart attack, stroke, heart failure, impaired blood flow in the extremities, etc. In 1904, the German scientist Marchand first introduced the term “atherosclerosis”, 10 years later in his It was substantiated by experimental studies by the Russian scientist Anichkov. The second name of the pathology is Marshan-Anichkov disease.
General urine analysis in Moscow from 1 weekday
from 340 ₽
Sign up
Homocysteine in Moscow from 1 weekday
from 1100 ₽
Sign up
Complete blood count (CBC/Diff - 5 fractions of leukocytes) in Moscow from 1 weekday
from 290 ₽
Sign up
Experts identify the following stages of development of atherosclerosis:
- Initial - the formation of fatty deposits on the walls of blood vessels. Symptoms at this stage are usually absent, which makes early diagnosis of the disease difficult. But at the same time, changes begin in the structure of the artery walls. The risk of rapid development of the following stages increases with excess body weight and diabetes.
- The second is the compaction of fat deposits. The vessels become inflamed, lipid deposits take the form of capsules and clog part of the lumen.
- The third is the development of complications. The arteries become clogged, blood clots form, and atherosclerotic plaques may rupture. This can give rise to limb necrosis or myocardial infarction.
Depending on the cause of development, atherosclerosis is classified as follows:
- Metabolic - hereditary factor, as well as diseases of the endocrine system, failure of fat metabolism.
- Hemodynamic - pathologies of the cardiovascular system, for example, arterial hypertension.
- Mixed - develops as a result of a combination of different factors.
Classification of atherosclerosis according to the degree of development activity:
- Progressive - new atherosclerotic plaques are constantly being formed, and existing ones are actively growing. Vivid signs of the disease appear, and there is a high risk of complications.
- Stabilized - lipid deposits form slowly, symptoms decrease or remain unchanged. The likelihood of negative consequences is low.
- Regressive - clinical signs weaken, tests and the general condition of the patient improve.
Symptoms of atherosclerosis
The first period of atherosclerosis is the preclinical (asymptomatic) period. During this period, the disease does not make itself known in any way, while a high (exceeding the norm) amount of β-lipoproteins or cholesterol is detected in the human blood. Clinical manifestations occur only after the vessel becomes 50% narrower (or more). The symptoms of this disease depend on which artery or aorta is affected.
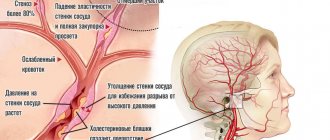
Atherosclerosis of cerebral vessels.
Symptoms:
deteriorated memory function, low poor performance, sleep problems, dizziness. As it progresses, the patient’s psyche becomes impaired. The following complications may also make themselves felt: thrombosis and hemorrhage.
Atherosclerosis of the heart vessels (coronary vessels).
Symptoms:
myocardial infarction, cardiosclerosis, angina pectoris.
Atherosclerosis of the thoracic aorta.
Symptoms:
severe pain behind the sternum, radiating to the upper abdomen or back and arm. Duration: the continuation of such pain occurs from a couple of hours and even up to several days.
Atherosclerosis of the abdominal aorta.
Symptoms:
constipation, flatulence, pain in the abdominal area; in addition, numbness of the legs and swelling of the feet may occur.
Atherosclerosis of the renal arteries.
Symptoms:
unilateral damage - gradual development and intensification of hypertension with constantly high blood pressure numbers; bilateral damage - arterial hypertension. Low back pain may also be present.
Atherosclerosis of the arteries of the lower extremities.
Symptoms:
pain in the calves or a feeling of weakness in them, a feeling of numbness in the legs.
Atherosclerosis of the penile arteries.
Symptoms:
erection problems, impotence.
Symptoms of renal artery stenosis
Stenosis is accompanied by:
- dizziness;
- pain in the lower back and abdomen;
- decreased urination or complete absence of urine;
- blood inclusions in the urine;
- rapid heartbeat;
- shortness of breath;
- muscle weakness;
- swelling of the legs;
- nausea, vomiting;
- fever;
- the appearance of “flies” before the eyes;
- sleep disturbance;
- memory impairment;
- emotional instability.
