Post-infarction cardiosclerosis (PICS) is an independent form of coronary heart disease (CHD). It is characterized by the formation of connective tissue in the heart muscle, replacing dead cardiomyocytes due to myocardial infarction (MI). This tissue cannot perform the functions of muscle cells of the heart, which is accompanied by dysfunction of the organ.
ABC Clinic provides highly specialized cardiac surgery medical care. Doctors of the highest category work here, who, using innovative high-tech equipment, conduct thorough diagnostics and perform operations of any level of complexity.
Symptoms of post-infarction cardiosclerosis
Symptoms of post-infarction cardiosclerosis include deterioration in pumping function, rhythm disturbances, conduction disturbances, enlargement of the heart chambers, hypertrophy of muscle tissue with the development of heart failure.
Clinically, this is manifested by tachycardia, shortness of breath, fatigue, attacks of suffocation, orthopnea, swelling of the legs, acrocyanosis, hepatomegaly, pericarditis, swelling of the neck veins, and chest pain. The larger the volume of newly formed tissue, the more intense the symptoms.
Symptoms
Manifestations of the disease depend on the location of scar formation, the width and depth of the affected area of the heart. The less intact myocardium remains, the more likely the occurrence of arrhythmias and heart failure.
Post-infarction cardiosclerosis has the following symptoms, common to all cases:
- Dyspnea. Appears both during physical activity and during rest. While in a horizontal position, the patient feels breathing problems. The attack passes 15-20 minutes after taking a sitting position.
- Increased heart rate. Develops due to acceleration of blood flow and contraction of the myocardium.
Blue discoloration of limbs and lips. Occurs due to lack of oxygen.- Discomfort and pain in the chest. The pain may be pressing or stabbing.
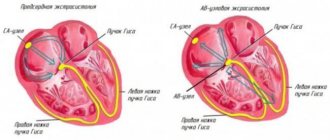
- Heart rhythm disturbance (arrhythmia). Manifests itself in the form of extrasystole and atrial fibrillation. The cause of its appearance is sclerotic deformation of the pathways.
- Swelling. It is provoked by the accumulation of excess fluid in the body cavity and right ventricular failure. Mostly observed in the lower extremities.
Additionally, the following may appear:
- constant fatigue and weakness of the body;
- dizziness;
- fainting;
- feeling of lack of air;
- increased blood pressure;
- increased liver size;
- dilatation of the neck veins.
Depending on the severity of the disease, the level of intensity of unpleasant and painful sensations differs. At the beginning of the disease or at the stage of remission, there may be no symptoms at all. After the formation of a lesion, the structure of the entire myocardium may change. In this case, the symptoms appear more clearly.
Types of post-infarction cardiosclerosis
Based on the size and location of the pathological focus, doctors classify this condition into the following types:
- Large-focal post-infarction cardiosclerosis (significant replacement of cardiomyocytes with connective tissue).
- Atherosclerotic (not a type of PICS, its cause is atherosclerosis of the coronary arteries, as a result of which the heart muscle experiences oxygen deficiency, cells are gradually damaged and replaced by connective tissue).
- Lower (damage to the lower wall of the heart, accompanied by dyspeptic disorders; sometimes involvement of the right ventricle in the pathological process is observed).
Consequences
A patient with the diagnosis in question needs lifelong medical supervision. Knowing what post-infarction cardiosclerosis is, one cannot ignore the situation, as this leads to inevitable complications in the form of the following consequences:
- Diffuse cardiosclerosis: symptoms, treatment tactics, preventive measures
- pericardial tamponade;
- atrial fibrillation;
- thromboembolism;
- blockades;
- pulmonary edema;
- tachycardia;
- decreased automaticity of the sinoatrial node.
These processes negatively affect a person’s quality of life. The patient loses tolerance to physical activity, loses the opportunity to work and lead a normal life. Advanced cardiosclerosis provokes the appearance of an aneurysm, the rupture of which leads to death in 90% of non-operated patients.
Diagnosis of post-infarction cardiosclerosis
Diagnosis of post-infarction cardiosclerosis includes:
- Anamnesis collection.
- ECG.
- Echocardiography.
- RKG.
- PET of the heart.
- Coronography, etc.
ECG is the most common and simplest method for detecting PICS. He clarifies the presence and location of scars; affected area; associated cardiac changes; rhythm and conduction disturbances; signs of an aneurysm. Post-infarction cardiosclerosis on the ECG has a distinctive feature - a deep Q wave.
