In hematology, there is a wide group of conditions that cannot be clearly classified as normal or pathological.
The problem is that it is quite difficult to immediately determine which of them is available, and even an experienced specialist requires at least several weeks, or even months of analytical work.
Hemolysis is a necessary physiological condition that involves the destruction of red blood cells. Normally, the rate of hemolysis is determined at 120 days. That is, every 4 months the old shaped structures die off and are replaced by new cells.
With excess, a pathological process occurs. And extremely dangerous. If quality treatment is not started, there is a possibility of death from complications. Like thrombosis and other abnormal conditions.
Hemolysis of red blood cells in the blood occurs constantly, without interruption. Therefore, you need to look at exactly how the alleged pathological process develops, and then draw conclusions about its physiology or pathogenicity.
What do patients need to know about hemolysis? When can it be called normal and when abnormal? You need to look into the issue carefully.
The essence of the process and its role in the body
As already mentioned, hemolysis is a natural process. Blood cells live for about 120 days. Then they die having fulfilled their function.
New, fresh ones are replacing them. They mature in the bone marrow. Blood hemolysis is the completion of the life cycle of red blood cells, and the analysis shows how quickly or slowly the process occurs relative to normal values.
In its development, the condition goes through a group of stages:
- The first concerns the actual beginning of the phenomenon. The strength of the cell membrane decreases. This is normal, because, relatively speaking, the red blood cells are “old”, having served their purpose.
- The second stage begins after the red blood cells wear out. The shell is gradually destroyed. Red blood cells die.
- A huge amount of hemoglobin is released into the blood, which ensures normal life functions. During active hemolysis, indicators may increase to catastrophic levels.
The body utilizes cell fragments plus those substances that remain after the death of shaped structures.
Why is the described process needed at all?
It performs several functions:
- Ensuring cellular respiration. After maturation, red blood cells take a long time to solve the problems facing them. Around the 4th month, all sorts of changes in the structure begin. Red blood cells cannot supply the body with oxygen. Hence the decrease in the quality of tissue respiration and gas exchange. Hemolysis ensures the turnover of formed cells.
- Preventing genetic mutations. Old red blood cells can degenerate. Thus, they no longer fulfill the tasks assigned to them. For obvious reasons, it is better to get rid of such cells. And the body completely agrees with this.
An indirect function that has nothing to do with natural life activity - the increase in hemolysis indicators plays the role of an indicator of health status. The more destroyed cells, the more likely the pathological process.
There are several types of hemolysis. In the overwhelming majority of cases, we are talking about a natural, biological state. Which does not pose any danger to life.
How does a red blood cell participate in respiration?
Red blood cells are responsible for saturating the blood with oxygen and removing unnecessary carbon dioxide accumulations. To achieve this, most of the cell mass is occupied by hemoglobin (globin protein + 4 heme/iron molecules). It is called "blood pigment" because heme is what gives blood its color. Depending on the sequence of amino acids, different types of pigment are distinguished in globin.
The oxyhemoglobin complex is formed by combining with oxygen. It is created in the pulmonary capillaries, and in the tissues it breaks down again and releases free oxygen to the cells.
The appearance of methemoglobin or carboxyhemoglobin in the blood during poisoning and intoxication disrupts the process of oxygen transfer and leads to tissue hypoxia.
Classification
Typing is carried out by hematology specialists. There are several ways to subdivide the process. The first criterion for erythrocyte hemolysis is the nature of the phenomenon.
Accordingly, they distinguish:
- Biological variety. The same one that was discussed above. This is a completely normal, vital condition. It is accompanied by the natural aging of red blood cells and further death of spent cells. When they talk about hemolysis, they most often mean the biological variety.
- Chemical form. Occurs when the body is poisoned with all kinds of poisons. Substances synthesized by snakes and some insects are especially dangerous. There are also more familiar options - the effects on the body of vapors of acids, alkalis, lead and arsenic poisoning.
All these compounds increase the rate of hemolysis and cause massive death of still functional red blood cells. It is considered an extremely dangerous species. Membranes are destroyed by poisons.
- Osmotic form. Almost occurs in natural conditions. Unless the patient receives an excess amount of solution intravenously. More often observed in laboratories.
It is detected during simple manipulations with chlorine-containing substances. These compounds increase the permeability of red blood cells to water. As soon as there is a lot of liquid, the membrane overstretches and collapses.
- Types of hemolysis also include a mechanical form. In this case, the red blood cells collapse as a result of gross physical influence. For example, vigorous shaking of a test tube.
For obvious reasons, this almost never happens in the natural environment. Except for situations involving extensive injury. More often observed in laboratory conditions.
