Hospitalization and treatment under the compulsory medical insurance quota. More details after viewing the pictures.
- Aneurysm clipping
A cerebral aneurysm is a local protrusion of the arterial walls. The disease often occurs without symptoms. As the brain aneurysm grows, a significant thinning of the walls of the formation occurs, which can lead to its rupture and the development of hemorrhagic stroke.
Depending on the shape, a cerebral aneurysm can be spindle-shaped or saccular. The exact type of disease can only be determined during a comprehensive diagnosis. Saccular aneurysm is much more common.
Causes of the disease
An aneurysm is a dangerous condition that primarily requires surgical treatment. Otherwise, complications will not be avoided. Experts believe that the disease is a consequence of developmental abnormalities that disrupt the structure of the vascular wall. Often, a cerebral aneurysm is combined with connective tissue dysplasia, polycystic kidney disease, and vascular disorders. The acquired form of the disease can be a consequence of traumatic brain injury. Also, a cerebral aneurysm occurs against the background of atherosclerosis and hypertension.
The vascular wall defect itself occurs gradually. Against the background of degenerative processes, tissue damage or underdevelopment, the area loses its former elasticity. Under the pressure of blood flow, the vascular wall begins to bulge. This is how a brain aneurysm forms. Most often, the formation occurs in the place where the arteries branch and there is the strongest pressure on the vessel wall.
An unruptured cerebral aneurysm may present with the following symptoms:
- Visual impairment of various types and degrees.
- Convulsions are not of an epileptic nature.
- The headache is unilateral, subacute in nature, with a predominant localization in the fundus of the eye, quite often the pain is throbbing.
- Transient ischemic attack. The most typical symptoms are dizziness, loss of consciousness, nausea, vomiting, temporary loss of orientation in time and space, memory loss, sensory disturbances with complete or partial loss of certain sensations, various paralysis, and speech impairment.
- Dysfunction of cranial nerves. When they are compressed, various neurological disorders can occur, such as paralysis of facial muscles, taste disturbance, inability to turn the head in the direction opposite to the damage, partial or complete drooping of the upper eyelid, hearing impairment with tinnitus, or even auditory hallucinations.
- Pain in the face.
Symptoms of an aneurysm
Two variants of the course of the disease can be distinguished: apoplexy and tumor-like. The characteristics of the clinical picture depend on the types of aneurysm. The tumor-like form of the disease is accompanied by an active course. In a short period of time, the aneurysm increases in size and compresses important anatomical structures of the brain.
A tumor-like aneurysm is most often localized in the area of the cavernous sinus or chiasm. When the chiasmal region is damaged, visual acuity decreases. Over a long period of time, optic nerve atrophy occurs. If a cerebral aneurysm is located in the cavernous sinus, paresis occurs and damage to the branches of the trigeminal nerve occurs. As the pathology develops, oculomotor disturbances occur and strabismus may appear.
Signs of a ruptured aneurysm
A sharp headache is the first symptom of a ruptured aneurysm. The pain syndrome is initially local in nature. But very quickly the headache spreads and becomes diffuse. In this case, patients note the appearance of nausea and repeated vomiting.
In the future, characteristic meningeal symptoms arise:
- stiffness of the neck muscles;
- Kernig's and Brudzinski's symptoms;
- loss of consciousness.
When a cerebral aneurysm ruptures, subarachnoid hemorrhage occurs. It may be accompanied by focal symptoms, which depend on the location of the formation. The most severe is hemorrhage into the ventricles, which often leads to the death of the patient.
With an aneurysm of the anterior cerebral artery, leg paresis develops, which is often combined with mental disorders. Damage to the middle cerebral artery leads to speech impairment and the development of hemiparesis.
If the pathology is localized in the area of the vertebrobasilar system, during the rupture of the aneurysm, swallowing disorders occur, nystagmus develops in combination with central paresis of the face and trigeminal nerve.
At the first sign of a possible aneurysm, you should immediately seek emergency medical help. It is important to maintain physical rest and avoid overexertion. Specialists will conduct an examination, diagnose, make an accurate diagnosis, and prescribe the necessary medications to reduce the risk of life-threatening complications.
