The human brain is the main organ of the central nervous system. Its surface layer consists of many nerve cells that are interconnected by synaptic connections.
Only 7% of the total number of neurons are in working condition; the rest are waiting for their “turn”. Even from a school biology course, it is known that some brain cells replace others in case of damage or complete death.
However, there are also anatomical deviations that negatively affect working and non-working neurons, thereby killing them and destroying the connection between them. This pathology leads to loss of brain mass and its functional abilities.
The death of nerve cells in the brain is a completely normal process that occurs every day. But the catch is that with neurological abnormalities, the atrophy process covers a significantly larger number of neurons than normal. This almost always leads to the emergence and progression of serious diseases that end in death.
General information
Natural aging processes affect the state of the central nervous system. All older people experience memory deterioration and a decreased ability to learn, remember, and process information. In elderly and senile people, brain atrophy occurs (0.1-0.3% of volume is lost per year), associated with age-related physiological processes, but cognitive function does not quickly reach the level of dementia .
Therefore, in patients with a normal level of consciousness, the term “infectious changes” in the brain is often used. Physiological atrophy begins to develop at the age of 40-60 years and reaches severity by 75 years. In psychoneurological diseases ( Alzheimer's disease , Pick's disease , multiple sclerosis , Lewy body disease ), brain atrophy and, accordingly, neurological disorders progress quickly, leading patients to disability. With these diseases, from 0.5 to 1.4% of brain volume is lost per year. Atrophic changes in the brain, what is it? This is a decrease in the volume and density of brain tissue due to the death of neurons, which occurs for various reasons. Typically, atrophy is the outcome of long-term processes in which organic, irreversible changes in the parenchyma occur and nerve connections are destroyed.
In this case, atrophy of the cerebral cortex, subcortical structures (visual thalamus, limbic system, basal ganglia, hypothalamus) and atrophic changes in the cerebellum are observed to varying degrees. Cortical (or external) atrophy is observed in all patients with secondary atrophy. The changes can be generalized (the entire brain is affected) or local (specific areas of the brain are affected).
In some diseases, the white matter of the brain predominantly atrophies, while in others, the gray matter atrophies. Thus, in multiple sclerosis , atrophic changes in the gray matter occur in the early stages; they develop faster than white matter atrophy and are associated with cognitive impairment. As the volume of the cortex decreases, neurological changes progress. Women get sick more often than men and the first signs of pathology appear at 55 years of age. In this regard, it is important to carry out effective treatment that would reduce the rate of atrophic changes. This pathology cannot be cured and sooner or later ends in dementia . The rate of atrophy determines the speed of onset and severity of disability.
Clinical symptoms of brain atrophy
The manifestations of pathology are largely determined by the causes and provoking factors. Most older people have dementia, frontal lobe syndrome, and internal multiple organ pathology.
How does frontal lobe syndrome manifest?
- Lack of appetite;
- Loss of memory, intellectual activity;
- Frequent emotional breakdowns;
- Lack of communication with surrounding people;
- Irritability;
- Lack of self-criticism.
Psychoorganic syndrome is accompanied by cerebroasthenic disorders, affective disorders, and amnesia.
The patient lacks an adequate assessment of surrounding events and self-criticism. Primitive thinking appears, a one-sided representation of the essence of the detail. Speech reserve decreases, paramnesia appears.
Concomitant affective disorders lead to depressive syndrome and inadequate mental state. Tearfulness, touchiness, irritability, unreasonable aggression are typical manifestations of pathology.
Pathogenesis
The development of atrophic processes in most cases is based on deterioration of blood supply. The cerebral cortex is gray matter. The white matter is located under the gray matter. The subcortical substance is formed by the thalamus, caudate and lenticular nuclei, and basal ganglia. It was found that the subcortical substance and the white matter of the hemispheres, located around the ventricles of the brain, are more affected by chronic cerebral ischemia than the gray matter. When cerebral vessels are damaged, the supply to the frontal subcortical areas is disrupted. Large areas of infarction develop in the white matter, in which axons and oligodendrocytes .
Damages to the cerebellum cause a decrease in its function: muscle contractions are discoordinated and it becomes impossible to perform normal movements in the limbs. The coordinated function of the muscles of the speech apparatus is disrupted, resulting in speech becoming slow and intermittent. Ataxia of the respiratory muscles is manifested by jerky breathing. Hypotonia of the tongue muscles causes soft consonants to be pronounced firmly.
Degrees of atrophy
The development of deviation occurs according to the following scheme:
- Initial stage or 1st degree brain atrophy - there are no clinical signs, but the disorder rapidly develops and passes into the next stage of the disease.
- The second stage is a rapid deterioration in the patient’s communication with others. At the same time, the person becomes conflicted, cannot normally perceive criticism, or catch the thread of the conversation.