- Hemolyzed blood is obtained by heating the tube or sharply cooling it to below 2 degrees Celsius or even a little more. Under the conditions of the body, this is also possible. But only at very high temperatures.
Red cells die and are destroyed at temperatures of about 42-43 degrees Celsius. It is quite possible to encounter such a fever. Patients in this condition are sent to the hospital for urgent, emergency measures.
Regulation
There are different types of regulation of erythropoiesis - humoral, nervous, with the help of reticular cells, vitamins and minerals.
Humoral regulation is carried out according to the principle of negative feedback. Thanks to the hormone erythropoietin, the processes of formation of young erythroid cells and disintegration of old, deformed bodies are clearly balanced and continuous. The level of red blood cells in the blood remains relatively stable and ensures adequate blood supply and tissue oxygenation. Organ hypoxia caused by vascular spasm, anemia or other pathology stimulates the secretion of erythropoietin, which enhances the production of red cells and increases their concentration in the blood. When the blood supply to the organs is restored, the secretion of erythropoietin decreases.
Other hormones that control erythropoiesis include: cortisol, androgens, glucocorticoids, insulin, somatotropic and thyroid hormones, catecholamines, interleukins, placental prolactin. They increase the production of erythropoietin or directly stimulate hematopoiesis. Erythropoiesis is suppressed by estrogens, calons, glucagon, acetylcholine, interferons, and tumor necrosis factors.
- The growth and development of the human body is accompanied by an increase in the intensity of erythropoiesis.
- With hyperglycemia and hypothyroidism, anemia develops, and with thyrotoxicosis, erythrocytosis occurs.
- Under severe stress, the production of red blood cells increases and blood supply to tissues improves.
- Hypofunction of the adrenal glands is accompanied by erythropenia, and hypercortisolism is accompanied by erythrocytosis.
Nervous regulation occurs as follows: the sympathetic system activates erythropoiesis, and the parasympathetic system inhibits it.
Reticular cells influence the process of hematopoiesis in two ways:
- Phagocytosis is the process of absorption and digestion of cell membranes, destruction of mature red blood cells with developmental defects, and cessation of metabolism of erythroblast nuclei.
- Ropheocytosis is the transfer of ferritin, formed after the breakdown of abnormal red blood cells, to young orthochromatic erythroblasts.
Macrophages have a direct effect on the proliferation and maturation of erythroid cells. They absorb normoblast nuclei, provide erythroblasts with iron and nutrients, stimulate the synthesis of erythropoietin and glycosaminoglycans, which increase the concentration of growth factors in the islets.
Some vitamins and minerals are critically needed for erythropoiesis:
- cobalamin - triggers the secretion of globin,
- folic acid - takes part in the formation of DNA nuclear forms,
- pyridoxine – provides heme production,
- riboflavin - formation of the lipid membrane of erythrocytes,
- Vitamin C - accelerates the absorption of iron,
- vitamin PP – strengthens the lipid stroma and prevents hemolysis,
- copper - allows iron to be absorbed more quickly in the intestine and be included in the heme structure,
- nickel and cobalt – formation of iron-containing blood protein,
- zinc - is part of vital enzymes,
- selenium - protects cells from free radicals.
The lack of one of them can cause a violation of erythrocytopoiesis, namely the differentiation and division of stem cells.
Where red blood cells are destroyed
According to localization, there are three places:
- Intracellular hemolysis. The destruction of red blood cells in the human body occurs in liver cells. As a red blood cell ages, its protein components break down into amino acids, and the iron that was part of the red blood cells is retained by the liver and can be reused in the formation of new red blood cells.
- Intravascular hemolysis. As the name suggests, cell breakdown occurs directly in the blood vessels.
- Extracellular. This refers to a situation in which red blood cells are destroyed under the influence of an external factor. Often outside the body altogether, for example, in a laboratory.
According to the process, the following are distinguished:
- Acute hemolysis. Characterized by a sharp increase in the “mortality” of red blood cells. Red blood cells die quickly and in large quantities.
Attention:
If nothing is done, the patient has a greater than 70% chance of dying within a couple of days.
Therefore, such a condition is corrected immediately. In a hospital or even intensive care.
- Chronic hemolysis. Another type of pathological process. Accompanied by constant, albeit rather weak, cell death. This is clearly visible during dynamic tracking. Checking the blood.
- Natural state. Normal hemolysis is considered the last in this triad. It is not considered a pathology. For obvious reasons.
All classifications are used to more accurately describe the diagnosis. Identify the process and quickly begin treatment. The work falls on the shoulders of hematology specialists. Less often than other doctors.
“Portrait” of a middle-aged red blood cell
Cell size is determined by diameter, which is 7.5 microns (micrometers). This is 6 times smaller than the thinnest human hair. The total surface of all red blood cells is 1.5 thousand times greater than the covering of the human body. The change in size is called anisocytosis.
