The subclavian artery is a paired vessel that consists of a right and left branch with branches. Together with other vessels, it forms the systemic circulatory system and originates from the anterior mediastinum. It transports oxygen, nutrients to the neck, upper limbs and other organs of the upper body. When an artery is damaged, blood flow is disrupted, which leads to various dangerous diseases. It is important to identify the pathology in time and carry out treatment, otherwise the likelihood of the patient’s death increases.
Location of the subclavian artery
The topography of this vessel is not as complex as it might seem at first glance. The right artery is the final branch of the brachiocephalic trunk (common and external carotid arteries), and the left artery arises from the flexure of the aorta. The left subclavian artery is longer than the right (about 2.5 cm), and its intrathoracic section is located behind the brachiocephalic vein. The subclavian vein is located anterior and inferior to the arterial vessel of the same name.
The subclavian artery is divided into 3 sections
The artery is located in a small space limited by the collarbone and right rib. In appearance, it is a convex arc that goes around the apex of the lung and the upper part of the pleural sac. Having reached the first rib, the vessel passes between the middle and anterior scalene muscles, where the brachial plexus is located. Having bypassed the rib, it goes under the collarbone, ending up in the axillary space.
Anatomy of the subclavian vessel depending on its sections.
Branches of the first department:
- The vertebral (vertebral) artery passes through the transverse process of the VI cervical vertebra, rises and enters the cranium through the opening between the skull and the spine. It then connects to the vessel on the other side, forming the basilar vessel. The vertebral artery supplies blood to the spinal cord, muscles, and occipital lobes of the brain.
- The internal thoracic artery emerges from the lower surface of the subclavian vessel. It saturates the thyroid gland, bronchi, diaphragm and other organs of the upper body with blood.
- The thyrocervical trunk comes from the scalenus muscle, its length reaches no more than 1.5 cm and is divided into several branches. This branch saturates the inner lining of the larynx, the muscles of the neck, and the shoulder blades with oxygen.
The second section has only a costocervical trunk, which emerges from the posterior surface of the subclavian vessel.
The third section is the transverse cervical arterial vessel, which penetrates the brachial plexus. It saturates the muscles of the shoulder blade and neck with blood.
Aberrant subclavian artery is a common pathology of the aortic arch, which is characterized by a deviation from the normal structure of the vessel. In this case, the right vessel branches from the arch and passes through the posterior mediastinum to the right.
Its location depending on the esophagus:
- 80% - behind the esophagus;
- 15% – between the esophagus and trachea;
- 5% - in front of the trachea.
And the left arterial vessel goes to the right of the arch behind the esophagus, creating an incomplete vascular ring with the left arch.
Vertebral artery syndrome with neck osteochondrosis
According to statistics, the majority of disorders (more than 70%) are degenerative-dystrophic changes in the body or osteochondrosis. The rest consists of congenital anomalies of the structure of the vertebrae or vertebral arteries, postpartum injuries, scars, tumors, herniated intervertebral discs and overgrown osteophytes, vertebral instability, etc.
Vertebral artery syndrome is a symptom complex of cerebral, vascular, and autonomic abnormalities that occurs as a result of compression of the vertebral arteries, deformation of their walls, or narrowing of the lumen of the blood canal.
Anatomy
The vertebral artery is a paired formation that arises from the subclavian arteries and runs in the canal formed by the openings of the transverse processes of the cervical vertebrae. After passing through the atlas and occipital foramen of the skull, the vertebral arteries merge into a single basilar artery, which supplies blood to the posterior parts of the brain. Any circulatory disorders immediately affect the nutrition of brain and nerve cells, causing severe headaches and dysfunction of the organs of vision and hearing.
On the one hand, the cervical spine has a rather delicate structure, a thin muscular corset and ligamentous apparatus, and does not have such reliable protection as other segments. On the other hand, he constantly experiences colossal loads (supports a fairly heavy skull, turns and tilts his head, etc.). Due to the natural deflection, the neck does not rest even during sleep.
In a normal healthy state under normal physiological conditions, the vertebral arteries are also compressed, limiting blood flow, but it is practically not impaired due to sufficient compensating conditions. The condition of the vessels can change due to anatomical narrowing of the lumen of the channels, atherosclerotic stenosis. Soft tissues, for example, the scalene or oblique muscles of the neck, can also have a compressive effect on the arteries, which intensifies after sharp turns or tilts of the head.
