Issues discussed in the material:
- What is cerebral ischemia in the elderly
- What are the symptoms to understand that treatment for cerebral ischemia in the elderly is required?
- How is cerebral ischemia diagnosed in the elderly?
- What are the consequences of untimely treatment of cerebral ischemia in older people?
When the vessels no longer allow the required amount of blood to pass through, an elderly person develops cerebral ischemia. The process is gradual and imperceptibly develops into a chronic form, but sometimes it also manifests itself in an acute form. Tissues and internal organs begin to lack oxygen and other nutrients that reach them through the blood. In this article we will talk about the treatment of cerebral ischemia in the elderly.
Symptoms of cerebral ischemia in the elderly
There are several symptoms of cerebral vascular ischemia: from mild dizziness to loss of consciousness. It depends on the form and degree of development of the disease.
Particular attention should be paid to the acute form of the disease. It manifests itself instantly as soon as a serious disruption of the blood supply to the brain tissue occurs. The acute form is considered to be transient ischemic attack (TIA) and ischemic stroke. Exacerbation of cerebral vascular ischemia can be caused by an advanced form of the disease or an embolus that has blocked the vessel. In the latter case, the blood clot can also provoke serious inflammation.
If the microscopic damage covers a small area, doctors diagnose transient cerebral ischemia, sometimes called a ministroke. In this case, the blood supply deteriorates for only 1-2 minutes, this time is not enough for the neurons to die completely. An elderly person is most often referred for treatment to a neurologist. Deterioration of the brain appears less frequently, leaving no consequences. Within 24 hours the patient’s health is restored.
Symptoms of ischemic attack:
- numbness of the limbs, acquiring a white tint to the skin;
- strong pulsation in the head;
- the appearance of red spots on the face;
- speech dysfunction;
- sudden deterioration of vision;
- feeling of weakness in the arms and legs;
- impaired coordination of movements;
- loss of consciousness;
- pain in the heart area;
- paralysis of an area or half of the body.
It is not at all necessary that all symptoms will be present at the time of the attack. The manifestation of any condition depends on which part of the brain the damage is recorded. With such pronounced symptoms, the disease is still reversible. After several minutes of a sharp deterioration in well-being, blood flow is restored, neurons are activated, and the attack passes. Within a week after the onset of acute cerebral vascular ischemia, the condition of the elderly patient’s body returns to normal without mandatory treatment.
If by the end of the day the ischemia continues to remain acute, and the symptoms even intensify, then the doctor diagnoses an ischemic stroke. Signs of the disease indicate significant damage to brain cells.
They stop receiving oxygen as the blood supply continues to deteriorate. Neurons die and tissue necrosis occurs. Six minutes are enough for the process to become irreversible; in this case, the neurons will not recover. As a result of the resulting neurological deficit, various types of dysfunction begin to appear in the body of an elderly person. Therefore, it is necessary to treat chronic cerebral ischemia in the elderly in order to prevent such situations.
The acute form of the disease also requires timely diagnosis and medical supervision. Especially with symptoms of coronary artery disease such as loss of consciousness, sensitivity in any part of the body, paralysis, blurred vision and speech, breathing problems, sudden changes in blood pressure. Each of these manifestations can be a sign of an ischemic stroke, so urgent medical attention and subsequent treatment are extremely important for an elderly patient. Any delay can lead to tragic consequences.
Recommended articles on this topic:
- Features of older people: psychological and physiological
- The main problems of older people and ways to solve them
- Boarding home for the elderly: features and rules of choice
Chronic obliterating diseases of the arteries of the lower extremities (COLD) is one of the most common cardiovascular diseases in the population. The prevalence of intermittent claudication (IC) depending on age varies from 0.9 to 7.0% with an increase in older age groups: 1-5% in people under 50 years of age, 10-14% among people aged 50-70 years ( J. Dormandy et al., 1989; M. Criqui et al., 1992). Surgical methods for treating COZANK continue to develop rapidly, and the share of X-ray endovascular interventions is constantly growing. In Russia, due to insufficient provision of the population with specialized angiosurgical care, only a small proportion of patients with chronic lower limb ischemia (CLI) receive it. Most of these patients are patients of general, and primarily outpatient, surgeons. The initial request for medical help occurs when a clinical diagnosis of PC appears, which corresponds to degrees IIA-IIB of ischemia according to the Pokrovsky-Fontaine classification and reduces the quality of life of patients.