The shape of the cells is flat, with thickenings along the edges, forming a disk concave on both sides. The “design” of the cell is determined by the optimal distance of each surface point to the center, this increases the possibilities of contact with transported gas molecules. There is no nucleus inside the cell (fish, birds and amphibians have one), which is associated with an adaptation to binding more hemoglobin.
Disturbance in the shape of blood cells is called poikilocytosis. Up to 15% of altered cells are allowed.
Red blood cells do not synthesize their own protein; 71% of the cell mass is water, 10% is the membrane-covered membrane. Cells are economically powered by energy obtained without oxygen.
Reticulocytes are larger in size; inside there is a mesh formation containing amino acids and fats.
The plasma membrane is half composed of glycoproteins; it is capable of transmitting oxygen, carbon dioxide, electrolytes sodium and potassium, and water. This suggests that a violation of the protein-lipid composition of the blood (cholesterol levels) leads to premature wrinkling and destruction.
By weight, up to 90% is occupied by hemoglobin (a chemical compound of iron and protein).
Causes of pathological breakdown of red blood cells and what treatment is needed
There are more than 10 factors in the development of the disorder. The following conditions are especially common.
Poisoning
As mentioned earlier, in this case the body is affected by toxic substances. The pathological process is accompanied by intense symptoms. Including others, except those that characterize hemolysis.
Salts and non-metal vapors pose a particularly great threat. For example, boron, bromine and others. Metals, salts, and alkalis are no less dangerous. Classic situations involve arsenic, lead, and mercury. All of them cause premature cell death.
Treatment is carried out in two stages:
- First, a detoxification course is prescribed. It is necessary to eliminate the poisoning as quickly as possible. Actually, remove the metabolic products of compounds and the toxic components themselves.
- Then a course of maintenance treatment is prescribed. Vitamins, diuretics to eliminate the remains of dangerous substances. Everything takes up to several weeks.
Next, the recovery period begins. The concentration of normal red blood cells increases on its own. As soon as the main pathological process is eliminated.
Excess medications, saline solutions
For example, sodium chloride. It is good in strictly prescribed dosages. Because with an excessive amount of substances, chlorine passes through the cell wall more actively.
Then the process of gradual penetration of fluid into the red blood body begins. Ultimately, the concentration of water inside increases. The cell membrane cannot withstand physical stress and collapses. Thus, the red blood cell also dies.
Treatment is carried out in a hospital setting. Typically, the patient is monitored. The blood is checked several times to determine the extent of damage and the rate of self-recovery.
If the condition becomes critical, a transfusion is prescribed. Red blood cell mass is needed; the liquid fraction is not used.
Injuries
Mechanical tissue damage. In such a situation, acute hemolysis develops, since the influencing factor is extremely intense.
The larger the area of physical tissue destruction, the worse the situation with the general condition. If the damage is extensive, shock and death are likely. Even doctors are not always able to correct the situation.
Treatment. Saline solutions and glucose are prescribed to nourish the body. It is imperative to restore the integrity of the tissues. Eliminate possible damage on the spot and quickly. Probably by surgery. The patient is then observed. In case of heavy blood loss, transfusion is indicated.
Burns
A type of mechanical damage, but of a slightly different nature. Thermal injury causes reflex death of red blood cells.
Because toxic substances like histamine are released in large quantities. They have a detrimental effect on the state of the body - they destroy cells.
There are other dangerous compounds. The result is a dual situation: on the one hand, you need to correct the burns, and prevent the patient from going into shock and dying. On the other hand, you should also work on your blood condition.
Treatment:
- Saline solutions are prescribed without fail. Infusion medications help restore electrolyte balance and nourish the body.
- For burns, contact a combustiologist. The question of how to correct the disorder is decided on the spot. Amputation of the affected parts and segments is possible.
- Large areas are covered with skin flaps, and other techniques are used.
The question is individual and quite difficult. But it needs to be resolved quickly.
Autoimmune diseases
Of very different nature. Moreover, there is a direct relationship: the more intense the body’s pathological response, the worse the situation with hemolysis. He becomes too fast and no longer meets the criteria for being “physiological.”
We are talking about a variety of diseases: from rheumatoid arthritis to lupus erythematosus. The probability of developing a pathological process is quite wide: from 5 to 50-70% and even more. Depends on the diagnosis and its activity.
Treatment:
- At the first stage, drugs from the glucocorticoid group are used. They eliminate the excessive response of the body's defenses.
- Then, they look at the patient's condition. If everything went well, the symptoms have subsided, the drug is taken for some time, then stopped. Prednisolone and Dexamethasone are mainly prescribed. Other analogues. And so on according to need. during exacerbations.
