In medical practice, blood pressure levels are divided into three groups.
- The first is low or reduced blood pressure. It is characterized by systolic numbers from 90 to 50 mm Hg to 60-40 and below divstolic.
- The second is a normal blood pressure level. This is the norm established by the World Health Organization, defined by the range from 120 to 140 per 70-90 mmHg.
- Finally, the third, high blood pressure or hypertension (not to be confused with hypertension, the first is a condition, the second is a disease of the cardiovascular system). The latter situation poses the greatest danger to the health and life of the patient, since the risk of serious complications increases significantly.
The indicated blood pressure level of 150/100 is pathological, but not always. It is necessary to take into account the so-called individual norm of the human body or working pressure (it can be no more than 10 mmHg from the norm).
Normal in some cases will be 150 to 100, and 145 to 95, and other variations within the mentioned figures.
Causes of a one-time jump in blood pressure levels
A one-time development of hypertension (an acute increase in upper and lower pressure) is somewhat less common. More often there is persistent hypertension, which is difficult to control with medications.
In what cases is it possible for a short-term increase in blood pressure to 150 to 100 or more in a healthy person?
- Consuming large amounts of table salt the day before. Sodium salts (in particular chloride) have the property of retaining fluid in the body.
As the concentration of water in the body increases, a generalized disturbance of hemodynamics (blood flow) occurs and the tonometer readings shift upward.
This can end not only in an increase in blood pressure to 150 to 100, but also in a hypertensive crisis, stroke, heart attack, and emergency conditions.
- Alcohol abuse. The misconception that alcohol lowers blood pressure has been entrenched in people's minds for a long time. But this is nothing more than a mistake.
In the first phase of alcohol intoxication, vasodilation is observed, which actually leads to a temporary decrease in blood pressure.
After about 15-30 minutes, the process is reversed: the pressure rises sharply due to a significant narrowing of the arterial structures. Hence the characteristic clinical picture.
Everything can end very badly: the same strokes, heart attacks. In addition, there is an increase in body temperature, which only aggravates the situation.
- Drinking large amounts of water the day before. It affects in a direct way. There is an increased load on the excretory system. The kidneys are partially responsible for regulating blood pressure levels. The result is a temporary increase in tonometer readings, sometimes to significant levels.
These causes of pressure 150 to 100 are relatively rare when compared with pathological factors.
Features of manifestations
The symptoms of symptomatic hypertension depend on the disease that caused the increase in tonometer values. The main symptom is a persistent increase in blood pressure, which is difficult to respond to drug therapy.
The following symptoms of the disease are distinguished:
- constant headache;
- noises in the head;
- pain in the occipital area;
- cardiopalmus;
- chest pain;
- flashing “flies” before the eyes;
- increasing weakness;
- swelling.
The absence of clinical manifestations entails gradual progression of the pathological process, which leads to damage to the functional activity of target organs.
[node:field_similarlink]
Causes of long-term persistent increase in blood pressure levels
There are many more factors for the development of persistent hypertension. More often, the increase in tonometer readings is caused by one or another pathology, that is, hypertension is secondary.
What diseases cause high blood pressure?
- Osteochondrosis of the cervical spine. It provokes a violation of cerebral circulation, sometimes significant. Certain areas of the cerebral structures responsible for regulating vascular tone do not receive enough nutrition. Hence the increase in blood pressure levels. The tonometer readings may vary depending on the intensity of the disorders.
- The course of primary or secondary hypercortisolism. In other words, a pathology associated with excessive production of cortisol by the adrenal glands.
This substance has a pronounced hypertensive (increasing blood pressure) effect and causes pressure of 152-156 to 112-115.
The development of the problem is possible with neoplastic processes (neoplasms) in the paired (thyroid) gland, tumors of the pituitary gland, and hypothalamus. Injuries of the chiasmatic-sellar region.
Hypercortisolism especially often develops as a result of Itsenko-Cushing's disease. When the pituitary gland produces too much corticotropin, which stimulates the synthesis of cortisol.
Such patients, as they say, fall apart before our eyes: the skeleton suffers, crumbling under its own weight, the reproductive system suffers, cardiovascular pathologies become commonplace.
Patients with the syndrome need to be treated comprehensively.
- Hyperthyroidism. Another endocrine disease. It develops as a result of excessive production of thyroid hormones: T3, T4 and pituitary hormone: TSH.
The disease is accompanied by characteristic symptoms, among which increased blood pressure is lost. Including a persistent rise in body temperature, exophthalmos, impaired neck relief, changes in sexual function, etc.