It should also be noted the high frequency (45-65 cases per 100 thousand population, according to Catalano, 1993) of the development of critical lower limb ischemia (CLI). The reason for this is the insufficiently high effectiveness of conservative therapy and prevention of progression of chronic arterial insufficiency. As a result, within 1 year after the diagnosis of CLI, major amputation of a limb is performed in 25-30% of cases (Pokrovsky, 2013). Within 5 years after the primary amputation, death occurs in 70% of cases (Riffel, 2009).
Taking these data into account, the need to improve the conservative element of treatment for patients with CLI should be recognized. In particular, it is necessary to introduce modern treatment methods and develop prevention of progression of the underlying disease in the practice of an outpatient surgeon.
Modern methods of non-surgical treatment of chronic ischemia of the lower extremities
Correction of risk factors. Healing Fitness
The basis of conservative treatment of peripheral arterial diseases are measures aimed at correcting risk factors (tobacco smoking, arterial hypertension (AH), diabetes mellitus, hyperlipidemia, hyperhomocysteinemia), and therapeutic physical education (PT). According to the 2021 ESC Guidelines on the Diagnosis and treatment of Peripheral Arterial Diseases, In Collaboration with the European Society for Vascular Surgery (ESVS), the basis for the treatment of intermittent claudication (IC) should be smoking cessation together with daily exercise therapy (the best effect is shown by dosed walking) [1].
Up to 80% of patients with CLI are smokers [2]. Quitting smoking may help prevent progression of the disease. Smoking after bypass surgery increases the risk of postoperative bypass thrombosis by at least 3 times [3].
In addition to smoking, the level of cholesterol in the patient’s blood plays an important role. All patients with peripheral artery disease should receive statins regardless of blood lipoprotein levels. This conclusion is based on the Heart Protection Study (20,536 patients, of which 6,748 had COPD), which showed that the risk of coronary circulatory disorders in the group taking statins (simvastatin 40 mg) was reduced by 22% compared with the placebo group [4]. Statins should definitely be included in the treatment of PC (level of evidence IA). In addition to the fact that lipid-lowering therapy significantly reduces the risk of developing cardiac complications, several meta-analyses have shown a positive effect of statin use on pain-free walking distance (PDW) and maximum walking distance (MPD) [5, 6].
In patients with peripheral arterial disease, it is also necessary to correct arterial hypertension. The target blood pressure values are 140/90 mmHg, and if the patient has diabetes mellitus and chronic kidney disease or is under 60 years of age - 140/85 mmHg. [1, 7]. Among antihypertensive drugs, preference should be given to blockers, angiotensin II receptors and angiotensin-converting enzyme inhibitors due to the peripheral vasodilating effect of these drugs. β-Blockers are not included in the first-line drugs for the treatment of hypertension; they are used to prevent myocardial infarction (MI) and atrial fibrillation.
One of the most significant risk factors is disorders of carbohydrate metabolism in the body, namely diabetes. Patients with COPD and diabetes mellitus require reasonable and comprehensive treatment. For many years, the target values for glycated hemoglobin were considered to be 7% and below, but recently there is a growing consensus that an individual approach to each patient is necessary [8].
Obesity plays an important role in the progression of ischemia. It is noted that in patients with COPD, normalization of body weight can potentially increase DBC [9].
Exercise therapy is one of the most effective methods of treating P.H. According to the ESVS, dosed exercise therapy should be recommended for patients with CLI (level of evidence IA). There have been studies comparing exercise therapy with other forms of treatment. When compared with antiplatelet therapy, the maximum walking time in the exercise therapy group after 6 months increased by 86%, while in the group taking antiplatelet drugs only by 38%. No differences were found in the ankle-brachial index (ABI) and peak blood flow of the leg [10].
Drug treatment
The basis of conservative treatment of cardiovascular diseases in general and peripheral arterial diseases in particular is the use of antiplatelet agents. Taking aspirin has been shown to significantly reduce the risk of MI, stroke, or death (Level of Evidence IA) (Antitrombotic Trialists' Collaboration, n
=135,000). In the group of patients with COPD, taking aspirin in various dosages reduced the risk of the above events by 22%. According to the ESVS, patients with symptomatic peripheral arterial disease should receive antiplatelet agents (clopidogrel or aspirin) long-term (Evidence Level IA) [1]. It is not yet possible to talk about the advantage of dual antiplatelet therapy over aspirin monotherapy as a preventive measure for the development of cardiovascular complications in patients with CLI due to a lack of information [11]. In the group of patients receiving dual antiplatelet therapy, a decrease in the incidence of myocardial infarction was noted compared to the group of patients receiving exclusively aspirin, but an increase in the number of “major”, including fatal, bleedings was also noted.