- The third stage - the patient gradually loses control over behavior. Unreasonable outbursts of anger or despondency may appear, and behavior becomes outrageous.
- The fourth stage is a loss of awareness of the essence of events and the demands of others.
- Final stage - The patient does not understand the events that are taking place, and they do not evoke any emotions in him.
Depending on the affected areas of the frontal lobe, speech disturbances, lethargy, indifference or euphoria, sexual hyperactivity, and certain types of mania may appear at first.
The latter point often makes the patient dangerous to society, which is an indication for his placement in a psychiatric hospital.
If the blood supply to the brain is impaired, one of the diagnostic signs may be the death of the temporal muscle, which is observed in some patients.
Classification
Cerebral atrophy occurs:
- Primary. It is rare and is caused by genetic disorders and congenital brain abnormalities. It appears at any age, progresses quickly and cannot be corrected.
- Secondary. It is associated with the impact of adverse factors on the brain, among which are vascular pathology, traumatic brain injury, exposure to radiation, toxic effects, metabolic disorders, and bad habits. With secondary atrophy, eliminating the cause to some extent slows down the development of the disease, and adequate treatment ensures a stable condition for many years and a relatively good quality of life.
- General (the entire volume of the brain parenchyma decreases and the volume of the ventricles and subarachnoid spaces increases).
- Local (the volume of some brain structures decreases).
Depending on the location, there are:
- Cortical atrophy (the main symptom is the involution of the cortex in the temporal and frontal lobes).
- Generalized (changes in all parts of the brain).
- Multisystem (foci develop in several areas).
Depending on the stage:
- Stage I. Organic changes are minimal, but mild neurological disorders are noted. Emotional lability, memory impairment, and decreased concentration are noted.
- Stage II. Severe atrophic manifestations, which are manifested by hearing, speech and vision impairments. Behavior changes, a person commits illogical actions that he cannot explain and quickly forgets about them.
- Stage III. Cortical atrophy is sharply expressed and multiple foci are noted in the hemispheres. The patient cannot care for himself and needs outside help. Personal degradation is expressed to the maximum. This is how a person lives for many years until the destruction of important centers occurs and death occurs.
Cortical cerebral atrophy
This form is manifested by loss of intelligence and behavioral disturbances. The cerebral cortex (gray matter layer) is associated with higher cortical functions: perception, memory, imagination, thinking and speech. It has a complex six-layer structure and the neurons of each layer differ in function. Cortical areas, and accordingly, functions are divided into sensory, associative and motor.
Cortical atrophy occurs with the death of neurons in the frontal lobe cortex. The frontal association area is involved in higher mental functions. It controls behavior, logical thinking, object recognition and speech understanding. After damage to the frontal cortex apathy , there is no critical attitude towards oneself and one’s actions, the patient cannot use past experience, and his behavior becomes inadequate and unpredictable, he commits unmotivated actions. Cognitive (cognitive) abilities are gradually lost: the patient loses the ability to perceive, perceive information, analyze and remember it, and think. In general, cortical atrophy of the brain is characterized by progressive personality degradation, which occurs in stages.
Grade 1 cortical cerebral atrophy is the initial stage of the disease, in which there are no symptoms, but this conclusion can be given with MRI even in young people. At the same time, a person lives a full life and is active in his professional activities, but may periodically experience headaches , irritability and be emotionally unstable. Factors causing cerebral atrophy of the 1st degree may be various intoxications, previous traumatic brain injuries and deterioration of blood supply to the brain with osteochondrosis of the cervical spine .
Generalized atrophy
This is a common atrophy characterized by uniform death of areas of the entire brain. This form is characteristic of extensive ischemic and post-traumatic conditions, as well as neurodegenerative diseases - Alzheimer's disease , Parkinson's disease , Pick's disease and frontotemporal dementia. The progression of neurological symptoms depends on the degree of atrophy of the cortex and subcortical gray matter. Decreased cognitive function is associated with damage to the white matter and parietal cortex.
In this regard, generalized cerebral atrophy of the 2nd degree is characterized by a noticeable decrease in the patient’s ability to think and analyze. The level of critical thinking and evaluation of one's actions is reduced. The patient's habits, speech and handwriting also change. The person loses emotional connection and communication abilities. Neurological disorders - movements and coordination of movements - are more pronounced.
The third degree is characterized by degeneration of gray and white matter. The patient cannot control his behavior, and also needs care and observation, since there is a deterioration in hand motor skills and coordination of movements. The patient cannot use basic household items and is unable to make decisions independently.
Local degeneration is associated with:
- vascular diseases;
- alcohol abuse (atrophy of the cerebellar vermis is noted);
- multiple sclerosis;
- drug use;
- brain injury;
- infection of the central nervous system.