- If it doesn’t help, use cytostatic drugs. To eliminate the excessive immune response and reduce its false work to a minimum.
Immunological incompatibility of injected blood
{banner_banstat9}
Occurs if the group or Rh factor does not match. In this case, new cells will be attacked by protective forces and destroyed. The consequences are catastrophic.
Massive death of red blood cells leads to disruption of the entire body. Due to the huge concentration of hemoglobin, thrombosis begins. Deadly.
Treatment. Therapy in the intensive care unit.
Infectious disorders
Red blood cells are destroyed by bacteria such as staphylococcus. By the way, several of its varieties are even named accordingly.
Infection with hemolytic streptococcus always causes accelerated hemolysis, since bacteria have the ability to destroy cells. Albeit in an indirect way, without direct “intention”. The problem is in those substances that are synthesized and released as a result of the vital activity of the microorganism.
Treatment is carried out under the supervision of an infectious disease specialist or a therapist plus a hematologist.
- The sensitivity of the pathogen to antibacterial agents must be examined. For example, they take a swab from the throat and other mucous membranes. Only then is a course of therapy prescribed. With the help of an antibiotic.
- The temperature is brought down with antipyretics. Antipyretics of the usual types: Paracetamol, Ibuprofen in various modifications. Here are the choices for patients and doctors.
- Be sure to prescribe a regimen. Usually bed. It is also recommended to consume more fluids.
Taking certain medications
{banner_banstat10}
In addition to the already mentioned saline solutions. We are talking about medications of the corticosteroid group. This also occurs with the use of anti-inflammatory drugs. Especially without the supervision of a doctor and without following the dosages in the instructions.
Attention:
There is a possibility of encountering a problem with the systematic use of oral contraceptives.
Treatment. As such it is not necessary. Usually, it is enough to give up one or another pharmaceutical drug, and everything returns to normal. But you cannot stop taking medications without permission. You need to consult a doctor. By profile.
Symptoms
The clinical picture depends on the severity of the pathological process. Chronic forms with insignificant indicators, an increase in them, are not accompanied by pronounced clinical symptoms. As a rule, we are talking about a group of implicit manifestations.
- Often low blood pressure. 5-10 mmHg less than normal.
- Discomfort in the chest.
- Weakness.
- Poor exercise tolerance.
Much more obvious symptoms that red blood cells are being destroyed are noticeable in an acute condition:
- Chest pain. This is the result of insufficient nutrition of the myocardium. There are fewer red blood cells, which means not as much oxygen comes in. The problem is that the normal position can only be restored by correcting the underlying disease. It's not always easy. And time goes by for months. Especially during an aggressive process.
- Increased body temperature. Growth up to 37-38 degrees. It persists for a long time until the condition is corrected.
- Feeling of weakness, drowsiness. Accompanies the patient at all times. Even after a good, quality rest.
- Possible increase in blood pressure. Also the fall. Depends on the individual characteristics of the body and the degree of damage.
- The hemolysis index is increased, and with pathologies of the kidneys and excretory system it is accompanied by lower back pain. Typically, the discomfort does not increase after physical activity or a change in body position. Nothing changes even after visiting the toilet.
- Anxiety. Constant fear for no reason. Panic attacks are possible.
- Feeling hot. Rush of blood to the face, which ends in hyperemia. Redness. Then, just as abruptly, the process reverses. The skin becomes pale or bluish.
- In critical conditions, voluntary emptying of the bladder and intestines is observed.
Clinical manifestations are varied and depend on the severity of the pathological process.
Additional examinations
Basically, a general blood test is prescribed. Then, besides it, the following are shown:
- Oral interview with the patient. Anamnesis collection. A hematology specialist is working on this.
- Visual assessment of body tissues.
- Ultrasound of the digestive tract.
- If necessary, MRI is also prescribed.
- Immunological tests.
- Examination of throat smears for flora. Her sensitivity to antibiotics.
Hemolysis is a natural and normal process. Usually. All deviations are considered as manifestations of potential diseases. In this case, diagnosis and treatment are needed.
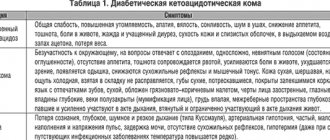
Types of hemolysis
| View | a brief description of |
| Intravascular | The destruction of red blood cells occurs as a consequence of anemia, hemolytic gas poisoning, and autoimmune diseases. Occurs directly during blood circulation |
| Intracellular | The process of hemolysis is observed in macrophage cells and is activated due to autoimmune types of anemia, thalassemia |
Attention!
The process of destruction of red blood cells can be caused artificially under the influence of poisons, an incorrectly performed blood transfusion, as a result of the influence of certain acids.