- Atherosclerosis. In other words, a blockage or sharp persistent narrowing of large blood vessels. It is more common in elderly and senile people, smokers, and people who abuse alcoholic beverages.
The process entails dangerous consequences for life and health: strokes, heart attacks, blood clots and acute tissue necrosis (primarily the lower extremities, which is well known to smokers) are possible.
- Systemic diseases such as diabetes. Another dangerous pathology that puts an end to the general health of an adult. Provokes severe damage to the cardiovascular system.
- Kidney diseases of various types. Including nephritis, pyelonephritis, glomerulonephritis. They directly influence the development of the hypertensive process.
There may be a gradual development of malignant hypertension: a life-threatening condition that is difficult to control even in a hospital setting.
Complications
The disease tends to progress and is dangerous due to the development of complications:
- myocardial infarction;
- hypertensive crises;
- cerebrovascular accidents (ischemic and hemorrhagic strokes);
- renal failure, pathological changes in kidney tissue (nephrosclerosis);
- cardiovascular failure;
- aortic aneurysm (dissection of the vessel wall under the influence of increased pressure).
Any of these complications of arterial hypertension greatly worsens a person’s quality of life, limits ability to work, any physical activity, and can cause sudden death.
Causes not related to diseases
Relatively physiological factors in the development of the problem are also possible: for example, puberty (during the puberty of a teenager, blood pressure fluctuates, it needs to be monitored).
Menstrual cycle (in any phase), pregnancy (gestation is associated with a temporary increase in blood pressure or the reverse process, which is considered completely normal).
Menopause or premenopausal period. The more severe the gynecological history, the more complex the course of menopausal syndrome is.
Related factors
In addition to the main reasons that provoke a sharp rise in blood pressure, there are a number of factors that can “trigger” the mechanism for the development of hypertension in the body.
In medicine, they are usually called risk factors. They are reversible, that is, under certain circumstances and actions they can be eliminated completely. There are also irreversible factors that, unfortunately, cannot be changed. The table below lists these factors by group:
ReversibleIrreversibleObesity (any stage).
Excess body weight.
Compounded heredity. Excessively salty foods often
(50% of patients) becomes the root cause of the development of hypertension.
Age and gender.
In men under 40 years of age, arterial hypertension is detected several times more often, in contrast to women. After age 50, the risk increases for both sexes.
Physical inactivity (tendency to a sedentary life). Diabetes mellitus. Diet that stimulates high cholesterol. Frequent stress. Adverse habits: smoking, alcohol addiction.
Important point! Knowing about the existence of such reasons, a person, subject to certain rules, can avoid undesirable consequences.
Are such indicators dangerous during pregnancy?
Depends on what normal working pressure the expectant mother had before pregnancy. If it was at the level of 140 to 90 or slightly higher, such indicators can be called relatively normal and safe.
But if the tonometer levels were 110-120 to 70-80 and went up sharply, this is a reason to be wary and consult a cardiologist for possible examination and treatment.
In general, the development of hypertension in pregnant women is not considered a variant of the physiological norm.
Rather, we are talking about the formation of a pathological process of one kind or another: the kidneys, adrenal glands, and the hypothalamic-pituitary system are most often affected during gestation.
Accelerated growth of tumor structures is observed; neoplasia of the anterior lobe of the pituitary gland, that is, adenomas, is most often detected).
The formation of secondary hyperthyroidism is less common. This is dangerous for both the mother and the fetus, since it is fraught with disturbances in the physical and mental development of the child. In all controversial cases, do not hesitate to consult a doctor.
Non-drug therapy
If hypertension has not become chronic, then folk remedies can help. The most popular decoctions are:
- Motherwort.
- Hawthorn.
- Dennika.
- Melissa.
If you have VSD or other chronic pathologies, then you need to be careful with herbs. Don’t rely on reviews from your relatives, but look at the characteristics of your body and read contraindications.
With a one-time increase in pressure, breathing exercises will help you. Take a sitting position and take 10 deep breaths. This will help reduce blood pressure by 10-20 units. The ear massage also worked well. Rub them in different directions until they become red, but do not overdo it so that it does not hurt. This will change the blood flow and reduce the tonometer readings.
Self-massage at certain points is also useful for eliminating the symptoms of hypertension:
- Massage the point between the index and thumb of your right and left hands alternately.
- Apply pressure to a point just above your elbow when your arm is bent. Massage in circular motions for 5 minutes.