But PICS is not always reflected in the conclusion of this survey. Therefore, differential diagnosis of postmyocardial cardiosclerosis is carried out using other methods.
EchoCG is highly informative for PICS. The study can detect cardiac aneurysm (chronic form), increased volume of the left ventricle, and impaired contractility.
Cardiac PET can identify persistent areas of hypoperfusion. Coronography makes it possible to evaluate coronary blood flow. In this case, an X-ray contrast study can show a fairly variable picture: both unchanged coronary arteries and three-vessel lesions.
Dibikor in the clinic: cardiology
This section brings to your attention the results of the clinical use of Dibikor
in medical centers of Russia
Experience of using taurine at the stage of rehabilitation of patients after cardiac surgery
Averin E. E. “Heart Failure” Vol. 15, No. 4 (85), 2014
The increasing availability of high-tech care such as cardiac surgery exacerbates the problems of rehabilitation of patients after surgery. The search for new drugs and methods for successful rehabilitation of patients is a promising direction in the development of restorative medicine.
In the course of the work, the effect of taurine on the main clinical, instrumental, laboratory and psychological indicators in patients after cardiac surgery during the rehabilitation stage was determined.
Materials and methods
.
The study included 48 patients with CHF aged from 21 to 62 years. The groups of patients with CHF of ischemic etiology who took and did not take taurine after coronary artery bypass surgery (CABG) included 12 men each. The groups of patients with CHF caused by acquired heart defects, who were prescribed or not prescribed taurine after heart valve replacement, also included 12 patients. Taurine (Dibikor, PIK-PHARMA LLC, Russia) was prescribed at a dose of 250 mg 2 times a day for 3 months. All patients underwent a clinical examination, their well-being, activity and mood were assessed using the Well-Being-Activity-Mood (WAM) questionnaire and quality of life (QOL) using the Minnesota Living with HF Questionnaire, ECG, EchoCG, and blood tests were performed.
Results
.
In groups of patients after heart valve replacement and CABG who took taurine, LVEF significantly increased and LV myocardial mass index (LVMI) and TG levels in the blood decreased.
In both groups of patients taking taurine, QoL significantly improved. According to the results of the SAN test, in the groups of patients who used taurine in therapy, indicators of well-being, activity and mood increased. See full article
Organoprotective and metabolic effects of taurine in the treatment of patients
with chronic heart failure and type 2 diabetes mellitus
Statsenko M. E. Shilina N. N. Vinnikova A. A. CONSILIUM MEDICUM, | 2014, VOLUME 16, No. 3, pp. 6-11
The purpose of the study was to study the effect of taurine as part of the basic therapy of CHF and type 2 diabetes on the severity of heart failure, structural and functional parameters of the heart, heart rate variability (HRV), functional state of the kidneys, liver, elastic properties of blood vessels, IR, carbohydrate and lipid metabolism.
- The inclusion of taurine in the basic therapy of CHF and type 2 diabetes significantly increases exercise tolerance and reduces the FC of CHF, helps reduce the level of Nt-proBNP and significantly increases LVEF, and leads to a decrease in the activity of the sympathetic division of the autonomic nervous system.
- Administration of taurine to patients with CHF and type 2 diabetes significantly reduces the severity of albuminuria, promotes the growth of GFR and has a hepatoprotective effect, reducing the activity of enzymes of the cytolysis and cholestasis syndrome.
- The addition of taurine to the basic therapy of patients with CHF and type 2 diabetes helps to significantly reduce the stiffness of the vascular wall of the main arteries and significantly improves endothelial function.
- Sixteen-week taurine therapy in patients with CHF and type 2 diabetes has beneficial effects on carbohydrate and lipid metabolism: it significantly reduces fasting glucose levels, HbA1c, IR, and also reduces LDL and TG levels.
See full article
Taurine in the treatment of chronic heart failure and type 2 diabetes mellitus: effect on microcirculation and elastic properties of great vessels
Statsenko M. E. Vinnikova A. A. Ronskaya A. M. Shilina N. N. Heart Failure 2013 Vol. 14, No. 6 (80), pp. 347-353
Relevance
. The high incidence of CHF and type 2 diabetes, poor prognosis and low quality of life of patients determine the relevance of selecting optimal therapy. The most important direction of treatment for this category of patients is the correction of metabolic disorders that underlie the development and progression of CHF and diabetes: lipid and glucose toxicity, insulin resistance. Target. To study the effects of the use of taurine as part of combination therapy for CHF and type 2 diabetes, taking into account its effect on the elasticity of large vessels and the microvasculature.
