The main cause of cerebrovascular accidents is atherosclerosis of the carotid arteries. Atherosclerotic plaques cause narrowing of the carotid arteries, which is an obstacle to normal blood circulation in the brain. Gradually, a complete blockage of the carotid artery develops, which is called occlusion. Impaired patency of the carotid artery is the main cause of ischemic stroke in the modern world. The risk of developing a stroke if the carotid artery is narrowed symptomatically by 70% or more is about 15% per year.
Many people die or become disabled from stroke every year, although modern vascular surgery can prevent it in most patients. Only regular diagnosis and trust in doctors will significantly reduce the risk of stroke. It is much easier to treat atherosclerosis of the carotid artery than ischemic stroke and its consequences.
Causes and risk factors
The carotid arteries are paired large arterial vessels that supply blood to the brain in those sections where the centers of thinking, speech, personality, sensory and motor function are located. The carotid arteries run through the neck and enter the brain through openings in the skull.
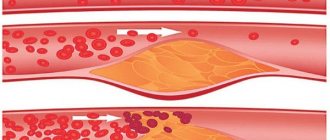
When fatty substances and cholesterol accumulate, an atherosclerotic plaque is formed, which narrows the carotid arteries. This reduces blood flow to the brain and increases the risk of ischemic stroke. A stroke occurs when blood flow does not reach any part of the brain. During a stroke, some brain functions are suddenly lost. If the lack of blood flow lasts more than three to six hours, then these disorders become irreversible.
Why does a stroke develop when the carotid artery narrows?
- Significant narrowing of the carotid artery reduces blood circulation in the brain, and with a sudden drop in pressure (suddenly getting out of bed, flying, overheating in the sun or major surgery), the blood flow suddenly stops, which leads to the death of nerve cells.
- Tearing off a piece of atherosclerotic plaque with its transfer by the bloodstream into small arteries of the brain, which leads to their blockage.
- Acute thrombosis (formation of a blood clot) due to narrowing of the carotid artery with complete cessation of blood flow in certain areas of the brain.
Diagnostics
Depending on the preliminary diagnosis, the specialist prescribes a proper diagnostic regimen.
The process of diagnosing pathologies takes place in several stages:
- Face-to-face consultation with a survey of the patient regarding current complaints, duration and severity of symptoms, the presence of direct provoking factors;
- Study of anamnesis (personal and family);
- Laboratory tests for the presence of atherosclerosis (lipid profile with calculation of the atherogenic coefficient, biochemical blood test, determination of proteins in blood serum, etc., at the discretion of the specialist);
- Magnetic resonance or classical angiography;
- Ultrasound Dopplerography (Doppler ultrasound).
The latest study is considered the most informative. It allows you to determine:
- The speed and intensity of blood flow in the vessels;
- Places that prevent the movement of arterial blood to the brain;
- The presence of atherosclerotic lesions;
- The presence of detachments, dilations, occlusions, stenosis of the vessel;
- The presence of blood clots and atherosclerotic plaques, their size and shape;
- Deformations of the vessel (tortuosity, loops, protrusions, bends);
- Dimensions of the lumen of the affected vessel;
- Condition of the vascular walls (elasticity, mobility, firmness);
- Modifications of the arterial wall.
When a pathology is detected, the specialist prescribes comprehensive treatment to the patient.
Risk factors for carotid atherosclerosis
Risk factors for carotid artery disease are similar to those for other types of cardiovascular disease. They include:
- Age
- Smoking
- Hypertension (high blood pressure) is the most important risk factor for stroke
- High cholesterol
- Diabetes
- Obesity
- Sedentary lifestyle
- Family history of atherosclerosis
Men under 75 years of age have a greater risk of developing carotid artery stenosis than women in the same age group. In the group over 75 years of age, women have a greater risk of stroke. In patients suffering from coronary artery disease, narrowing of the carotid artery is often detected.