After interventions on the vessels of the lower extremities, patients are recommended to take aspirin (evidence level IA) [1]. According to some researchers [1], instead of aspirin as an antiplatelet agent in the treatment of patients with CLI, clopidogrel should be used, in particular in cases of intolerance to acetylsalicylic acid (evidence level IIB). According to the results of the ECLID study ( n
=13,885), which compared the effectiveness of clopidogrel and ticagrelor in relation to the development of cardiovascular complications and bleeding, no significant differences were obtained in the study groups [12]. GPIIb/IIIa receptor antagonists (the most commonly used is integrilin) have not shown significant benefit in patients with atherosclerosis of the arteries of the lower extremities [13].
One of the main drugs that relieve PC is pentoxifylline. This is a vasodilating drug with an additional antiplatelet effect, mainly affecting the microcirculation. The antiplatelet effect is secondary, so it is possible to prescribe pentoxifylline in combination with other antiplatelet agents and antiplatelet drugs [14]. Pethoxifylline is a first-line drug not only in the Russian Federation, but also in many countries around the world: in the United States, for many years, pentoxifylline was the only drug approved by the FDA for the treatment of peripheral artery disease. A significant number of studies confirm the positive effect of pentoxifylline on DBC and IVD [15].
Many studies have been conducted that compared the effectiveness of various drugs and treatment methods with pentoxifylline therapy: when compared with exercise therapy, after 13 weeks the maximum walking time increased in the pentoxifylline group by 88% versus 62% in the exercise therapy group [16]. Iloprost showed worse results than pentoxifylline [17], and when comparing alprostadil with pentoxifylline, the differences in MTD and DBC were insignificant [18]. When comparing the effectiveness of bufomedil, pentoxifylline and nifedipine based on the results of a 90-day study, it was concluded that nifedipine had the best effect in the treatment of PC, followed by pentoxifylline and the least - bifomedil [19]. When taking pentoxifylline, patients developed dyspeptic symptoms, headache, pharyngitis, and pain in the extremities. But at the same time, in the groups taking placebo, the appearance of the same complaints was also noted, so one should not assert a direct connection between pentoxifylline and these complications.
In world practice, one of the main drugs for the treatment of PC is cilostazol (trade name “Pletal”), a phosphodiesterase-3 inhibitor that has an antiplatelet and antiplatelet effect [20]. In addition, cilostazol has a vasodilating effect and has a positive effect on the concentration of triglycerides and high-density lipids [21]. A contraindication to taking cilostazol is primarily the presence of chronic heart failure, liver and kidney failure in the patient [21, 22]. The recommended dose of cilostazol for PC is 100 mg 2 times a day, however, many studies have been conducted with different dosages of the drug. When taking the recommended dose of cilostazol, many studies have shown an undeniable positive effect on the clinical manifestations of CLI [23-28]: the average increase in IVD compared to the placebo group was 43.11 m (from 18.27 to 67.9 m). The effect on ABI cannot be considered significant: Dawson (2000) reported an average increase in ABI in the cilostazol group of 0.04, while in the placebo group ABI fell by an average of 0.01.
At the same time, there are studies indicating a negative effect of cilostazol: Otsuka Study 21−86−103 showed a decrease in IVD by 6.9 m when taking cilostazol and an increase of 30 m in the placebo group (the statistical deviation of the geometric mean was 0.83 in favor placebo). Otsuka Study 21−87−101 also showed negative results. In contrast, Strandness (2002) et al. compared the intake of cilostazol 50 mg with placebo and showed a pronounced positive effect (increase in DBC in the cilostazol group by an average of 32 m compared with the placebo group) [23]. Taking cilostazol at a dose of 150 mg 2 times a day also has a positive effect (IVD in the cilostazol group increased by 51.8 m compared with the placebo group) [28].
When comparing cilostazol and pentoxifylline, mixed results were obtained: in some, preference was given to cilostazol [29], in others, no difference was found between the effectiveness of the drugs [30].