Materials and methods.
Included were 60 patients in the early post-infarction period (3–4 weeks from the onset of MI) with class II–III CHF and concomitant type 2 diabetes, who were divided into two groups of 30 people: 1 (control group) – patients receiving basic therapy HF in the post-infarction period and oral hypoglycemic agents, and 2 (experimental group) - patients taking taurine (Dibikor, PIK-FARMA, Russia) in addition to the main treatment of CHF and type 2 diabetes in a dose of 500 mg 2 times a day. The examination of patients included a 6-min walking test, determination of blood levels of Nt-proBNP, glucose, insulin, glycated hemoglobin, total cholesterol, LDL, HDL, TG, GFR, echocardiography, and microcirculation parameters.
Results.
It has been shown that taking taurine for 16 weeks leads to an improvement in microcirculation parameters, most pronounced in patients with a spastic type of microcirculation. There was a redistribution of microcirculation types in favor of normocirculation as a result of taurine therapy. A positive effect of taurine on the elastic properties of great vessels has been established, an improvement in endothelial function, lipid and carbohydrate metabolism, and a decrease in insulin resistance have been noted.
Conclusion.
It is advisable to include taurine in the basic therapy of CHF and type 2 diabetes in patients in the early post-infarction period.
See full article
The effect of taurine on the incidence of cardiac arrhythmias and QT interval dispersion in patients with heart failure due to post-infarction cardiosclerosis: results of a comparative, randomized study
Gordeev I.G., Pokrovskaya E.M., Luchinkina E.E. Cardiovascular Therapy and Prevention, 2012; 11(1): 65-70
Target
. To study the effect of taurine therapy on the incidence of cardiac arrhythmias and QT interval dispersion in patients with chronic heart failure (CHF) due to post-infarction cardiosclerosis (PICC).
Material and methods
. The study included 40 patients who had myocardial infarction (MI) with left ventricular ejection fraction (LVEF)
conclusions
- The use of taurine in patients with NYHA FC II CHF caused by PICS leads to a significant decrease in dQT; in patients with NYHA FC III CHF caused by PICS, it has a positive effect on the dynamics of this indicator.
- The use of taurine in patients with NYHA class II CHF and PICS can significantly reduce the number of ventricular dysrhythmias and supraventricular arrhythmias according to CM ECG data.
- The addition of taurine to patients with NYHA class III CHF against the background of PICS can significantly reduce the number of CVDs according to CM ECG data and has a positive effect on supraventricular arrhythmias in this group of patients.
- It is advisable to include taurine in the complex treatment of patients with NYHA class II and III CHF after MI in order to reduce cardiac arrhythmias and prevent fatal arrhythmias.
See full article
Taurine deficiency in Russia and its consequences. Effects of Dibikor in the clinic
Elizarova E.P., Doskina E.V. Directory of a polyclinic doctor 2011, No. 8, p. 16-19
Since the Russian population is deprived of foods rich in taurine, Dibikor® can solve the problem of taurine deficiency in the diet. Dibikor's lack of side effects and contraindications and compatibility with other drugs makes it indispensable when added to therapy for a number of diseases associated with metabolic disorders.
See full review
Efficacy and tolerability of taurine in patients with type 2 diabetes mellitus and left ventricular diastolic dysfunction
Nechaeva G. I, Ryapolova E. A, Druk I. V. Attending physician 2011, 11
Diastolic dysfunction (DD) is recorded in patients with type 2 diabetes mellitus (T2DM) without concomitant cardiovascular pathology in 50–75% of cases and is considered by researchers as a manifestation of diabetic cardiomyopathy.
Increased taurine intake has been shown to inversely correlate with the prevalence of coronary heart disease (CHD). According to an epidemiological study by Yamori et al. (2001), the level of taurine excretion, as an indicator of the level of its consumption, inversely correlates with mortality from coronary artery disease. According to some data, plasma levels of taurine in patients with diabetes are lower than in the general population.