- Massage the middle of your foot for a couple of minutes.
- The point two fingers below the knee is also responsible for blood pressure. Massage it for five minutes.
Additional measures to reduce pressure when it is at around 150 to 100:
- Baths with lavender oil and table or sea salt are good for relieving fatigue, relaxing and lowering blood pressure. 2-3 procedures per week for 20 minutes are enough.
- Proper nutrition and a healthy lifestyle. Do not overeat, especially at night, do light sports or exercise, monitor the balance of carbohydrates, fats and proteins, and a sufficient amount of vitamins.
- Garlic boiled in milk. Drink half a glass three times a day.
- Reduce salt consumption, it is advisable to add only pinches of it to prepared dishes.
- Quitting smoking and drinking alcohol.
- Fight obesity - diet food prescribed by a specialist and moderate physical activity.
- A course of physiotherapy on the advice of a doctor.
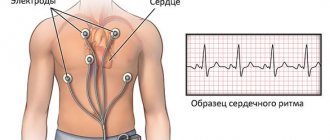
Heart Rate Estimation
The pulse plays a secondary role in determining the degree of danger of pathology.
There is no direct relationship between pressure readings and heart rate. These are different mechanisms.
It is necessary to evaluate blood pressure indicators, and only then consider heart rate.
If the pulse at a pressure of 150/100 or more exceeds 90-100 beats per minute (weak tachycardia), this means that the heart muscle is not coping with the task assigned to it. The reason lies in a violation of the neuro-reflex regulation of the third reflexogenic zone of the heart, responsible for pulse indicators.
We are talking only about a regular and long-term condition. A one-time jump in heart rate means nothing. A pulse of 60-80 is normal. This is a typical picture for hypertension in the considered values.
Pressure 150 over 70 (150 over 60): normal or pathological?
The optimal pressure is considered to be 120/80, the concept of an individual norm includes indicators from 130/85 to 140/90, but anything that exceeds these numbers is already dangerous for a person due to its destructive consequences.
Blood pressure readings of 150/70 (150/60) are the first stage of hypertension, unless we are talking about a single surge in pressure as a result of stress or physical activity, atmospheric disasters or overeating, or taking certain medications.
Blood pressure is not a constant value: in young people, diastolic pressure increases more often, and the increase in systolic pressure is not related to age. If only the systolic indicator increases, we speak of isolated systolic arterial hypertension (ISAH). Blood pressure 150/70 (150/60) is one of the variants of this disease.
Fluctuations in arterial markers depend on the gender, age, constitution of a person, his habits, and lifestyle.
Almost always, blood pressure is related to heart rate. Analysis of heart rhythm and blood pressure helps doctors identify arterial hypertension and prevent the development of hypertension.
Symptoms requiring consultation with a specialist
As trite as it may seem, doctors exist to treat. Therefore, you need to discard imaginary shyness and other limiting factors, and if you have any suspicions, contact a specialist.
There is a list of symptoms that cannot be ignored.
Among them:
- Headaches of varying degrees of intensity. Even weak if the symptom has a long course. At a minimum, differential diagnosis is required.
- Dizziness is again of a long-term nature.
- Nausea.
- Vomiting without relief. It is reflexive in nature. Develops due to irritation of certain areas of the brain.
- Shortness of breath, especially when at rest.
- Visual disturbances, including photopsia, fog, blurred images.
Which specialist to choose in case of high blood pressure
To begin with, if the tonometer shows increased readings more and more often, it is worth visiting your local physician. He will conduct an inspection and, if no serious deviations are identified, in the first stages his recommendations will be quite sufficient.
If the appeal was delayed, and there is a risk to health, then you should go directly to a doctor who treats heart diseases - a cardiologist. It is also worth visiting a neurologist and nephrologist, since in its advanced form the disease can cause damage to individual organs.
How to reduce blood pressure at home
First of all, you need to take a semi-sitting position. If antihypertensive drugs (for example, Andipal) have not been prescribed by a doctor, you can lower your blood pressure by 150/100 or more on your own only with the help of light sedatives based on herbal ingredients: motherwort or valerian, most importantly in tablet form and not in alcohol form. Valocordin and Corvalol will also help.
You can take pills to quickly lower blood pressure (for example, Captopril or Clonidine) only if they have been prescribed by a doctor. Otherwise (the body's reaction is unknown) the vessels may not withstand the pressure drop.
If, after the described actions, the tonometer readings do not decrease within 30-40 minutes, an ambulance must be called.