Among the side effects when taking cilostazol, the most common were headache, diarrhea, bowel movements, dizziness, tachycardia, and pain in the limbs. Convincing data on the effect of cilostazol on mortality have not been obtained.
The use of naftidrofuryl shows promising results. This drug blocks 5-HT2 receptors, thereby improving blood circulation in the ischemic area and increasing ATP production. In addition, its vasodilating effect should be noted. The drug currently holds 52% of the UK market.
Studies [31, 32] provided evidence of a significant positive effect of naftidrofuryl: DBC and MTD compared to their values in the placebo group increased by 49 and 60%, respectively. Naftidrofuryl showed better results compared to cilostazol and pentoxifylline in assessing DBC and IVD [33].
Prostacyclin analogues (in particular, iloprost, prostaglandin I2) are also used to treat CINC. Iloprost has antiplatelet properties; in addition, it activates fibrinolysis, suppresses the adhesion and activation of platelets, as well as the adhesion and migration of leukocytes after endothelial damage. The vasodilating effect of the drug manifests itself at the level of venules and arterioles. Despite the fact that prostaglandins are most often used to treat critical ischemia, there are studies on the effect of the drug on PC: 6 months after the start of the study, an increase in MTD by 7.7, 8.8 and 11.2% was noted when taking 50, 100 and 150 ng 2 times a day compared to the initial values. Interestingly, in the placebo group there was an increase in IVD by 3.3% compared to baseline values. Among the side effects of iloprost, headache was most often noted (44-67% depending on the dosage), and cases of diarrhea, pain in the limbs, and dilatation of subcutaneous vessels were also encountered [16].
In addition to prostaglandins I2, prostaglandins E1 are used to treat CLI. This group of drugs mainly finds its use in the treatment of CLI.
It is believed that the use of dietary supplements (in particular, propionyl-L-carnitine) may have a beneficial effect as a component of the treatment of cardiovascular diseases. The main effect is antioxidant. Propionyl-L-carnitine is responsible for transporting fatty acids across the mitochondrial membrane. In [34], the effect of this dietary supplement on diseases of peripheral arteries is shown. The study assessed the maximum walking time as well as pain-free walking time. There were no data on significant differences in changes in the studied parameters between the treatment and placebo groups, as well as on serious complications associated with taking the drug.
Actovegin is a biological drug used in the treatment of atherosclerosis. The drug is a combination of more than 200 bioactive molecules [35, 36], which was demonstrated using gas and liquid chromography.
One of the most important features of Actovegin is its insulin-like effect, which confirms the significant positive effect of the drug in patients with type 2 diabetes mellitus [37].
Actovegin protects liver cells, myocardium, and neurons from hypoxia, which helps improve metabolism at the cellular level during ischemic tissue damage; in addition, the drug reduces the rate of apoptosis [38]. In case of circulatory disorders in the lower extremities, Actovegin has a stimulating effect on wound healing [39].
Actovegin has a positive effect on the microcirculation of ischemic tissues of the lower extremities and increases their oxygenation, which stimulates reparative processes in the affected extremities [40].
Sulodexide (belongs to the group of heparinoids) reduces platelet aggregation and adhesion, and is also involved in stimulating fibrinolysis by increasing the release of plasminogen activators from the endothelium. Studies confirm the positive effect of sulodexide on the clinical picture of PC: DBC increased by 95%, MDC by 70%, fibrinogen level decreased by 15%. However, no serious complications associated with taking the drug were noted [41].
Genetic therapy as a method of stimulating angiogenesis can be considered a promising direction in the development of therapy for CLI. Currently, several growth factors are used for treatment: endothelium, placenta, fibroblasts, hepatocytes, etc.
There are several ways to administer factors: intramuscular, intraarterial, subcutaneous [42].
Some gene therapy studies have used the likelihood of limb amputation compared with standard treatment to estimate treatment effect. A positive effect of the treatment on this indicator was noted (14% versus 30%) [43]. There were no significant differences in the probability of death between the control and study groups - 12 and 14%, respectively, within 1 year, 9 and 12%, within 2 years. The incidence of serious complications in the groups also turned out to be approximately the same.
In other studies [44–49], the effectiveness of gene therapy was assessed using subjective criteria (DBH, MTD, pain-free walking time, maximum walking time). If Deev (2015) indicates an increase in DBC in the study group compared to the control group (by 151, 231 and 251 m after 6, 12 and 24 months, respectively), then the meta-analysis of the studies did not reveal significant differences between the groups.