In the early stages of multiple sclerosis, the disease is characterized by degeneration of subcortical gray matter, most pronounced in the thalamus. After this, damage to the cortex develops (the central gyri are more affected), over time, destruction of the white matter is noted, and only then the spinal cord. In multiple sclerosis, not only general atrophy is observed, but also local atrophy - structures that have gray matter are affected: the cerebellum , basal ganglia and thalamus . In multiple sclerosis, gray matter atrophy predominates over changes in white matter, and it determines the degree of disability of patients.
Cerebellar atrophy
The cerebellum is located below the hemispheres and above the brain stem. This formation coordinates movements and their precision, receiving information from the cortex and basal ganglia about the position of the legs. Cerebellar lesions are characteristic of multiple sclerosis , Friedreich's ataxia , olivopontocerebellar degeneration , Pierre-Marie's ataxia . Ataxia (meaning disorder) is a characteristic feature of lesions of this brain formation.
Friedreich's ataxia appears at 10-20 years of age. Patients develop weakness in the legs, falls, staggering and uncertainty when walking, handwriting, speech and hearing are impaired. Muscle atrophy gradually increases (at first it is expressed in the legs, and over time it also covers the arms), deep sensitivity is impaired, cataracts develop, the optic nerve atrophies, and dementia develops. Computed tomography for this disease is ineffective, since a weak degree of atrophy of the hemispheres and cerebellum, expansion of the cisterns, and ventricles is detected in the later stages. Olivopontocerebellar atrophy is considered a form of multiple system atrophy.
Multiple system brain atrophy
This is a variant of a degenerative progressive pathology of the brain, which affects the basal ganglia, cerebellum and centers that are responsible for autonomic reactions. Clinically, multiple system atrophy is manifested by parkinsonism , cerebellar ataxia and autonomic disorders . The disease appears at the age of 50-60, progresses rapidly and leads to death. The muscles become stiff, the patient has difficulty moving, coordination and function of internal organs are impaired.
Depending on the predominant syndrome, the following forms of the disease are distinguished:
- Striatonigral degeneration or parkinsonian form . With it, degenerative changes are most pronounced in the striatum (belongs to the basal ganglia) and the substantia nigra (part of the extrapyramidal system, which plays a role in motor function). The leading symptom is parkinsonism .
- Olivocerebellar atrophy or cerebellar form . The cerebellum, olives and pons are affected. In the clinic, cerebellar syndrome predominates, manifested by impaired coordination and inability to maintain balance.
- Shy-Drage syndrome . In this form, the leading ones are autonomic failure and orthostatic hypotension - in patients, the pressure sharply decreases and a pre-fainting state appears when moving to a vertical position. Patients are also concerned about decreased sweating, darkening of the eyes, urinary disorders, impotence and unsteady gait.
Alzheimer's disease
This is a progressive disease with increasing impairment of memory, thinking, intelligence, speech, praxis and recognition, ultimately leading to dementia.
Data on the prevalence of the disease are conflicting. According to some reports, it is 4–5% among people over 60 years of age. The main clinical forms of the disease are Alzheimer's disease itself (with onset mainly in presenile age) and senile dementia of the Alzheimer's type (with onset mainly in old age). An atypical form of the disease with a predominance of frontal lobe atrophy and Alzheimer's type dementia within Down syndrome are also distinguished. Here is a description of the main forms of the disease. 1. Alzheimer's disease . In approximately 80% of cases, it begins at the age of 45–65 years, less often - at the age of about 40 or after 65 years. The duration of the disease is on average 8–10 years, possibly protracted (more than 20 years) and catastrophic (from 2 to 4 years). There are three stages of the disease.
| | Read about diagnosing and treating Alzheimer's disease |
The initial stage includes the stage of “doubtful” dementia and the stage of “mild” dementia. The first stage is manifested by mild disturbances in memory, thinking, speech, praxis, and personality, which are noticeable mainly to the patients themselves and which they manage to hide or compensate for for some time. At the stage of mild dementia, impairments become more serious. Memory for current events decreases, chronological and spatial types of memory suffer.
Violations of various thinking operations are revealed. Disorders of speech, praxis, recognition, and psychopathic personality changes are detected. The severity of the disorders is such that patients can no longer cope independently with professional responsibilities and other types of social activities, such as shopping, paying bills, receiving guests, writing texts, etc.
Patients cope with self-care, although they need outside control and encouragement. Affective and delusional disorders are often observed at this stage. These are subdepressions, sometimes chronic and combined with anxiety, hysteriform and hypochondriacal manifestations; episodic or protracted delusional ideas of damage, theft, less often - ideas of relationship, persecution or jealousy. Some patients show increased exhaustion and headaches; the duration of the initial stage ranges from 4–8 to 15–20 years. At the same time, in some patients, memory impairments predominate, while in another, larger group, focal impairments (aphasia, etc.) prevail.