In order to study the effect of taurine (Dibikor) on the state of carbohydrate metabolism and lipid metabolism, the state of the cardiovascular system, clinical status and quality of life indicators of patients suffering from type 2 diabetes, 195 patients were examined. The placebo-controlled, double-blind study included 80 patients with an established diagnosis of type 2 diabetes in accordance with the inclusion criteria (previously diagnosed type 2 diabetes; patient age 45–60 years
The use of the drug Dibikor while taking hypoglycemic, lipid-lowering, antihypertensive drugs, following recommendations regarding lifestyle (diet, physical activity) contributes to a significant improvement in the subjectively assessed clinical status of patients, a decrease in BW, an improvement in carbohydrate and lipid metabolism, a moderate decrease in blood pressure and heart rate , improving the process of myocardial repolarization and diastolic function of the left ventricle with a significant positive effect on the quality of life of patients with good tolerability of the drug.
In the group of patients with type 2 diabetes and left ventricular DD, a course (16 weeks) use of the drug Dibikor is preferable in order to have a positive effect on the clinical status, indicators of carbohydrate and lipid metabolism, blood pressure levels, and diastolic heart function. See full article
Use of the drug Dibicor in adolescents with arterial hypertension
Ledyaev M.Ya., Zhukova V.B., Ananyeva Y.A. Systemic hypertension 2011, No. 4, p. 64-68
4-week therapy of hypertension I in adolescents with Dibicor at a dose of 750 mg per day orally in three doses led to a decrease in the average daily, average daytime and average night-time SBP. Therapy with Dibicor after 2 weeks led to a decrease
hypertensive SBP load during the day (decrease in SBP IV), normalized the daily SBP profile (SI SBP) and reduced SBP variability according to ABPM data. Dibikor reduces arterial tone after 2 weeks. therapy. The use of Dibikor in adolescents with stage 1 hypertension reduces the level of reactive anxiety. See full article
Optimization of arterial hypertension therapy in pregnant women
Zakharov I.V. Issues of gynecology, obstetrics and perinatology, 2010, vol. 9, no. 5, p. 10–13
The purpose of this study was to optimize the pharmacotherapy of arterial hypertension (AH) in pregnant women by including the original Russian drug Dibikor® in treatment regimens, taking into account its effect on the daily blood pressure profile, the quality of life of pregnant women and the absence of negative effects on uteroplacental and fetal blood flow. The study included 90 pregnant women aged 18–40 years with mild to moderate hypertension, divided into 4 comparison groups. The patients underwent a comprehensive assessment of the state of the cardiovascular system and fetoplacental blood flow.
It was found that all the studied drugs contributed to the improvement of ABPM indicators. It has been proven that the combination of Dibikor with dopegyt in pregnant women with hypertension is superior to the effectiveness of dopegyt monotherapy. It was concluded that it is advisable to use Dibikor for the treatment of hypertension of mild and moderate severity, for the prevention of complications during pregnancy and childbirth in women suffering from hypertension. See full article
Dependence of the severity of the disaggregation effects of Dibikor on its plasma concentrations in patients with type 2 diabetes mellitus
Rogova N.V. Bocharnikov A.A. Bulletin of VolSMU, 2008, 1(25), 45-48
The study showed that Dibikor, used in the treatment of diabetes, has pronounced activity. A linear relationship has been established between the concentration of Dibikor and the severity of its disaggregation effect. Treatment with Dibikor led to the elimination of spontaneous aggregation and a statistically significant decrease in blood viscosity. All patients treated with Dibicor achieved compensation of carbohydrate metabolism. See full article
Experience of clinical use of taurine and trimetazidine in chronic heart failure in perimenopausal women
EM. Sedova, O.V. Magnitskaya. CARDIOLOGY (KARDIOLOGIIA), 1, 2010, p. 66-67
Treatment of heart failure is one of the most important problems in clinical cardiology. The risk of developing coronary heart disease (CHD) in women before menopause is 2-4 times less than in men of the same age, but then it increases exponentially and at the age of 60-70 years is compared with the risk in men]. When assessing the risk of developing heart pathology, it is necessary to take into account the peculiarities of the pathophysiology of the female body. Approaches to therapy should be different for men and women. Little has been studied about the use of drugs with pronounced metabolic activity in the treatment of women with chronic heart failure (CHF). See full article
The use of dibikor in elderly and senile patients with chronic heart failure
Pustozerov V.G. Bazhenova Yu.V. Maslova E.G. Practical geriatrics: conference materials, February 11, 2010, Irkutsk / ed. F.I.Belyalova, Yu.S.Chaikisova. Irkutsk, 2010. p. 52.