Due to the narrowing of the lumen, blood flows to the cells in insufficient quantities, which causes filtration to worsen, blood pressure to increase, kidney and heart failure to develop, and edema to form in the lungs. If left untreated, the kidney shrinks and ceases to perform its functions.
How is atherosclerosis treated, what options exist?
For atherosclerosis, treatment is carried out comprehensively. A person must adhere to a diet. The diet is drawn up by a doctor, limiting fatty foods (primarily animal fats), simple carbohydrates and salt, and the person must also give up bad habits - smoking and drinking alcohol, and perform light physical activity (therapeutic exercises). In addition, the patient begins taking a course of medications, the task of which is to remove excess cholesterol from the human body, as well as aimed at reducing the activity of the body’s “production” function of cholesterol. If the above steps do not work, as well as in the case of a high probability of arterial blockage, then the patient is prescribed surgical intervention.
Unfortunately, atherosclerosis is an irreversible disease and it is completely impossible to cure it.
Causes of the disease
Non-modifiable factors for the occurrence of atherosclerosis include the following:
- Genetic predisposition. The disease more often occurs in those whose loved ones suffer from this disease.
- Age-related changes. After 45–50 years, atherosclerotic vascular pathologies occur in most people.
- Floor. The disease appears in men 10 years earlier than in women, and by the age of 50–55 the incidence statistics among both sexes level out. This is associated with a decrease in estrogen production in women during menopause.
Factors that can be influenced by the person himself:
- Poor nutrition. Excessive consumption of animal fats leads to changes in the arteries.
- Smoking. Extremely harmful to blood vessels. A long history of smoking has a direct impact on the development of hyperlipidemia and atherosclerosis.
- Sedentary lifestyle. Physical inactivity entails a violation of fat metabolism, which can serve as a trigger for the development of serious pathologies, including vascular atherosclerosis.
Potential causes of atherosclerosis also include:
- arterial hypertension;
- dyslipidemia;
- diabetes mellitus and overweight. The disturbance of fat metabolism that occurs in these pathologies is the direct cause of atherosclerosis.
Prevention of atherosclerosis
A healthy lifestyle is the main way to prevent atherosclerosis. Only a nutritious and balanced diet, sufficient physical activity, and giving up bad habits will have a positive effect on the condition of blood vessels. In addition, a mandatory method of prevention (or at least identifying the disease at an early stage) is to pay attention to your health: preventive examinations by doctors and taking a cholesterol test. If you have hypertension, you must constantly monitor your blood pressure and take the necessary medications; if you have diabetes, maintain normal blood sugar levels.
Watch your health and remember that a healthy lifestyle is necessary for everyone!
Diagnostics
To diagnose atherosclerosis, both laboratory and instrumental methods can be used:
- general blood analysis;
- blood cholesterol level test;
- angiography (injection of a contrast agent into the blood, which reflects X-ray radiation and gives the specialist a detailed map of the condition of the vessels of the entire body);
- CT, MRI;
- coronary angiography (to study the coronary arteries);
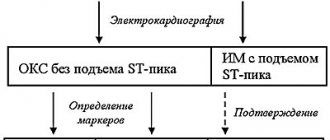
- ECG, echocardiography (echocardiography);
- Holter ECG monitoring (to detect disturbances in heart rhythms);
- Ultrasound (to study the condition of the aorta, kidney vessels, heart).
Diagnostics usually does not cause problems for an experienced doctor - for this, our center has all the necessary equipment. After all, modern high-tech devices will be required - the better the equipment, the more detailed the examination data will be, which will help the doctor choose the optimal treatment method.
Cholesterol is not your enemy!
There are already many publications in foreign scientific literature about the role of the lymphatic system in the development of atherosclerosis (the formation of plaques in the arteries).