Treatment with drugs
There are several groups of medications that are good for lowering blood pressure. Only a specialist can tell you which pills to take; you shouldn’t buy them yourself. Highlight:
- Calcium antagonists – Diltiazem.
- Diuretics – Torasemide.
- Beta blockers – Bisoprolol.
- Angiotensin receptor blockers - Losartan.
- ACE inhibitors – Enalapril.
- Alpha adrenergic blockers – Urorek.
Any drug must be used according to the instructions or doctor's orders. Take the full course, and do not stop treatment after the first improvement.
Necessary research
The patient must be examined on a scheduled or urgent basis, depending on the nature of the process and at the discretion of the treating specialist.
The list of diagnostic procedures is presented by the following activities:
- Interviewing the patient for complaints. It is important to objectify complaints in the form of specific symptoms. This will help assess the patient’s condition and determine a possible diagnosis.
- Taking an anamnesis: it is important to establish the facts of the presence of bad habits, lifestyle, physical activity, etc.
- Measuring blood pressure levels on both arms, with an interval of 10-15 minutes.
- Daily blood pressure measurement using a special monitor or daily tonometer. Makes it possible to establish the presence of pathology.
- Heart rate study.
- Electrocardiography. Required to assess the condition of the myocardium and determine the nature of cardiac activity.
- Echocardiography. A more accurate technique that allows you to visualize the heart and surrounding structures.
Other studies are possible at the discretion of the cardiologist or other specialized specialists: determination of hormone levels in the blood, encephalography.
Doctors whose help may be required: endocrinologist, nephrologist, nephrologist (doctor who treats pathologies of the kidneys and excretory system).
Measurement errors
Sometimes you have to observe the following picture: when measuring, the device shows that the pressure is elevated, but the person has absolutely no complaints. In such a situation, you can refer to measurement errors or a malfunction of the device itself. To verify the veracity of one of these two versions, you need to repeat the procedure half an hour after the first test.
And for greater accuracy of the result, the person being examined is recommended to do the following:
- 5-10 minutes before the measurement, limit physical activity,
- when preparing for the procedure, strictly follow the instructions, fasten the tonometer cuff in the proper place on the arm (above the elbow),
- the hand should not hang in the air,
- During the measurement process, the patient should not move or talk.
If the repeat test again shows 150/100, you must inform your doctor about the measurement results or go to an appointment at your local clinic.
Therapeutic tactics
Treatment involves taking certain medications to lower blood pressure. But this is not enough, this is symptomatic therapy.
Etiological treatment involves combating the root cause of the condition, that is, the underlying disease. Depending on the primary pathology, it will be different. This issue is resolved at the discretion of a group of specialists.
Relieving high blood pressure involves taking the following groups of medications:
- ACE inhibitors.
- Diuretics or diuretics.
- Calcium channel blockers.
- Beta blockers.
The specific names of the drugs (there are more than 150 of them) are selected by the doctor, first prescribing in minimal dosages, since the body’s reaction may be different.
It is important to change your lifestyle, quit smoking, alcohol (completely), reduce salt intake, normalize your drinking regimen, physical activity regimen, and diet.
A specialized diet with a maximum content of healthy foods (plant origin), protein, and a minimum of fast carbohydrates and sugar is indicated.
If you have increased body weight, weight loss measures are recommended, but they must be carried out with caution. A complete abstinence from fatty, fried, smoked, salty, semi-finished and canned foods is expected.
In the system, treatment measures will have an effect in the short term. Reducing blood pressure from 150 to 100 is not so easy, especially if hypertension is long-term, but if you follow the recommendations, it is quite possible.
Symptoms of hypertension
At levels of 150 to 100, the body begins to suffer from hypoxia, and unpleasant symptoms of hypertension appear:
- dull, pressing pain in the back of the head, spreading to the temporal part;
- blurred vision, dark spots and blurred vision;
- flushing of the face, redness of the skin;
- numbness of the limbs;
- weakness, powerlessness;
- increased sweating;
- temperature changes;
- gagging;
- pressing feeling, pain in the thoracic region;
- sudden fainting, vestibular disorders.
Symptoms appear in the second stage of hypertension. At the initial stage, the disease rarely manifests itself, so many people miss the onset of the disease.
In order not to delay the treatment of hypertension, you need to pay attention to signs warning about the development of the disease:
- sensitivity to weather changes;
- frequent, causeless mood swings;
- increased nervousness;
- deterioration of brain function;
- generalized edema.