Deev (2015) et al. assessed ABI in patients treated with growth factors [46, 50–52]. There was only a slight increase in ABI in the study group compared to the placebo group (+0.04) [53].
The only gene therapy drug approved on the territory of the Russian Federation is Neovasculgen, the active substance is a plasmid with the gene for endothelial growth factor (VEGF165). The mechanism of action is stimulation of the growth of collateral vessels and microvasculature in ischemic tissues. The indication for the use of neovasculgen is grade II-III CINC according to the Fontaine-Pokrovsky classification. It is recommended to administer the drug intramuscularly into the lower or middle third of the gastrocnemius muscle along its posterior surface [46]. There are studies that have shown that the use of neovasculgen has a persistent positive effect in the form of an increase in DBC in most patients [46], in particular, in the long-term period - for at least 5 years [54].
Thus, different drugs affect different stages of the pathogenesis of P.H. However, there is no reason to talk about the exclusive advantage of any of the drugs, since depending on the studies, the results vary significantly and the accumulated information is not yet sufficient [6].
Based on the world literature, there are many drugs whose action is aimed at treating PC, corresponding to degrees IIA-IIB of ischemia according to the Fontaine-Pokrovsky classification. The issue of adjusting risk factors can no longer be considered so pressing: the evidence-based results of the studies made it possible to develop national recommendations and guidelines in which the directions for such adjustment are quite clearly defined. If we talk about the direct treatment of PC, then convincing data on the effectiveness that would meet the criteria of evidence-based medicine have so far been obtained only for drugs of the disaggregant group. But even there, research on the comparative effectiveness of various drugs and treatment regimens is still ongoing, so there is an obvious need for further study, which will optimize the conservative, namely medicinal, treatment of patients with CLI, in particular in the practice of an outpatient surgeon.
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Information about authors
Shabunin Alexey Vasilievich
- Corresponding Member RAS; https://orcid.org/0000-0002-0522-0681
Matveev Dmitry Valentinovich
- Doctor of Medical Sciences; https://orcid.org/0000-0003-2990-2035
Kuznetsov Maxim Robertovich
- Doctor of Medical Sciences; https://orcid.org/0000-0001-6926-6809
Matveev Alexey Dmitrievich
— e-mail; https://orcid.org/0000-0002-0430-2263
How is cerebral ischemia diagnosed in the elderly?
Only a good diagnostician will be able to accurately determine whether a patient has chronic cerebral ischemia. The difficulty is that its symptoms are very similar to those of other pathologies: Parkinson's disease, ataxia, supratentorial brain tumor, multiple system atrophy and others. If an elderly person suffers from angina pectoris, renal ischemia, diabetes, or has suffered a myocardial infarction, then the likelihood of diagnosing chronic ischemia in him increases.
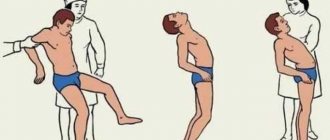
To prescribe the correct treatment, a procedure for recognizing the disease is necessary. It begins with a survey and examination of the patient, and an anamnesis of the disease is collected. The doctor is trying to find the main signs of chronic cerebral ischemia in an elderly patient. To do this, he examines muscle tone, checks clarity of consciousness, facial symmetry, determines the sensitivity of various parts of the body, listens to speech, trying to determine its clarity, examines the reaction of the pupils to bright light, etc.
If the results of a survey and examination of the patient indicate the possible presence of pathology, before starting treatment for an elderly person, the neurologist continues the study, prescribing laboratory, instrumental and physical studies.
The laboratory does blood and urine tests, paying special attention to sugar and cholesterol levels.
Studies of chronic cerebral ischemia on medical equipment are carried out using the following methods:
- Doppler ultrasound ultrasound;
- encephalography;
- ultrasound tomography;
- electroencephalography;
- MR angiography;
- fluorography;
- electrocardiogram.
All necessary treatment procedures are prescribed only by a doctor. After studying the results, the attending physician may refer the patient to other specialists. A physical examination measures the pulsation in the blood vessels of the arms, legs and head.