The lymphatic system is involved in the regulation of the immune response, inflammation and reverse cholesterol transport. Researchers show that what is responsible for the uncontrolled formation of plaque is not so much low-density lipoproteins, which everyone is up in arms against (from ordinary people and YouTube bloggers to nutritionists and even doctors), but rather the inability of the lymphatic system to remove the consequences of the attack on cholesterol by inflammatory cells.
“In other words, atherosclerosis is a problem of the immune system, the lymphatic system, and only then cholesterol,” explains Nadezhda Aleksandrovna Garyaeva, doctor of medical sciences, professor, lymphologist. Indeed, it makes sense to review the diet for hereditary hypercholesterolemia, but this does not mean that cholesterol itself is harmful.
High levels of total cholesterol and LDL in the blood are indeed a prognostic sign of the development of atherosclerosis. However, the disease does not develop due to cholesterol, but due to a decrease in the function of the lymphatic system against the background of the inflammatory reaction of the immune system to damage in the blood vessels, and cholesterol in this case is the target of attack by immune cells.
Cholesterol is an essential building material in the human body. It is used for the construction of cell membranes, the formation of sex hormones, and the secretion of bile acids. A large amount of cholesterol is contained in the myelin sheath of nerve fibers. Even in the process of Vitamin D synthase, one of the precursors is cholesterol. You can imagine the long-term consequences of artificially blocking cholesterol synthesis in the body. By the way, most of it is synthesized in the liver, and does not enter the body with food.
That is why the world is already discussing the ideas of pharmacological and even genetic correction of lymphangiogenesis - the process of formation of lymphatic vessels in the artery wall. A Russian clinic has developed and patented another approach - enhancing the function of the lymphatic system using lymphotropic injections of official (can be bought at the pharmacy) medications.
In modern medical education, the lymphatic system occupies an insignificant place, which is why in general medical practice you will never be offered what you will find in this article. Moreover, there are heads of universities who still believe that the lymphatic system is not worth any attention.
In this article, we were not only able to briefly and clearly summarize modern knowledge about atherosclerosis, but also revealed the approach of the Lymphatek Clinic to the pathogenetic (affects the mechanisms) treatment of atherosclerosis without the use of cholesterol-binding drugs (statins).
Surgical methods for treating atherosclerosis
- elimination of atherosclerotic plaque by open surgery on the vessel,
- expansion of the lumen of the vessel from the inside using special instruments and installation of a metal frame that prevents further narrowing,
- when the lumen of the vessel is completely closed by a plaque, a bypass operation is performed (a bypass of the blood flow).
Surgical treatment is prescribed when the risk of developing disabling complications without surgery exceeds the development of such complications after surgery.
Publications in the media
Atherosclerosis of the coronary arteries with their hemodynamically significant stenosis leads to the emergence of various clinical variants of coronary heart disease (see Coronary heart disease) • In addition to atherosclerosis (more than 90% of cases of coronary artery disease), coronary artery disease can be caused by arteritis, collagenosis, thrombosis and embolism, anomalies in the development of coronary vessels and etc.
Frequency - see Coronary heart disease.
The etiology in most cases is unknown • The main role, apparently, belongs to various disorders of lipid metabolism (see Hyperlipidemia), detected in almost all patients with coronary artery disease • In some cases, atheromatosis is accompanied by diffuse distal sclerosis of the coronary arteries without local lipid infiltration of their wall (X- syndrome).