Brain aneurysms
Department of Emergency Neurosurgery > Diseases
Content:
1. Structure of an aneurysm 2. Classification of aneurysms 3. Causes of cerebral aneurysms 4. Clinical picture of aneurysm rupture 5. Instrumental diagnosis 6. Complications of non-traumatic subarachnoid hemorrhage 7. Assessment of the severity of the patient’s condition 8. Surgical treatment of aneurysms 9. Postoperative management 10. Outcomes
A cerebral aneurysm (cerebral aneurysm, intracranial aneurysm) is a protrusion of the wall of an artery. Aneurysms are characterized by the absence of a normal, three-layer structure of the vascular wall. The wall of the aneurysm is represented only by connective tissue; the muscle layer and elastic membrane are absent. Rupture of a cerebral aneurysm is the most common cause of non-traumatic subarachnoid hemorrhage (more than 50%), in which blood enters the subarachnoid space of the brain.
Non-traumatic subarachnoid hemorrhage (NSAH) is one of the most severe and common forms of cerebrovascular accident. In the Russian Federation, the incidence of NSAC is about 13:100,000 population per year.
Most often, aneurysm rupture occurs in patients aged 40 to 60 years.
For the first time, a cerebral aneurysm was described in section by the Italian JB Morgagni in 1725. The first cerebral angiography for NSAC was performed in 1927 by the Portuguese E. Moniz, and in 1937 the American WE Dandy performed the first microsurgical intervention for the rupture of a cerebral aneurysm with its exclusion from the bloodstream using a silver clip.
At the Research Institute of SP named after. N.V. Sklifosovsky, the first operations for ruptured cerebral aneurysms began in 1979 under the leadership of Professor V.V. Lebedev.
Patients with cerebral aneurysms are admitted to our clinic mainly for emergency reasons.
Over the course of a year, the institute’s staff carries out more than 2,000 on-site consultations in hospitals in Moscow, of which about 40% are for patients with NSAC. At the Research Institute of SP named after N. During the year, V. Sklifosovsky’s visiting advisory team transfers more than 250 patients with ruptured cerebral aneurysms.
1. Structure of the aneurysm
An aneurysm is divided into a neck, body and dome. The neck of the aneurysm retains the three-layer structure of the vascular wall, therefore it is the most durable part of the aneurysm, while the dome is represented by only one layer of connective tissue, therefore the aneurysm wall in this part is the thinnest and most often susceptible to rupture (Fig. 1).
Rice. 1. The structure of the aneurysm during cerebral angiography: 1 - dome, 2 - body, 3 - neck, marked with a dotted line.
2. Classification of aneurysms
By form:
- saccular (Fig. 2)
- fusiform
- Fusiformes.
A)
b)
Fig. 2. Macroscopic specimens of cerebral aneurysms: a) giant saccular aneurysm of the anterior communicating artery; b) saccular aneurysm of the fork of the middle cerebral artery. Aneurysms are indicated by arrows.
By size:
- milliary (diameter up to 3 mm)
- regular size (4-15 mm)
- large (16-25mm)
- gigantic (more than 25 mm).
By the number of chambers in the aneurysm:
- single-chamber
- multi-chamber.
By localization:
- on the anterior cerebral - anterior communicating arteries (45%)
- on the internal carotid artery (26%)
- on the middle cerebral artery (25%)
- on the arteries of the vertebrobasilar system (4%)
- multiple aneurysms – on two or more arteries (15%).
3. Causes of cerebral aneurysms
Currently, there is no single theory of the origin of aneurysms. Most authors agree that the origin of aneurysms is multifactorial. There are so-called predisposing and producing factors.
Predisposing factors include those factors that result in changes in the normal vascular wall:
- hereditary factor - congenital defects in the muscular layer of the cerebral arteries (type III collagen deficiency), most often observed in places where the arteries bend, bifurcate or branch off from the artery of large branches. As a result, cerebral aneurysms are often combined with other developmental pathologies: polycystic kidney disease, hypoplasia of the renal arteries, coarctation of the aorta, etc.