Chronic heart failure (CHF) is a common cause of death in older people. The risk of sudden death in patients with CHF is 5 times higher than in the general population. In Russia there are more than 3 million patients with severe CHF. The number of hospitalizations due to decompensation of CHF is 43.6-45.4% (EPOCHA-CHF study 2006). Against the background of multimorbid pathology, CHF significantly reduces the quality of life of patients and tends to increase in prevalence in elderly and senile people.
The purpose of the study was to study the effectiveness of taurine (dibikor), which is a unique corrector of metabolic processes. We used Dibicor in the complex treatment of elderly patients with CHF. A group of patients with CHF was examined: 40 people (group 1) aged from 60 to 94 years (27 women and 13 men). The average age of patients with CHF stages 1,11,111 was 74.2+2.4 years. Dibikor was prescribed 0.5 g twice a day for 1 month.
The results were compared with a group of patients (group 2) representative by gender and age who received basic therapy for CHF. Before and after treatment, all patients in groups 1 and 2 underwent an ECG, an echocardiogram, an exercise test (6-minute walk), a CMECG in patients with cardiac arrhythmias, and general clinical and biochemical blood tests were examined.
In the 1st group of patients receiving Dibicor, an improvement in subjective and objective condition was noted. The stage of CHF was significantly changed downwards in 9 patients 22.5% (R
Conclusion. The use of Dibicor in the elderly in combination with basic therapy improves metabolic processes in the myocardium. Improves hemodynamics and parameters of myocardial contractility in CHF. Improves the quality of life in elderly and senile patients with CHF. Dibikor can be used in the complex treatment of CHF in elderly patients, as an auxiliary drug.
Possibilities for correcting disorders of carbohydrate metabolism and daily blood pressure profile in patients with chronic heart failure and metabolic syndrome
A.S. Adamchik, I.V. Kryuchkova. PHARMATEKA No. 15 - 2009, p. 81-85
The results of a study assessing the effect of the drug Dibicor (taurine) on carbohydrate metabolism, insulin resistance (IR) and 24-hour blood pressure monitoring (ABPM) parameters in patients with metabolic syndrome (MS) and chronic heart failure (CHF) are presented. The study included 65 people aged 31–66 years. In the main group, Dibikor was added to therapy with enalapril and indapamide. While taking Dibikor, a predominance of positive dynamics was noted in terms of anthropometry, carbohydrate metabolism, IR and ABPM. Thus, the use of Dibikor in the treatment of patients with MS and CHF significantly improves their carbohydrate status, reduces the severity of IR, and contributes to a more effective correction of existing disorders of daily blood pressure. See full article
Possibilities for correcting carbohydrate metabolism disorders in metabolic syndrome
Adamchik A.S. Kryuchkova I.V. Russian Journal of Cardiology, No. 2, 2009
The work was carried out to assess the effect of the drug Dibicor on carbohydrate metabolism (CM), insulin resistance (IR) in patients with metabolic syndrome (MS), to identify correlations between CB indicators, chronic heart failure (CHF) and abdominal obesity (AO).
Under the conditions of voluntary informed consent, the study included 60 people aged 31–66 years, men – 21.7%, women – 78.3%. There were 2 groups of 30 people each. In the main group, dibicor was added to therapy. Everyone underwent an anthropometric examination, blood pressure measurement, determination of lipid and carbohydrate status and the severity of IR.
While taking Dibicor after 12 months, there was an improvement in SV indicators and a decrease in the severity of IR. A pronounced positive correlation was revealed between the functional class (FC) of CHF and the degree of SV impairment; AO with plasma glucose levels on an empty stomach and after a glucose load.
The use of dibicor for MS and CHF significantly improves carbohydrate status and reduces the severity of IR. Correction of these disorders helps to reduce the FC of CHF.
See full article
Site search
What should I do if I have a similar but different question?
If you did not find the information you need among the answers to this question, or your problem is slightly different from the one presented, try asking an additional question to the doctor on the same page, if it is related to the topic of the main question. You can also ask a new question and after a while our doctors will answer it. It's free. You can also search for the information you need in similar questions on this page or through the site search page. We will be very grateful if you recommend us to your friends on social networks.