Pathophysiology • The heart requires 0.1–0.2 ml of oxygen per 1 g of weight per minute. Such intense gas exchange is possible due to the high perfusion pressure in the coronary arteries arising directly from the aortic ostium, the high inflow volume of 5% of the bcc, and the increased extraction of oxygen by the myocardium (more than 75% at rest and almost 100% at maximum load) • With stenosis of the coronary arteries of less than 70–75% of their lumen, disturbances in myocardial perfusion occur only during exercise, and at rest the decrease in perfusion does not exceed 5% of normal values • Even with complete occlusion of one of the main coronary arteries, the level of perfusion of the “compromised” myocardial zone is reduced by only 50 % due to collateral circulation • With hemodynamically significant stenoses of several coronary arteries, the dependence of impaired myocardial perfusion at rest on the degree of stenosis is almost linear, therefore multi-vessel damage is always associated with a worse prognosis • As a rule, even in the area of the previous infarction, a certain amount of viable myocardium remains (see . Heart disease is ischemic), therefore revascularization interventions improve the contractile function of the heart even in the area of infarction • When assessing the degree of damage to the coronary bed by atherosclerosis and choosing tactics, the following classification is used.
Classification of atherosclerosis of the coronary arteries (Petrosyan-Zingerman) • Anatomical type of blood supply to the heart •• Predominantly left (about 10%) •• Predominantly right (85–90%) •• Balanced (about 5%) • Localization of the lesion •• Trunk of the left coronary artery (CA) •• Anterior interventricular branch •• Circumflex branch •• Diagonal branch •• Right CA •• Blunt edge branch •• Other arteries • Extension of lesion •• Local stenosis •• Diffuse stenosis • Localization of stenoses •• Proximal segment of artery •• Middle segment of the artery •• Distal segment of the artery • Degree of luminal stenosis •• Without stenosis •• Moderate (less than 50%) •• Severe (less than 75%) •• Severe (from 75% to subtotal stenosis) •• Occlusion • Collateral blood flow • • Anastomoses between the anterior interventricular and circumflex branches •• Anastomoses between the circumflex branch and the right coronary artery •• Anastomoses of the circle of Viessen-Tebezia •• Other anastomoses.
Clinical picture and diagnosis.
• Complaints and objective examination - see Coronary heart disease.
• Instrumental methods •• ECG, chest x-ray, echocardiography, radioisotope study, stress tests - see Ischemic heart disease •• Intravascular ultrasound of the coronary arteries ••• Indications: •••• stenting of narrow coronary arteries; •••• restenosis after stent implantation; •••• unsatisfactory results of percutaneous transluminal coronary angioplasty; •••• questionable stenoses, especially of the trunk of the left coronary artery; •••• stenosis and implantation of stents in the mouths of arteries; •••• the need to assess the extent of stenosis and vessel diameter before endovascular interventions; •••• additional indications are under development ••• Methodology •••• Determine the cross-sectional areas of the coronary artery, the degree of stenosis, the transverse area of the residual lumen in the area of maximum stenosis, the length and eccentricity index of the plaque •••• If three-dimensional reconstruction is possible determine the volume of the plaque and its structure throughout •••• A study in color Doppler mapping mode is carried out when there are difficulties in interpreting the area of the lumen of the vessel that arise in the area of lipid plaques with a thin cap, and during coronary artery stenting, when measurements of the coronary artery lumen in the area of implantation can be significant influence further tactics •• Ultrasound of coronary bypass grafts ••• Indications •••• Transthoracic ultrasound of pedicle coronary bypass grafts is performed for all patients in the immediate period after coronary bypass surgery •••• Intravascular ultrasound of coronary bypass grafts is performed for endovascular correction of coronary bypass graft stenoses in the postoperative period •••• Additional indications are under development ••• Technique •••• Transthoracic ultrasound of pedicled mammarocoronary bypass grafts, pedicled coronary artery bypass grafts from the gastroepiploic artery, as well as intravascular ultrasound of coronary bypass grafts are feasible in almost all patients ••• • Transesophageal and transthoracic ultrasound of autovenous coronary artery bypass