Degenerative-dystrophic changes in the body lead to disruption of metabolic processes in the cartilage of the intervertebral discs. Over time, the disc shell dries out, cracks, and flattens, pinching the vertebral arteries. Constant mechanical compression of blood channels entails chronic irritation of periarterial nerve clusters and the development of angiospastic syndrome (constant vasospasm).
Signs of vertebral artery syndrome
Functional symptoms of compression of the vertebral arteries:
- Headaches in combination with autonomic abnormalities. There may be pulsating, burning, aching, constant. As a rule, they originate in the back of the head, then spread to the temples, parietal and frontal parts. They intensify paroxysmally, especially during physical exertion (sudden movements of the head, after a long stay in a forced position, fast walking, running, with strong shaking in transport).
- Cochleovestibular disorders, manifested in the form of paroxysmal systemic or non-systemic dizziness. It manifests itself as a feeling of instability of the soil, rotation of surrounding objects or the body in space, instability of gait, and inability to maintain balance. Sometimes accompanied by slight hearing loss, inability to perceive a certain frequency of sounds.
- Visual disturbances are expressed in the flickering of butterflies or diverging circles before the eyes, pain, a feeling of sand, flashes. During an attack of severe headache, photophobia is noted. An ophthalmological examination shows a slight change in the tone of the vascular system of the fundus.
Organic symptoms accompanied by persistent impairment of cerebral circulation manifest themselves in the form of sudden dizziness, nausea, vomiting, difficult or slow articulation (the ability to pronounce sounds). Drop attacks (sudden falls with preservation of consciousness) lasting up to several minutes, loss of consciousness lasting up to 10 minutes may occur.
The attack usually subsides after the patient assumes a horizontal position. After the attack, there is a feeling of general weakness, sweating, tinnitus, irritation from bright lights, increased heart rate, blood pressure may increase, etc.
Neurological disorders include neuralgia of the occipital nerves, inflammation of the cervicobrachial plexuses, loss of sensitivity or reflex reactions of the lower part of the head, neck, shoulder girdle, and upper extremities. Torticollis may form - a forced tilt of the head, usually in the direction where the artery is pinched, and pain develops. The development of the disease against the background of existing cardiovascular pathologies is dangerous due to the occurrence of angina pectoris, coronary artery disease, etc.
Diagnosis and treatment
Diagnosing vertebral artery syndrome is quite difficult due to the variety of clinical complaints and symptoms. X-ray images do not always give a clear picture (changes are noticeable only in the bone structures of the spine), so an additional CT or MRI examination is required to identify the location and degree of vascular compression.
Magnetic resonance imaging can visualize in more detail intervertebral discs damaged by osteochondrosis, the presence of protrusions or hernias, subluxations of articular processes, vertebral hypermobility and other pathologies.
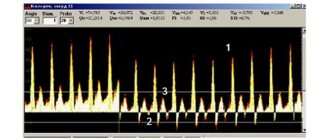
It is possible to identify compression of the vertebral arteries, their congenital anomalies of structure, and determine the asymmetry of the linear velocity of blood flow and the intensity of blood circulation in them using duplex scanning or vertebral Dopplerography. Tests are carried out both in a calm state (relaxed) and with functional loads (with flexion and extension of the neck, lateral bending, rotation).
From hardware diagnostics, electrocardiography and electromyography (determining the passage of nerve impulses) are mandatory. If necessary, a consultation with a cardiologist and neurologist is carried out.
Treatment of patients with vertebral artery syndrome requires an integrated approach. At first, it consists of complete rest, elimination of the compressive effect on blood vessels, reduction of neurogenic inflammation and traditional drug therapy:
- To relieve pain and inflammation - analgesics and non-steroidal anti-inflammatory drugs. In this case, anti-inflammatory drugs are best taken in the form of intravenous injections. Then they have a more gentle effect on the gastrointestinal tract, are more effective and the speed of onset of relief is much higher.
- Muscle relaxants are substances that relieve muscle spasms (relax muscles).
- Vasoactive drugs are prescribed to eliminate vascular inflammation and changes in the arterial bed, as well as to expand the lumen of the canals.
- Vitamins (a high content of B vitamins is especially useful) and anabolic agents - to activate trophic processes and improve the general condition of the body.