We recommend
“How to care for a bedridden elderly person” Read more
How to maintain quality of life for people with cerebral ischemia
— Irina Leonidovna, in simple words, what kind of disease is cerebral ischemia? — Cerebral ischemia can be divided into acute and chronic. Acute - cerebral stroke - ranks second in the frequency of deaths from diseases of the circulatory system in Russia. Stroke is an emergency condition, therefore all patients with acute cerebrovascular accident (ACVA), both stroke and transient ischemic attack, should be hospitalized in specialized departments for the treatment of such patients. Assistance before the ambulance arrives or during the patient’s delivery to a medical facility consists of monitoring and maintaining the functioning of the patient’s cardiovascular and respiratory systems.
Chronic cerebral ischemia (CHI) is a slowly progressive brain dysfunction resulting from diffuse and/or small-focal damage to brain tissue in conditions of long-term insufficiency of cerebral blood supply. The concept of “chronic cerebral ischemia” includes “dyscirculatory encephalopathy”, “vascular encephalopathy”, “cerebrovascular insufficiency”, “atherosclerotic encephalopathy”. In the initial stages, chronic ischemia can be manifested by decreased mental performance, mood changes, headache, dizziness and other symptoms.
— What is the diagnosis? — The main diagnostic tests to establish this diagnosis on an outpatient basis include a general blood and urine test, biochemical tests (urea, creatinine, bilirubin, total protein, cholesterol, glucose and other indicators), coagulogram (determination of blood clotting, hematocrit), ultrasound vessels of the head and neck. Based on the results of these examinations, the doctor decides on the patient’s treatment tactics. In addition, it is necessary to clarify the reason that could lead to the onset of the first symptoms. These may be diseases such as myocardial infarction, cardiac ischemia, angina pectoris, arterial hypertension, atherosclerosis of the arteries of the head, neck, extremities, diabetes mellitus and others.
— Who can develop chronic cerebral ischemia and how to avoid it? — Risk factors for development include physical inactivity, obesity, stress, smoking, and alcohol abuse. Moreover, it is necessary to treat diseases such as diabetes, hypertension, atherosclerosis only under the supervision of a doctor. In case of the first signs of the disease, immediately stop smoking, limit the consumption of alcoholic beverages, reduce intense physical activity, and avoid prolonged exposure to the sun. You should be examined by a doctor in a timely manner, since a timely diagnosis and adequate treatment will help stop the progression of the disease.
- But many patients prefer the position “everything will go away on its own”... - If the disease is not controlled, it will lead to acute cerebral ischemia and associated pathologies, which will reduce the quality of life. The main goal of treatment for CICM is to stabilize the destructive process of cerebral ischemia, as well as to take preventive measures against strokes, both primary and recurrent.
— What kind of measures are these and who should especially pay attention to their health? — Primary prevention includes measures to control blood pressure, heart rate, blood sugar levels, blood lipids, the state of the blood coagulation system, body weight regulation, giving up bad habits (alcohol abuse, smoking), and physical activity.
It is especially important to pay attention to your health for women over 50 and men over 45 who have high and, conversely, low blood pressure, suffer from heart failure, arrhythmia, diseases accompanied by the formation of blood clots, patients with diabetes and long-term smokers.
Secondary preventive measures are carried out for patients who have already suffered an acute cerebral circulatory disorder, stroke, heart attack, hemorrhage. They consist of taking measures to prevent the development of a recurrent vascular accident. Chronic cerebral ischemia is very common. And only systemic treatment of the disease can prevent recurrent brain disorders. Proper treatment will help prevent cerebral infarction. The prognosis is good for those patients who are constantly under the supervision of their neurologist. Moreover, preventive measures to prevent the development of this disease should be carried out at any age.
— How to preserve the quality of life for people with cerebral ischemia? — The main goal is to slow down the progression of the disease. The selection of adequate drug therapy (if indicated) and preventive measures aimed at normalizing blood pressure, lipid levels, cholesterol and blood glucose will help improve the quality of life. The use of a number of drugs, including antiplatelet and antioxidant effects, will also help. Antiplatelet agents reduce blood clotting and improve its properties. Antioxidants and antihypoxants bind free radicals, slowing down oxidation processes. They increase the body's resistance to oxygen deficiency, influence intracellular redox processes indirectly, facilitating the transition of oxygen from the blood to tissues, improving blood supply to the brain. Non-drug preventive measures will also help: physiotherapy, occupational therapy, hydrokinesitherapy, regular motor and mental activity.