Stages of development
If you think that atherosclerosis of the brachiocephalic vessels occurs suddenly, then this is a mistaken opinion. The pathological process often begins at a young age, when cholesterol accumulates in the vessels. The first symptoms appear, on average, after 40 years of age and at first are seemingly harmless. Only when health worsens, for example, against the background of some chronic disease, does a person learn about a disappointing diagnosis. How does vascular atherosclerosis develop?
- Non-stenotic form. The cholesterol plaque blocks the vessel by only 30% and practically does not interfere with blood flow. During the primary stage, blood pressure does not increase significantly, so a person may not even feel such changes. BCA atherosclerosis at this stage is easy to stop and even cure.
- Stenosing form. The cholesterol plaque occupies the entire lumen of the vessel, and blood flow decreases to a critical level. All the symptoms of acute atherosclerosis of the brachiocephalic arteries with stenosis and a deterioration in the general condition of the patient are evident.
- What is stenosing atherosclerosis of the brachiocephalic arteries and how to treat it?
Non-stenotic atherosclerosis of the extracranial parts of the brachiocephalic arteries is determined if the plaque covers less than half of the internal lumen
Complaints and symptoms
Atherosclerosis of the carotid arteries can be asymptomatic or cause complaints associated with impaired cerebral blood flow. Most often, patients may complain of temporary impairment of brain function (transient ischemic attack) or persistent loss of brain function (ischemic stroke).
Transient ischemic attack (TIA)
A TIA occurs when blood flow to the brain is briefly interrupted. This is the initial phase of acute cerebrovascular accident, which is reversible. It has the same symptoms as a stroke, but these symptoms go away within minutes or hours.
A TIA requires emergency medical attention because it is impossible to predict whether it will progress to a stroke. Immediate treatment can save lives and increase the chances of a full recovery.
Modern research has shown that patients who have had a TIA are 10 times more likely to suffer a major stroke than a person who has not had a TIA.
Ischemic stroke has the following symptoms:
- Sudden loss of vision, blurred vision, difficulty in one or both eyes.
- Weakness, tingling, or numbness on one side of the face, one side of the body, or one arm or leg.
- Sudden difficulty walking, loss of balance, lack of coordination.
- Sudden dizziness.
- Difficulty speaking (aphasia).
- Sudden severe headache.
- Sudden memory problems
- Difficulty swallowing (dysphagia)
Ischemic stroke and transient ischemic attack begin in the same way, so any ischemic stroke can be called an ischemic attack if the symptoms completely resolve within 24 hours of the onset of the disease. The presence of a time interval between the onset of stroke symptoms and the death of parts of the brain allows for urgent surgery to restore cerebral blood flow.
Prevention
Preventive measures must be observed by everyone, especially those who have a genetic predisposition to atherosclerosis. They are also important in preventing relapse after successful recovery. The basic rules of prevention include:
- rejection of bad habits;
- choosing a suitable sport taking into account age and health status;
- maintaining normal weight;
- avoiding overeating;
- limiting stress;
- limiting the addition of salt to the diet;
- adherence to the principles of proper nutrition.
Also, an important preventive measure is to consult a doctor in a timely manner if you suspect any health problems.
Thus, non-stenotic atherosclerosis is a serious problem associated with the formation of cholesterol plaques on the walls of the arteries. The sooner it can be diagnosed, the greater the consequences can be avoided. Treatment requires complex therapy: medication, diet therapy, and lifestyle changes.
Course of the disease
Once atherosclerotic plaques appear, they will no longer be able to resolve, but only gradually progress. The rate of growth of an athersclerotic plaque depends on many risk factors, including cholesterol levels. All people over 50 years of age are recommended to undergo an annual ultrasound of the carotid arteries in order to exclude the development of atherosclerotic plaques and the risk of ischemic stroke.
With the development of complications of atherosclerosis of the carotid arteries, discirculatory encephalopathy quickly progresses. Frequent TIAs, and even more so ischemic stroke, contribute to the death of part of the brain tissue and disruption of brain function. Patients with atherosclerosis of the carotid arteries often develop vascular dementia (dementia).