- Antidepressants and tranquilizers - for the correction of psycho-vegetative pathologies, improving emotional and psychological mood.
As the pain syndrome subsides, physiotherapeutic procedures (UHF, electrophoresis, ultrasound, etc.), massages, reflexology, and exercise therapy are added to the treatment.
If necessary, wearing a support collar (for example, Shants) and posture correction using traction (spinal traction) may be prescribed. The use of manual techniques (acupuncture, plantar and Thai massages, acupuncture, etc.), swimming, classical and passive yoga has a good effect. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Narrowing of an arterial vessel
This is a common pathology in which the artery located next to the subclavian vein is affected. In most cases, its narrowing is provoked by atherosclerosis and thrombosis. In this case, the first disease, which is characterized by the deposition of low-density cholesterol on the walls of blood vessels, can be congenital or acquired.
Stenosis occurs when a section of the artery narrows
Damage to the artery under the collarbone occurs for the following reasons:
- the patient has hypertension;
- the person smokes, drinks alcohol;
- the patient is overweight;
- suffers from diabetes.
In addition, stenosis is a consequence of metabolic disorders, inflammatory reactions or cancer.
Other factors in the development of stenosis:
- irradiation;
- arterial compression and other compressive neuropathies;
- inflammation of arterial vessels;
- fibromuscular dysplasia, etc.
In some cases, the narrowing of the vessel reaches 80%, and this threatens artery obstruction. As a result, the likelihood of ischemia and stroke increases due to a lack of oxygen and nutrients.
Characteristic symptoms of stenosis:
- muscle weakness;
- increased fatigue;
- pain in the hands;
- hemorrhage in the area of the nail plate;
- necrosis of the soft tissues of the fingers.
In addition, the pathology is manifested by severe neurological disorders:
- visual disturbances;
- speech disorders;
- lack of coordination in space:
- loss of consciousness;
- vertigo (dizziness);
- numbness of the face.
If such symptoms occur, you should immediately consult a doctor to clarify the diagnosis and choose a treatment method.
Pathology treatment methods
To assess the condition of the artery under the collarbone and establish an accurate diagnosis, instrumental and laboratory research methods are used:
- Ultrasound.
- Triplex scanning using contrast agents.
- Arteriography is a study during which an arterial vessel is punctured and a contrast agent is injected into it through a catheter. The subclavian vein is punctured in exactly the same way during diagnosis.
- MRI, CT, etc.
Surgical treatment of stenosis is considered the most effective
There are 3 methods of treating stenosis: conservative, interventional, surgical. However, surgery is the most effective method of therapy. X-ray endovascular stenting is a surgical procedure performed using local anesthesia. During the procedure, the surgeon makes a miniature incision (about 3 cm) using a puncture to reduce the likelihood of damage and discomfort to the patient. The surgical technique allows you to preserve the original appearance of the vessel, which is important.
This surgical method allows you to expand the artery using catheters and stents that look like balloons.
A stent is an endoprosthesis that is cut from a metal tube. The compressed device is fixed on the balloon catheter and inserted into the vessel. The stent is then inflated under pressure.
Carotid-subclavian shunting is prescribed for patients with below average height and a tendency to be overweight. This is explained by the fact that it is difficult for the doctor to determine the first section of the artery under the collarbone. This operation is also recommended for patients with stenosis of the second section of the arterial vessel under the collarbone.
The following complications may occur after the procedure:
- Injury to peripheral nerves.
- Plexopathy (inflammation of the nerve plexus).
- Dysphagia (difficulty swallowing).
- Swelling.
- Horner's syndrome (damage to the sympathetic nerves).
- Stroke.
- Hemorrhages, etc.
The patient's further condition depends on the general condition and progress of the operation.
Angioplasty and stenting of the subclavian arteries
Subclavian arteries
Subclavian arteries
- These are large vessels that carry blood to both upper extremities.
Rice. Subclavian artery
Atherosclerotic lesions of the subclavian arteries are quite common and can lead to strokes or thrombosis of the arteries of the upper extremities, followed by possible amputation.
Also, with this pathology, the so-called “steal” syndrome, or “steal” syndrome, when blood flows through the vertebral artery into the subclavian artery, after which cerebral ischemia may develop.