At the stage of moderate dementia, impairments in the cognitive sphere and higher cortical functions reach a degree where patients can no longer cope with professional and social responsibilities. They need help even with everyday life and self-care. Neurological disorders appear, such as muscle stiffness, akinesia, hyperkinesis, and seizures. A critical attitude towards the disease nevertheless remains. Along with deficient ones, productive disorders are sometimes observed: episodes of hallucinatory confusion, a state of psychomotor agitation, often not associated with a deterioration in the somatic condition. The aphato-apracto-agnostic syndrome (three A syndrome) characteristic of this stage is finally formed, the weakening of memory takes on the character of progressive amnesia. Confabulation and ecmnesia often do not occur.
The stage of severe dementia is characterized by the breakdown of memory, thinking and intelligence, as well as higher cortical functions. Patients need help even with basic self-care. Basically, only in Alzheimer's disease are such profound disturbances, to the point of insanity, observed, as well as fetal position, contractures, multiple violent motor phenomena, violent laughter and crying, and epileptic seizures. At the same time, there are pronounced somatic changes: weight loss, extreme decrepitness, bulimia, endocrine disorders.
2. Senile dementia of the Alzheimer's type. In approximately 80% of cases, it begins between the ages of 65 and 85 years. The duration of the disease ranges from 4 to 15 years or more. In the initial stage of the disease, significant memory impairment for current events develops, often with a revival of memories of the distant past. Thinking operations suffer, as well as intelligence (creativity, planning, forecasting, etc.). Personality changes are characteristic: egocentrism, narrowing of interests, emotional impoverishment, conflict, opposition and suggestibility. Moral decline and disinhibition of drives are also observed.
The suspicion inherent in patients later develops into a tendency to develop delusions. However, half of the patients experience psychotic episodes with low-level delusions. Subdepressive states are also observed, especially gloomy depression. In the second stage of the disease, memory impairment takes on the character of progressive amnesia. There may be scanty confabulations, as well as states of amnestic disorientation with a “shift of the situation into the past.” At the stage of moderate dementia, disorders of higher cortical functions also become clear. At the stage of severe dementia, a complete breakdown of mnestic-intellectual functions is observed, and serious neurological disorders are also detected.
The etiology of Alzheimer's disease has not been established. The role of genetic factors in the development of familial forms of the disease can apparently be considered proven. However, this role remains unclear in sporadic forms, which account for about 90% of all cases of the disease. Aging is essential.
The leading place in the treatment of patients is occupied by replacement therapy aimed at overcoming neurotransmitter deficiency. To compensate for cholinergic deficiency, tacrine, amiridine, exelon, memantine, Aricept, and reminyl may be recommended. To eliminate the deficiency of other neurotransmitter systems, other drugs are recommended, in particular Yumex and Citalopram. To increase the survival of neurons, nootropics are prescribed, especially Cerebrolysin, as well as vasoactive drugs, in particular sermion or nicergoline. Anti-inflammatory treatment such as indomethacin may be helpful. Therapy for psychotic disorders is carried out with the help of antidepressants, antipsychotics, and tranquilizers. The prognosis of the disease is unfavorable.
Causes
Cerebral atrophy in most cases is secondary in nature and it is worth noting the reasons that lead to this condition:
- Genetic predisposition.
- Chronic cerebral ischemia , causing diffuse damage to the white matter (cerebral atrophy), against which vascular dementia develops. It should be noted that cerebral atrophy in vascular dementia is not very pronounced when compared with Alzheimer's disease , and hippocampal atrophy in chronic cerebral ischemia is the same as in Alzheimer's disease.
- Arterial hypertension hypertensive encephalopathy develops . With this disease, MRI reveals multiple changes in the subcortical zones around the ventricles (leukoaraiosis), cortical atrophy and dilatation of the ventricles. The same changes are observed during physiological aging.
- Antiphospholipid syndrome.
- Central nervous system infections ( meningitis , polio , leptospirosis ).
- State of decortication in coma .
- Atherosclerosis general and cerebral. The condition worsens when atherosclerosis is combined with arterial hypertension.
- Brain tumors.
- Embolism of the cerebral arteries. The source of embolism is fragments of atherosclerotic plaques and blood clots from the heart.
- Atrial fibrillation . In patients with fibrillation, the brain matter as a whole, as well as individual parts, decreases. The frontal regions of the brain and hippocampus are primarily affected.
- Congenital anomalies of cerebral vessels, causing cerebrovascular disorders.
- Blood rheology disorders (increased viscosity, platelet aggregation, etc.).