— Does CIGM affect intelligence and memory? — Chronic cerebral ischemia, occurring against the background of atherosclerosis, hypertension, or a combination of them, causes the development of motor and cognitive disorders. One of its main manifestations is a decrease in memory and speed of thinking, leading to impairments in social adaptation, self-care and communication. These are precursors to the development of vascular dementia. Given the increasing life expectancy, neuropsychological rehabilitation of such patients is becoming an increasingly pressing medical and social problem.
The disease can also manifest itself as disturbances in the emotional sphere: anxiety, depression, apathy, decreased reaction speed, difficulty concentrating, increased fatigue during mental work. Therefore, patients with initial manifestations of decreased memory and thinking deserve close attention; adequate treatment of them before the development of pronounced disorders can be quite effective.
— Older people are more likely to suffer from chronic cerebral ischemia. What should they, their family and friends pay attention to? — It is very important for the timely identification of patients with a high risk of subsequent development of dementia (dementia), so that the elderly patient himself or his relatives pay attention to the first signs of memory loss as early as possible.
In addition, to prevent dementia in the elderly, it is important to provide them with an adequate level of physical activity, quit smoking, and improve their educational level. The first manifestations of memory impairment, gait, falling, loss of balance should alert all elderly people and their relatives.
— What should patients with this diagnosis remember? — About the constant prevention of your illness. That first of all you need to lead a healthy lifestyle. Strictly monitor and treat arterial hypertension, diabetes mellitus, atherosclerosis. Be trained in health schools organized on the basis of health centers of territorial clinics.
Treatment of cerebral ischemia in the elderly
There is no single correct method for treating cerebral ischemia in the elderly. Doctors say it simply doesn't exist.
Therefore, complex therapy is used: many specialists take part in the treatment procedure, but the main role is given to neurologists.
1. Folk remedies.
Traditional medicine over hundreds of years of existence has accumulated many recipes and methods to alleviate chronic cerebral ischemia in older people. However, they can only be used as an additional treatment. The main thing is to take medications and perform procedures prescribed by the attending physician.
Traditional healers offer a number of decoctions and potions that can be taken as an addition to the main treatment:
- decoctions based on oak bark;
- freshly squeezed carrot juice;
- mint infusions;
- recipes with adonis;
- compresses based on herbal ingredients.
2. Medication.
In each specific case, the doctor prescribes individual medication for an elderly patient, based on the basic steps of drug treatment:
- First of all, it is necessary to normalize blood pressure in order to subsequently prevent stroke or ischemic attacks. The doctor prescribes drugs to thin the blood and dilate blood vessels, for example, Pentoxifylline, Warfarin, etc.
- Then you should restore blood circulation in the vessels and improve metabolism. In this regard, the piracetam-based drug Omaron has recently become popular.
- To treat cerebral ischemia in the elderly, it is necessary to restore the patient’s physical and psychological condition. For this, a course of physiotherapy is prescribed, which may include massage, magnetic therapy, electrophoresis and restorative techniques.
- The next step is to restore brain activity. For treatment, the doctor usually prescribes Cerebrolysin, and to support normal blood circulation - Bilobil or Nimodipine.
- If the disease of an elderly person is very advanced, then surgery will be required to remove sclerotic plaques.
We recommend
“How to prevent stroke using folk and medical means” Read more
Consequences of untimely treatment of cerebral ischemia in the elderly
If you do not consult a doctor in time, an elderly person with chronic ischemia will show unpleasant signs of the disease: memory and performance deteriorate, and fatigue quickly appears. Night sleep becomes interrupted, insomnia appears, and during the day, on the contrary, you want to sleep.
Nausea and vomiting may occur, migraines begin to overcome, and you often feel dizzy.
The healing process is influenced by many factors, primarily age. The older the patient, the more disappointing the prognosis may be. Next comes the general physical condition of the patient, the presence of bad habits and other chronic diseases.
Statistics provide information on the survival rate of elderly patients within a year after treatment. The figure is 75%.
The chronic form of cerebral vascular ischemia is not life-threatening. The acute stage of the disease is much more dangerous.
In this case, urgent medical attention is required, otherwise ischemic attacks or acute oxygen starvation may occur.
An exacerbation is manifested by loss of sensitivity in certain parts of the body, even partial paralysis, and deterioration of vision in one eye. Timely medical intervention within 24 hours will relieve all symptoms.