About the angioplasty and stenting procedure
Today, the most effective methods of treating severe narrowing of the subclavian arteries are balloon angioplasty and stenting. These are the most gentle and organ-preserving treatment methods that do not require open surgery and anesthesia. The procedure is painless and takes place under local anesthesia. Surgeries allow you to restore the lumen of narrowed arteries using special balloon catheters and stents.
In recent years, isolated angioplasty of the subclavian arteries has been used very rarely, because Stent implantation is almost always more effective.
What is a stent?
Stent
- a cylindrical endoprosthesis, laser cut from a solid metal tube. Subsequently, it is attached to a special balloon catheter, and in a compressed state it moves along the course of the altered subclavian artery.
When the stent is installed in the area of narrowing of the artery, control angiography
to confirm optimal positioning of the stent, and then deploy it under high pressure. In case of incomplete deployment of the stent, angioplasty of the stented area will be performed with a special catheter with a balloon at the end to achieve an optimal result.
Rice. Angiography with stenting of the subclavian artery
Indications and contraindications
Indications
for angioplasty and stenting of the subclavian arteries: symptomatic stenoses (narrowing) more than 50% and asymptomatic stenoses more than 75%. Symptoms of narrowing of the subclavian arteries are weakness in the affected arm, sometimes necrosis of the fingers or gangrene of the hand.
Contraindications:
- total occlusion of the vessel (in relation to the internal carotid artery);
- vascular diseases preventing the use of endovascular instruments
Preoperative examination and preparation
Before you begin treatment for subclavian artery stenosis, you must first diagnose it and confirm the diagnosis. To do this, we use the following research methods:
- Ultrasound diagnostics
- Computed tomography with vessel contrast;
- X-ray of the lungs.
Additionally, general clinical blood and urine tests and biochemical blood tests are performed. It is necessary to perform endoscopy of the stomach to exclude ulcers, since after surgery antithrombotic drugs are prescribed, which can provoke gastric bleeding in case of ulcers.
Where are stenting operations performed in Kyrgyzstan?
Angioplasty and subclavian artery stenting operations are performed in the following clinics:
- MC "Cardio-Asia Plus";
- Research Institute of Heart Surgery and Organ Transplantation;
- Southern Regional Scientific Center for Cardiovascular Surgery (
URRCSS )
These clinics have accumulated a lot of experience in stenting complex lesions of the subclavian arteries, including recanalization of extended occlusions (when the subclavian artery is closed over a long distance).
Prognosis after angioplasty and stenting of the subclavian arteries
After successful angioplasty and stenting of the subclavian artery, the likelihood of re-stenosis is significantly reduced, rapid recovery of the body occurs, and good long-term results are predicted. A huge advantage of these interventions is that there is no need to open the sternum or make an incision in the neck, as when performing bypass and other open operations, but only a small puncture (about 2 mm) at the site of catheter insertion.
Observations after angioplasty and stenting of the subclavian arteries
After this surgical intervention it is recommended:
- Give up bad habits, especially smoking.
- If necessary, control your eating behavior: exclude fatty, smoked, salty foods.
- Lose weight if you are overweight.
- Perform dosed physical activity daily.
- If possible, spend more time in the fresh air.
- Avoid stress!
- Take medications recommended by your doctor.
- Visit your doctor at recommended intervals!
- If you experience any discomfort in your body, consult a doctor.
Is stenting of the subclavian arteries performed in Kyrgyzstan?
In our country, such operations are carried out in several medical institutions. Among them:
- MC "Cardio-Asia Plus"
- NIIHSTO (Research Institute of Heart Surgery and Organ Transplantation).
At NIIHSTO, stenting operations are performed by an experienced cardiac surgeon-arrhythmologist, head of the department of X-ray endovascular surgery, Turdubaev Abay Kubanychbekovich.
Rice. Cardiac surgeon-arrhythmologist Abay Turdubaev
At the Cardio-Asia Plus MC, highly qualified endovascular surgeon Eraliev Talant Kakanovich performs operations.
!! Many operations are performed in our country and now there is no need to travel abroad.
Rice. Endovascular surgeon Talant Eraliev
These medical institutions have everything necessary to perform angiography and stenting. Patients at high risk who seek help prevent the development of stroke, preserve their life and improve its quality.