- Elevated homocysteine . Homocysteine is a sulfur-containing amino acid, an increase in the level of which is associated with the development of vascular disorders of the brain and heart and neurodegenerative processes in the brain. Hyperhomocysteinemia is a risk factor for recurrent strokes and white matter changes. Patients with elevated homocysteine levels have greater hippocampal atrophy.
- Diabetes . Patients with diabetes mellitus are characterized by mild cerebral atrophy of the cortex, subcortical structures and leukoaraiosis . Even an increase in glucose to the upper limit is associated with atrophic changes in the hippocampus and amygdala complex.
- Multiple sclerosis . Already in the early stages, patients experience degenerative changes - neurons and axons die. Axonal damage is observed in active and chronic lesions of sclerosis. In the latter, axon density decreases to 80%. These processes, plus gliosis and demyelination, lead to a decrease in brain volume. Patients with relapsing-remitting sclerosis (it occurs with exacerbations and remissions) lose 0.5-1.3% of brain volume per year.
- Alzheimer's disease . MRI reveals atrophy of the temporal lobe (reduction in the volume of the gyri and widening of the sulci) and hippocampus, which are markers of this disease. The hippocampus plays an important role in memory formation (categorization of information and long-term memory). Any traumatic brain injury accelerates the development of Alzheimer's disease.
- Any intoxication of the body (drug, alcohol, drugs). With alcoholism, diffuse brain atrophy develops.
- Age-related changes.
- Hydrocephalus in children. This pathology is accompanied by structural changes in the brain: thinning of the cortex, reduction of white matter, vascular atrophy and atrophy of the basal ganglia and cerebellum.
- Traumatic brain injury . 3-4 weeks after the injury, minor hemorrhages resolve, the ventricles and subarachnoid space expand, and generalized brain atrophy develops, which is caused by prolonged intracranial hypertension.
- Long-term corticosteroid therapy can cause cerebral atrophy.
- Acute pain. Acute pain that persists for 3 months causes atrophic changes in the cerebral cortex.
- Physical inactivity . A risk factor for the appearance of atrophic processes and a decrease in cognitive cognitive functions is the limitation of physical activity.
Diagnostics and differential diagnostics
Cerebral arthrosis is a disease for which diagnosis may require a detailed history of the patient.
The medical history is studied and the patient is interviewed about his living conditions and well-being.
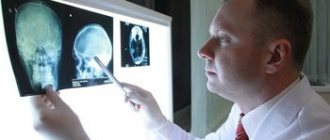
But to make an accurate diagnosis, professionals send the patient to undergo the following diagnostic tests:
- CT head;
- diffuse optical tomography;
- MEG (measurement and visualization of magnetic fields);
- two-photon or single-photon emission tomography;
- MRI of the head.
And also in rare cases, differential diagnosis is possible. Having a patient's medical history, using a specially created computer program, a diagnosis can be made by exclusion. Based on the facts and symptoms that appear in the patient, the computer reduces the range of all possible diseases to one.
If it is impossible to carry out a complete diagnosis, a partial differential diagnosis can be made.
Symptoms of brain atrophy
The initial symptoms of the disease reflect changes in the mental state of patients. Early symptoms are anxiety and depression . Patients become apathetic, lethargic, they are not interested or attracted to anything, they prefer to retire and constantly stay at home, their night sleep is disturbed. The mask of depression is irritability, dissatisfaction with everything and grumpiness, which are regarded as characteristics of older people.
If depression is a marker of internal atrophy, then anxiety disorders are characteristic of focal and external cerebral atrophy.
Cognitive disorders (memory, attention, concentration, ability to recognize objects and perform actions purposefully) are detected in all patients in the early stages of brain degeneration. Cognitive symptoms and depression are often regarded as senile forgetfulness and low mood. Impaired memory and attention first occur against the background of maintaining professional and everyday skills. As it progresses, social skills are gradually lost (the patient cannot independently go to the store, pharmacy, or visit the clinic, since he lacks purposefulness of actions) and household skills (he cannot simply take care of himself, eat and take a shower). Over time, sloppiness appears, the vocabulary becomes poor, the patient does not comprehend the speech and requests addressed to him. His movements are sweeping, his handwriting changes and his fine motor skills deteriorate.
In severe cases, the patient does not recognize his relatives and friends, cannot navigate the place and cannot answer questions. The specific behavior is that patients constantly repeat actions and words after others. The final stage of brain degeneration is marasmus - complete regression of mental abilities and destruction of personality. At the same time, infant reflexes are activated: a sucking reflex appears, the patient lies in the fetal position, recovers and urinates under himself. He responds to calls with inarticulate sounds.
Symptoms of cerebellar atrophy
Since the cerebellum regulates movements, if it is damaged, the following will be observed:
- Balance and muscle tone problems.
- Gait disturbances (wide-spaced legs, unsteadiness, difficulty turning).
- Fine motor disorders.
- Uncoordinated movements of arms and legs.