grafts appear to be futile •••• Transesophageal and transthoracic ultrasound of autoarterial coronary artery bypass grafts is under development •• Ultrasound of arteries and veins used as coronary artery bypass grafts ••• Performed in all patients before coronary artery bypass grafting ••• Determine the presence of the corresponding arteries, their diameter, length, their possible stenosis in case of damage by atherosclerosis or other pathological processes, anomalies in the development of arteries, volumetric blood flow in them ••• When using saphenous veins of the lower extremities as coronary bypasses, diagnose varicose veins ••• When using internal mammary arteries as shunts, ultrasound of the subclavian arteries is also performed ••• When ultrasound of the radial and ulnar arteries is performed, the Allen compression test is performed to determine the anatomical type of blood supply to the hand •• X-ray contrast selective coronary angiography ••• Indications: performed on all patients, initially admitted with a diagnosis of myocardial infarction, who have suffered acute coronary events, with clinical symptoms in patients with chronic forms of coronary artery disease, as well as with positive results of stress testing ••• Methodology •••• Typically, radiopaque selective coronary angiography is performed from a transfemoral approach, but with severe atherosclerosis of the femoral arteries, it can be performed from other approaches •••• In most cardiological centers, catheterization of the coronary arteries is carried out using the Judkins controlled catheter technique •••• The study reveals the indicators indicated in the heading Classification of atherosclerosis of the coronary arteries •••• When planning endovascular treatment, except assessment of the localization and degree of stenosis of the coronary artery, the presence, severity of calcification and angioarchitecture of the coronary arteries (in particular, tortuosity of the artery, lateral branches, etc.) are important in the area of possible transcatheter correction •••• When planning coronary bypass surgery, information about the structural and morphological features is obtained coronary artery distal to the stenosis, where a coronary bypass can be applied, as well as the functioning of collateral circulation in the area of impaired myocardial vascularization.
TREATMENT
Drug therapy - see Coronary heart disease.
Surgery.
• Indications: in general, the indications are determined by the anatomical type of coronary atherosclerosis, left ventricular function and, to a much lesser extent, the clinical picture of the disease.
• General indications for endovascular treatment •• One- or two-vessel coronary artery disease with stenosis or occlusion of type A or B according to the classification given below •• The introduction of new methods of endovascular treatment (stenting, laser revascularization) allows interventions in some cases with type stenosis WITH.
• Angiographic characteristics of stenoses by type •• Type A (minimal complex) ••• Local (less than 10 mm) ••• Concentric ••• Easily passable ••• Non-curved segment (<45°) ••• Incomplete occlusion ••• No major branches in the area of stenosis ••• No thrombosis ••• Smooth contour ••• Little or no calcification •• Type B (medium complex) ••• Tubular (10–20 mm) ••• Eccentric ••• Slight tortuosity proximal segment ••• Slightly curved segment (45–90°) ••• Total occlusion less than 3 months ••• Stenosis at the bifurcation, requiring the use of two guidewires ••• Thrombosis ••• Irregular contour ••• Moderate or severe calcification •• Type C (severe complex) ••• Diffuse (more than 20 mm) ••• Eccentric ••• Marked tortuosity of the proximal segment ••• Very curved segment (>90°) ••• Total occlusion, existing for more than 3 months, with developed collaterals ••• Impossibility of bypassing all major branches in the area of stenosis ••• Thrombosis ••• Irregular contour ••• Severe calcification.
• Contraindications to endovascular treatment •• Absolute: end-stage circulatory failure •• Relative ••• Type C stenoses ••• Poor short-term prognosis for life due to concomitant diseases (for example, malignant neoplasms with distant metastasis) ••• Diffuse distal sclerosis coronary arteries (X-syndrome).
• Specific complications of endovascular treatment •• Perioperative MI due to dissection, intimal volvulus, spasm or thrombosis of the coronary artery •• Restenosis due to progression of atherosclerosis, arteritis or hyperplastic reaction in the area of stent implantation •• False aneurysms at the access site •• Adverse reactions associated with use contrast media.