Medical portal 03online.com
provides medical consultations via correspondence with doctors on the website. Here you get answers from real practitioners in your field. Currently, you can consult an allergist on the website. venereologist. gastroenterologist. hematologist. genetics. gynecologist. homeopath. dermatologist. pediatric surgeon. nutritionist. immunologist. infectious disease specialist cardiologist. cosmetologist. speech therapist Laura. mammologist. narcologist. neurologist. orthopedist-traumatologist. ophthalmologist. pediatrician plastic surgeon. proctologist psychiatrist. psychologist. pulmonologist. sexologist-andrologist. dentist urologist. herbalist. surgeon endocrinologist.
Poem about a lighter (Full text)
Treatment and rehabilitation
Treatment of cardiac cardiosclerosis is aimed at reducing the risk of complications, normalizing heart function and blood circulation, and improving the patient’s quality of life.
An integrated approach can be used for this:
- Non-drug post-infarction treatment of the post-infarction condition (regular, but not too intense physical activity, giving up bad habits, proper nutrition with limited animal fat, body weight control).
- Treatment of post-infarction cardiosclerosis with drugs (ACE inhibitors, nitrates, beta-blockers, antiplatelet agents, diuretics, etc.)
- Operation. In case of severe lesions and conduction and rhythm disturbances, an ICD or pacemaker is sometimes necessary. If indicated, CABG, stenting or angioplasty of the coronary arteries is performed. In case of an aneurysm, its removal in combination with CABG is necessary.
- Psychotherapy. Not all patients are ready to change their lives when they learn about the diagnosis. In this regard, it is important that the patient realizes that the duration and course of the disease depend on the lifestyle. This may require psychotherapeutic help.
- Dispensary observation. With PICS, the patient must be observed by a cardiologist for at least a year. It is recommended to do an ECG every month for six months after diagnosis.
Six months later, the patient is sent to MSEC to determine his ability to work. You will first need an ECG, stress test, and echocardiography. Also pass a series of tests: general, biochemistry. Subsequently, electrocardiography must be repeated every year.
Diagnostic procedures
A patient who has suffered a myocardial infarction must be constantly under medical supervision. When the symptoms described above appear, the diagnosis is beyond doubt. The following studies are used to make a diagnosis:
- ECG. Shows disturbances in the functioning of the heart, myocardial defects and contractility disorders.
EchoCG. Deciphering the results of this study is most valuable. Demonstrates the location, the volume of replaced tissue, and also allows you to count the number of ventricular contractions and determine the presence of aneurysmal dilatations.- Radiography. Makes it possible to see the size of the heart and determine whether it is enlarged.
- Scintigraphy. The patient is injected with radioactive isotopes that reach only healthy areas of the myocardium. This allows you to see the microscopically sized affected areas.
- Angiography. Allows you to determine the degree of narrowing of blood vessels and the presence of blood clots in them.
- MRI. Determines the location and size of connective tissue in the myocardium.
The cardiologist needs to carefully examine the patient’s medical history and conduct a detailed interview. An assistant in determining the diagnosis will be the patient’s medical record, which records all the diseases suffered during life. This allows you to predict future complications and prevent them.
Is disability issued to patients after post-infarction cardiosclerosis?
Not everyone gets a disability. Much depends on the general health of the patient and the presence of complications caused by the pathology. To determine the group, the following factors are taken into account: angina pectoris, which is confirmed by electrocardiography data; features of rhythm disturbances (constant, episodic); aneurysm with thrombosis, also confirmed by echocardiography.
The cardiology department of the ABC Clinic deals with the diagnosis and treatment of pathological changes in the heart muscle, vessels of various sizes, and the valve apparatus. Modern equipment makes it possible to detect diseases at an early stage of development, which makes it possible to prevent the development of complications. In their work, doctors are guided by the principles of evidence-based medicine, recommendations of the Russian Ministry of Health, and their own clinical experience.
Prevention
No methods of prevention have been developed as such. It is enough to adhere to clinical recommendations that are common to all risk groups for developing cardiovascular pathologies.
- Refusal of bad habits and behavioral stereotypes. Smoking, alcohol, drugs will sooner or later play a cruel joke.
- Normalization of the rest regime. Approximately 8-9 hours per night. Not worth it anymore.
- Salt no more than 7 grams per day.
- Regular examinations with a cardiologist. Once a year. If the patient is at risk - every 6 months.
- Hiking. No sports or excessive physical activity.
- Stress and overheating are eliminated.
- Proper nutrition.
- Timely treatment of conditions that can lead to a heart attack. For example, atherosclerosis, arterial hypertension and others.