- Unsteadiness and frequent falls.
Patients are also worried about headaches , dizziness , attacks of nausea and vomiting, visual disturbances, pronunciation problems, scanned and slow speech, uncoordinated eye movements, and decreased hearing acuity. As it progresses, urinary incontinence , paresis and paralysis .
Clinical symptoms of multiple system atrophy
Diffuse neurodegeneration is accompanied by problems in the reproductive and urinary areas. Necrosis of many parts of the brain is simultaneously accompanied by a variety of clinical symptoms:
- Muscle tremors in Parkinsonism;
- Impaired gait and mobility coordination;
- Loss of erection;
- Vegetative-vascular disorders.
Before the advent of magnetic resonance imaging, early diagnosis of the disease was problematic. Only nuclear magnetic resonance verifies a decrease in the thickness of the brain parenchyma.
Tests and diagnostics
When examining a patient, psychodiagnostic examinations are used - tests, Schulte tables, MMSE mental status assessment scale, memorizing 10 words, etc.
- An MRI scan of the brain is also used. MRI is more effective at detecting local changes. Characteristic signs of atrophy are widening of the grooves (cortical atrophy) and enlargement of the ventricles. Based on this, the cerebroventricular index (the ratio of the size of the ventricles to the transverse diameter of the brain) is calculated. With this pathology, MRI reveals: an increase in CVI; expansion of subarachnoid spaces; white matter degeneration; decreased tissue density; reduction in shares in size. Based on the study, a quantitative assessment of atrophy is made. In generalized cortical atrophy, sulcal and ventricular widening is assessed in 13 different areas. Certain diseases are characterized by certain changes: with Pick's disease, atrophy is expressed in the frontal and temporal regions. In Huttington's disease , changes in the heads of the caudate nuclei. Parkinson's disease is accompanied by generalized atrophy and atrophy of the substantia nigra, and in Alzheimer's disease - atrophy of the hippocampus.
- The Fazekas scale evaluates quantitative white matter damage. The score on this scale has prognostic value. If the total score is 3, then the patient loses the ability to care for himself and live independently within a year: 0 - no leukoaraiosis; 1— multiple point lesions; 2 - moderate leukoaraiosis, with a tendency to merge; 3 - severe leukoaraiosis (“confluent”).
- Doppler ultrasound. Detects vascular patency.
- Electroencephalography (studies the degree of brain activity).
- Rheoencephalography (studies the state of blood circulation in the brain).
- Angiography (radiography of blood vessels with a contrast agent).
- Blood pressure monitoring and ECG monitoring if indicated.
- Ophthalmoscopy.
- Biochemical blood test.
Principles of diagnosing atrophy
The initial stage involves taking an anamnesis, examination, and physical examination. The second stage is clinical and instrumental methods (ultrasound, CT, MRI of the brain, scintigraphy, PET/CT). Damage to the optic nerve is confirmed by ophthalmoscopy, tonometry, contrast CT or MRI angiography.
The best way to detect pathology of the soft tissues of the brain is MRI. The procedure must be performed several times (a month apart) to identify atrophy of varying depth and extent.
Magnetic resonance examination reveals the smallest local lesions and helps to correctly determine the degree of disease progression.
Diet
Mediterranean diet
- Efficiency: from 2 kg in 7 days
- Terms: from 7 days
- Cost of products: 4000-6000 rubles for 7 days
Diet for Parkinson's disease
- Efficacy: therapeutic effect after a month
- Timing: constantly
- Cost of food: 1600-1700 rubles per week
In addition to drug maintenance treatment, it is important for patients with beginning signs of degenerative age-related processes to follow a diet. The Mediterranean diet has been proven to have a neuroprotective effect and prevent the development of cognitive impairment. Its features are a large amount of vegetables, fruits, fish (at least 3 times a week), which should replace meat, whole grain products and vegetable oils rich in ω-3 PUFAs (flaxseed, rapeseed) and ω-9 PUFAs (olive).
For problems with the cardiovascular system, the patient should receive 1 g of ω-3 PUFAs daily from fatty fish (salmon, herring, mackerel), nuts and flax oil. Mackerel has the highest omega-3 content (2299 mg per 100 g), followed by salmon (1966 mg) and herring (1571 mg). Depending on the type of fish, 50-80 g of it contain the daily requirement of 1 g of ω-3 PUFAs, and a handful of walnuts - 2.5 g of omega-3.
Flaxseed oil is a source of alpha-linolenic acid , from which eicosapentaenoic and decosahexaenoic acids are formed in the body. It is useful to consume not only flax oil, but also whole flax seeds, which contain fiber and phytoestrogens . Other sources of omega-3 include broccoli, melon, cauliflower, canola oil, beans, spinach, and Chinese cabbage.