• General indications for coronary artery bypass grafting •• Hemodynamically significant stenosis of the trunk of the left coronary artery •• Variant of the trunk lesion (stenosis of the anterior interventricular branch, circumflex branch, right coronary artery) •• Two-vessel and single-vessel lesion with hemodynamically significant proximal stenosis of the anterior interventricular branch •• Two-vessel lesion without proximal stenosis of the anterior interventricular branch with a decrease in the contractile function of the left ventricle, severe ischemia, tolerant to conservative treatment, and also when stenotic vessels supply blood to a large volume of viable myocardium •• MI during the course or relapse of MI, refractory to intensive conservative therapy •• MI accompanied by left ventricular insufficiency in the presence of coronary artery stenosis, providing blood supply to viable myocardium beyond the developed necrosis •• Coronary artery bypass grafting as a primary reperfusion strategy in the early stages (no later than 6–12 hours) MI with ST segment elevation •• One- or two-vessel lesion that caused the onset life-threatening ventricular arrhythmias, especially if the patient has undergone resuscitation for arrhythmic cardiac arrest or there is sustained ventricular tachycardia •• Failure of percutaneous transluminal coronary angioplasty with persistent ischemia threatening coronary artery occlusion involving a significant volume of myocardium in the risk area •• Foreign body in the coronary artery in a position that threatens cessation of blood flow •• Ischemia of viable myocardium, tolerant to drug and endovascular correction, outside the blood supply zone of a functioning mammarocoronary shunt to the anterior interventricular branch.
• Contraindications to coronary artery bypass grafting •• Absolute: end-stage circulatory failure •• Relative: diffuse distal sclerosis of the coronary arteries (X-syndrome); unfavorable short-term prognosis for life due to concomitant diseases (for example, malignant neoplasms with distant metastasis).
• Specific complications of coronary artery bypass surgery •• Perioperative MI •• Osteomyelitis of the sternum with flap isolation of both internal mammary arteries •• Ischemia of the hand after isolation of the radial artery with a predominantly radial type of blood supply to the hand.
Prognosis • Has a pronounced dependence on the anatomical variant of the lesion of the coronary arteries, left ventricular function, the presence of rhythm disturbances and concomitant pathology • Surgical treatment has little effect on the prognosis for life expectancy, with the exception of cases of three-vessel and stem lesions • Coronary artery bypass grafting has advantages over endovascular correction in in terms of quality of life, frequency of restenosis and the need for repeated interventions • Endovascular treatment has advantages over coronary artery bypass surgery in terms of the duration of hospital treatment, its cost (in Russia this is true only if intervention on one vessel is necessary).
Synonyms: Coronary heart disease, Coronary disease (heart).
Abbreviations • CA – coronary artery
ICD-10 • I25.1 Atherosclerotic heart disease
Treatment results
Depending on the initial localization of the process, already during the first course of treatment, the patient clinically notices the following improvements:
- Reducing noise in the head and headaches
- No pain when walking
- Disappearance of discomfort in the heart area during physical activity
The proposed treatment method is not generally accepted because it goes against the standards of the pharmaceutical industry. Currently, in general practice, the problem of atherosclerosis is dealt with therapeutically by cardiologists, and, if immediate surgical intervention is necessary, by vascular surgeons.
In addition, the treatment method requires in-depth knowledge of the morphology and physiology of the lymphatic system. Here, using the example of the treatment of lymphedema, we have already discussed why doctors in ordinary hospitals do not treat lymphedema.
Despite the fact that the first patient was treated 13 years ago (he managed to save his legs due to obliterating atherosclerosis of the vessels in the knee area), we still continue to accumulate statistical data and take a limited number of people for treatment. It is possible to come for treatment from another city. Treatment technologies are patented in the Russian Federation and can only be safely used at the Lymphatek Clinic. We select patients for whom treatment is indicated individually based on their application.
LEARN ABOUT TREATMENT POSSIBILITIES
You can learn more about the treatment process and some of the results in other blog articles. There are interesting videos with patient reviews and comments from leading doctors.
- Vascular atherosclerosis. Lymphologist's explanation.
- Atherosclerosis of leg vessels. Case of Yuri's treatment
- Atherosclerosis of the vessels of the neck and heart. Analysis of Valery's treatment.