Artery blockage
Causes and signs of blockage
Occlusion is a pathology characterized by complete blockage of the artery lumen by cholesterol plaques. The disease occurs for the following reasons:
- Atherosclerosis (accumulation of cholesterol plaques on the walls of the vessel).
- Nonspecific aortoarteritis is a rare disease in which the aorta, as well as its large branches (including the subclavian artery), become inflamed and narrowed.
- Endarteritis is a chronic inflammation of the arteries, due to which blood flow is disrupted and gangrene develops.
- Tumors, mediastinal cysts.
- Closure of the lumen of a vessel after injury or embolization (minimally invasive intravascular procedure).
- Complications after surgery on the subclavian artery.
- Congenital anomalies of the arch and branches of the aorta.
With occlusion, the lumen of the subclavian artery is completely blocked by cholesterol plaques
Most often, blockage of the subclavian artery is provoked by atherosclerosis, endarteritis, and nonspecific aortoarteritis. These pathologies are characterized by the formation of fatty plaques or blood clots on the walls of the vessel, which is located near the subclavian vein. After some time, the covering of the cholesterol plaque thickens and enlarges. Due to the blockage of the vessel, blood circulation is disrupted. The entire area for which the subclavian artery is responsible (especially the brain) suffers from a decrease in blood supply.
When a vessel is blocked, patients experience the following symptoms:
- vertigo, headache;
- unsteady gait;
- slight or severe hearing loss;
- uncontrolled oscillatory movements of the eyeballs and other vision disorders;
- numbness or tingling in the hands, muscle weakness;
- blue skin on the upper extremities, the appearance of cracks, trophic ulcers, gangrene develops;
- the patient loses consciousness or is in a pre-fainting state;
- Pain in the back of the head occurs periodically.
Due to a decrease in blood supply to the brain and the risk of thrombosis of its vessels, the likelihood of ischemic stroke increases.
Treatment methods
To eliminate the symptoms of occlusion, it is necessary to restore blood flow in the subclavian artery. The vessel can be reconstructed in the following ways:
- The surgeon removes the inner wall of the vessel affected by cholesterol plaques and replaces the damaged area with an implant.
- Additional blood flow paths are created to bypass the damaged areas of the vessel using grafts (shunt system). For this purpose, aorto-subclavian, carotid-axillary, carotid-subclavian, cross-axillary-subclavian bypass methods are used.
- The subclavian artery is stented, dilated, and ultrasound or laser restoration of the patency of the thrombosed vessel is performed.
The main goal of treatment is to restore blood flow in the subclavian artery
Regardless of the surgical method chosen, treatment may cause complications. Thus, during and after surgery, the likelihood of stroke, damage to peripheral nerves, and disruption of the innervation of the eye muscles increases. In addition, surgical intervention threatens difficulty swallowing, lymphorrhagia (leakage of lymph through damaged vessels), swelling of the brain, and hemorrhage.
Subclavian artery aneurysm
An aneurysm is a limited expansion of an arterial vessel due to damage to its walls. Due to atherosclerosis, vasculitis and other pathologies that disrupt the structure of the vessel, a certain section of the artery protrudes under blood pressure.
An aneurysm is manifested by the expansion of a section of the subclavian artery as a result of damage to its walls.
In most cases, an aneurysm occurs as a result of fractures, wounds, etc. After injury, blood accumulates in the tissues, a hematoma is formed, and as a result, the likelihood of developing a false aneurysm, which grows rapidly, increases. As its size increases, it compresses nearby tissues, causing pain in the arm and impairing blood circulation. In addition, a disorder of innervation occurs in the upper limb.
The main complication in this case is the rupture of the aneurysm and arterial hemorrhage, which often ends in the death of the victim. Also, due to impaired blood flow in the aneurysmal cavity, the likelihood of thrombus formation increases. These complications provoke obstruction of the artery, disturbances in the blood supply to the arm (pulsation slows down, the arm swells, the skin on the limb becomes pale bluish).
An aneurysm is a source of emboli (intravascular substrate that causes blockage of an arterial vessel), which provoke arterial insufficiency. Due to an acute circulatory disorder, severe pain in the arm occurs, numbness occurs, the patient cannot move the limb normally, it swells and turns pale. If left untreated, the likelihood of developing gangrene increases.
To treat aneurysms, surgery is prescribed. However, recently they are increasingly resorting to low-traumatic methods of endovascular surgery.