In addition, it is better to replace omega-6 fatty acids (sunflower oil and soybean oil) with omega-9 - oleic acid found in olive oil. High doses of antioxidant vitamins (vitamins C and E) have been proven to be beneficial for the restoration of vascular endothelium. Flavonoids in red wine, red grapes and chocolate improve endothelial function in large arteries.
Preventive measures
Today there are no effective ways to prevent this disease. We can only advise you to treat all existing disorders in a timely manner, lead an active life and have a positive attitude.
Life-loving people often live to a ripe old age, and they do not show any signs of atrophy.
It should be understood that over the years, not only brain disorders can occur - other organs are subject to changes. These conditions of the body are related to the development of vascular atherosclerosis, because as a result of this disease their narrowing occurs.
There are people in whom the development of atherosclerosis occurs much faster, which is the cause of early wear and tear of the body. They are the ones who experience clear processes of atrophy.
Ways to prevent atherosclerosis:
- healthy lifestyle;
- proper nutrition;
- high physical activity;
- to give up smoking;
- refusal of alcohol;
- blood pressure control;
- eating fresh fruits and vegetables;
- replacing animal fats with vegetable ones;
- fasting days;
- daily memory training.
Brain atrophy is a disease that cannot be treated with modern medications. This disorder does not develop immediately, but eventually ends in dementia.
To prevent negative consequences, it is necessary to adhere to preventive measures . Among other things, if you have any problems, it is very important to consult a doctor on time - this will help preserve good health for many years.
Prevention
There is no specific prevention, but following generally accepted recommendations for a healthy lifestyle can to some extent prevent or reduce the severity of degenerative changes in old age.
- Full sleep.
- Physical activity. Sufficient activity in old age has a positive effect on brain function and slows down age-related changes. Individuals with high activity exhibit less atrophy—less damage to white matter and greater volume of gray matter.
- Sufficient intellectual activity.
- Maintain a diet rich in antioxidants, vitamins and omega PUFAs. The results support the possibility of effective use of fish oil in reducing cognitive ability in the elderly and in Alzheimer's disease. Often cognitive impairment is associated with a deficiency of folic acid and vitamin B12 .
- Quitting the use of alcohol and drugs.
- Elimination of risk factors (high blood pressure and blood sugar levels, lipid metabolism disorders, anxiety, depression, sleep disturbances).
- Timely treatment of initial cerebrovascular disorders.
- Prevention of head injuries and infections of the nervous system.
- Genetic counseling for people with a family history of Alzheimer's disease .
- To prevent hydrocephalus in children, which causes brain atrophy, it is important to promptly identify and treat infections in pregnant women.
Causes of the disease
According to statistics, symptoms of Alzheimer's disease develop in 5-8 people per 1000 population. Every second case of dementia is caused by this particular pathology. In the last decade, there has been an increase in incidence, but doctors still find it difficult to name the exact causes of neurodegenerative processes. Increased risks have been proven in the age group over 65 years of age. After 95 years, almost 70% of older people develop characteristic symptoms. Women are affected more often than men, but this may be due to their longer life expectancy, especially in European countries.
Most experts agree that the main factor that triggers neurodegenerative processes is the natural aging of the body. Slowing metabolic processes contributes to the accumulation of amyloids.
Genetic studies have proven a hereditary predisposition to Alzheimer's disease. Mutations in several chromosomes lead to disruption of protein metabolism in cerebral tissues. Genetics most often causes the early onset of the disease, when the first signs of dementia appear at the age of 30-40 years.
The following factors can accelerate the development of pathology:
- Poor nutrition.
- Living in areas with poor ecology.
- Bad habits.
- Poisoning with chemicals, heavy metals.
- Chronic stress.
- Past neuroinfections: meningitis, encephalitis.
- Brain tumors.
Forecast
The prognosis for cerebral atrophy is unfavorable, since this pathology is not treated, progresses and is associated at first with a decrease in the quality of life, and then with disability. Irreversible changes in the brain lead to a decrease in intelligence to the point of mental retardation. Cerebral atrophy does not always reduce life expectancy, but significantly worsens its quality. Life expectancy with cerebral atrophy depends on the degree of damage and the rate of progression. With rapid progression and involvement of vital centers, life processes may stop.
Life expectancy with multiple system atrophy is significantly reduced as bulbar palsy , a swallowing disorder, progresses rapidly. Dysphagia is complicated by aspiration of food and pneumonia , often leading to death. asphyxia occur .
Causes and essence of the disease
Vascular dementia develops due to disruption or cessation of blood circulation in one of the brain areas, as a result of which some brain cells die. The rate of progression of the process and the severity of symptoms will depend on how quickly the provoking factor acts.