After restoration of the patency of the carotid artery, the phenomena of cerebrovascular insufficiency are stopped, and the likelihood of repeated cerebrovascular accidents is significantly reduced.
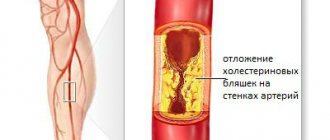
Atherosclerotic disease of the arteries of the lower extremities without stenosis
As mentioned above, with this type of atherosclerosis, the vessel is blocked by less than 50%.
Frequent patient complaints
In the initial stages of the disease, patients, as a rule, do not make complaints, or patients do not pay attention to the symptoms.
The main features include:
- pain in the thighs, buttocks, lower back, calf muscles;
- increased pain with physical activity;
cold skin in the legs;- nausea;
- dizziness;
- feeling of numbness in the limbs, “crawling”, tingling;
- change in skin color (pallor);
- poor wound healing;
- cramps in the muscles of the lower extremities;
- itching, peeling of the skin of the legs;
- roughening of nails and skin of the feet;
- cracks, hair loss on legs.
Criteria necessary for diagnosis:
- Systolic blood pressure (BP) increases, while diastolic blood pressure does not increase.
- The skin of the legs, especially the feet, is cold to the touch.
- Blood test for: cholesterol, triglycerides, low-density lipoproteins – the indicators are increased; high density lipoproteins – reduced.
- Weakening of pulsation in the main arteries of the limbs.
- Doppler ultrasound. Sonographic signs of pathology: the presence and determination of the size of plaques, slow blood flow in the vessels, their damage and wall injuries.
- Angiography - places of vascular narrowing are visible (up to 50% of the lumen).
- Computed tomography is also partially capable of detecting all of the above changes.
Directions in treatment
Therapy is selected individually for each patient, but basically it includes:
Statins: simvastatin, atorvastatin, rosuvastatin (in the absence of contraindications).- Vasodilators (antispasmodics): nitrates, papaverine, dibazol.
- For the prevention of thrombosis: antiplatelet agents - aspirin, chimes, clopidogrel; anticoagulants – warfarin, rivaroxaban, dabigatran.
- Vitamin preparations and antioxidants.
- A healthy lifestyle aimed at losing weight.
- Blood pressure control - it is not recommended to allow systolic blood pressure to rise above 140 mmHg.
- Physical education classes, swimming, exercise bike.
- Treatment of chronic diseases.
- Refusal of alcohol, smoking, excessive consumption of coffee and tea.
- Elimination of animal fats and salt, increasing the amount of fruits and vegetables in the diet.
The duration of drug therapy is 1.5 – 2 months. The course must be repeated 4 times a year.
Prognosis for future life and rules of observation with a doctor
This disease should not be taken as a death sentence. Narrowing of arteries without stenosis is not a critical point. The most important thing is to try to stop the progression of the atherosclerotic process, which can be achieved by following the above recommendations.
Forecast
Carotid atherosclerosis carries a significant risk of ischemic stroke. With asymptomatic narrowing of the internal carotid artery of more than 70%, the risk of ischemic stroke exceeds 5% per year. If the patient has had episodes of cerebrovascular accidents, then this risk is already 25% per year.
The risk of ischemic stroke in asymptomatic atherosclerotic plaques with a narrowing of less than 70% does not exceed that in patients without atherosclerosis.
After adequate restoration of blood circulation in the carotid arteries, the risk of ischemic stroke is reduced by more than 3 times.
Minimally invasive methods of treating stenosing atherosclerosis of BCA
The clinic is equipped with equipment for performing several types of hemocorrection. Often, a correctly selected method in combination with drug treatment provides excellent results without surgical intervention. Hemocorrection allows you to eliminate certain substances from the blood (in this case cholesterol), and medications prevent their reappearance. After completing the course of treatment, the patient receives recommendations for changing diet and lifestyle. Positive results can often be maintained for many years.