Acute development of pathology is observed with stroke, ischemic or hemorrhagic. In the case of an ischemic stroke, a blood line is blocked by a thrombus. Its hemorrhagic form is characterized by rupture of the vessel. Both phenomena interfere with blood supply, which leads to irreversible death of cells in the brain area.
Typically, vascular dementia occurs in 25% of stroke patients. This happens if 50 ml of brain tissue is affected. The area and affected area play a big role. However, there are particularly sensitive areas of the brain, where even the slightest destruction entails disastrous consequences. These are, for example, the frontal lobes, visual hillocks.
For patients with vascular dementia, there is such a pattern: the first symptoms can appear either immediately after a stroke, or delayed, within six months. A period of 6 months is an indicative sign of vascular dementia. Typically, a stroke, especially a hemorrhagic one, leads to a rapid development of events, the appearance and increase of symptoms.
In a chronic destructive process, when small vessels are damaged, brain cell atrophy occurs gradually. Its compensatory mechanisms are activated, and symptoms increase gradually. The first signs are difficult to identify. Sometimes they hide not only from others, but also from the patient himself.
The main provoking factor that causes disruption of the patency and integrity of the blood network in the brain is atherosclerosis, that is, the deposition of sclerotic plaques on the vascular walls. Other reasons include:
- heart disease, cardiovascular failure;
- arterial hypertension;
- arterial hypotension;
- vasculitis – inflammation of the vessel wall;
- diabetes;
- hyperlipidemia;
- lack of estrogen;
- bad habits;
- excess body weight.
List of sources
- Lokshina A. B., Zakharov V. V. Mild and moderate cognitive impairment in dyscirculatory encephalopathy. //Neurologist. magazine – 2006. – T.11, appendix.1. – P.57 – 64.
- Vorobyova O. V. Chronic cerebral ischemia: from pathogenesis to therapy (recommendations for an outpatient neurologist) // RMJ “Medical Review” No. 5, 2021. - P. 26-31.
- Golubev V.L., Vein A.M. Neurological syndromes: a guide for doctors. 6th ed. – M.: MEDpress-inform, 2021. – 736 p.
- Ekusheva E.V. Clinical portraits of “typical” patients in neurologist practice. Consilium Medicum. 2019; 21(9): 131-135.
- Odinak M.M., Voznyuk I.A. Neurometabolic therapy for pathologies of the nervous system. Emergency medicine. 2013; 3(50): 72-77.
Symptoms
Atrophic manifestations will be of a different nature depending on what form of the disease affected the patient, where the focus is localized and how widespread it is. Common clinical signs are:
- Reduced ability to think and analyze;
- Violation in the pace and tone of speech;
- Memory disorder;
- Changes in finger motor skills;
- The appearance of pathological reflexes with convulsions;
- Difficulty in learning new information;
- Reduced vocabulary;
- Emotional imbalance in the form of depression, aggressiveness, resentment, euphoria for no reason;
- Headache with increased fatigue.
All these symptoms eventually lead to the patient’s loss of ability to work.
Methods for treating atrophic brain pathology
Cortical atrophy of the brain cannot be completely cured. The most important thing is to stop the progression of the pathology, which can be done with greater success at a young age than in older people. Therapy for atrophy, depending on the situation, can be carried out using the following medications:
- nootropics are used to improve nutrition of brain cells. In addition, these drugs help normalize the thinking process;
- the action of antioxidants is aimed at improving metabolism, slowing down the atrophy process, and counteracting oxygen free radicals;
- drugs to improve blood microcirculation.
In addition, if a person suffers from headaches, he is prescribed to take analgesics or anti-inflammatory non-steroidal drugs. For increased excitability, irritation, and insomnia, sedative medications are indicated. The support of the patient’s relatives, their help and understanding is very important. It is undesirable for the patient to change the usual way of life; it is necessary to create the most calm and familiar environment for the person. Walking in the fresh air and feasible physical activity are very important. Daytime sleep is undesirable for a person with atrophic pathology of the brain. If the doctor allows, the patient may be prescribed a course of therapeutic massage to improve the patient's blood flow. If necessary, the treating specialist can prescribe sedatives, antidepressants, and tranquilizers. In cases where relatives are not able to cope with the patient on their own, due to his aggressive behavior, specialized nursing homes and boarding schools are provided for patients with impaired brain function.
The prognosis of people with cortical atrophy of the brain is far from rosy. The disease, one way or another, progresses at a slow or rapid pace, leading to irreversible changes in the cerebral cortex, personality degradation, which ultimately leads to death. The main factors that can stop the development of pathology in a patient are:
- positive psycho-emotional mood, complete absence of stressful situations;
- daily mental stress, working on your memory;
- eating healthy foods;
- complete cessation of habits harmful to the body, such as smoking, alcohol, and taking drugs;
- blood pressure control;
- daily walks, moderate physical activity.