- arterial injury
- bacterial, mycotic, tumor embolism
- exposure to radiation
- atherosclerosis, hyalinosis of the vascular wall.
Producing factors are those that directly result in the formation and rupture of an aneurysm.
The main producing factor is hemodynamic - an increase in blood pressure, a change from laminar blood flow to turbulent one. Its effect is most pronounced in places of arterial bifurcation, when an already altered vascular wall is subject to constant or periodic exposure to impaired blood flow. This leads to thinning of the vascular wall, the formation of an aneurysm and its rupture. 4. Clinical picture of aneurysm rupture
The symptoms of aneurysm rupture depend on the anatomical form of the hemorrhage, the location of the aneurysm, and the presence of complications of intracranial hemorrhage.
The typical clinical picture of aneurysm rupture develops in 75% of patients and has both general signs of non-traumatic subarachnoid hemorrhage and a number of features.
The disease most often begins suddenly with a severe headache of the “blow” type, which can be accompanied by nausea and vomiting, often against the background of physical activity, psycho-emotional stress, and increased blood pressure. The resulting headache is of a “burning”, “bursting” nature. Short-term and sometimes long-term disturbances of consciousness of varying degrees of severity (from moderate stupor to atonic coma), hyperthermia, and psychomotor agitation may occur.
Meningeal symptoms are observed in almost all cases of NSAH: the patient has a stiff neck, photophobia, increased sensitivity to noise, Kernig's, Brudzinsky's symptoms, etc.
Depending on the location of the aneurysm, various focal symptoms may occur:
- Aneurysms of the internal carotid artery are characterized by headache localization in the frontal or paraorbital region; Visual disturbances, paresis of the oculomotor nerve, contralateral hemiparesis, and sensory disturbances in the area of innervation of the I-II branches of the trigeminal nerve may occur.
- Rupture of an anterior cerebral - anterior communicating artery aneurysm is often accompanied by mental changes (emotional lability, psychotic disorders, decreased intelligence, memory impairment, concentration disorders, etc.). Electrolyte disturbances, diabetes insipidus, and contralateral hemiparesis, more pronounced in the leg, may be observed.
- rupture of an aneurysm of the middle cerebral artery is characterized by the development of contralateral hemiparesis, more pronounced in the arm, or hemiplegia, contralateral hemihypesthesia, motor and/or sensory aphasia (with damage to the dominant hemisphere), visual impairment such as homonymous hemianopia, and convulsive seizures.
- with aneurysms of the basilar artery, unilateral or bilateral paresis of the oculomotor nerve, Parinaud's symptom, vertical or rotatory nystagmus, and ophthalmoplegia often occur. Alternating syndromes, homonymous hemianopsia or cortical blindness, and the development of tetraparesis are possible. With massive hemorrhage, the level of consciousness is depressed to the point of coma, the patient has wide pupils without a photoreaction, and breathing problems occur.
- Aneurysms of the vertebral artery are characterized by the occurrence of dysphagia, dysarthria, hemiatrophy of the tongue, impairment or loss of vibration sensitivity, decreased pain and temperature sensitivity, and dysesthesia in the legs. With massive hemorrhage - coma, respiratory failure.
In approximately every 4 patients (about 25%), atypical variants of the course of aneurysm rupture are observed, when the hemorrhage is “masked” as other diseases.
Such patients may be diagnosed with “hypertensive crisis”, “migraine”, “acute food poisoning”, “acute psychosis”, “sciatica”, “meningitis”, etc., which leads to hospitalization of patients in non-core institutions and untimely provision of necessary medical care . When cerebral aneurysms rupture, both subarachnoid hemorrhage itself and intracerebral and/or intraventricular hemorrhage can occur.
With all anatomical forms of hemorrhage, occlusion of the cerebrospinal fluid pathways may occur with the development of acute occlusive hydrocephalus and brain dislocation.
5. Instrumental diagnostics
To identify non-traumatic subarachnoid hemorrhage due to rupture of aneurysms, determine the prognosis of the disease, the likelihood of complications, and develop treatment tactics, a number of instrumental diagnostic methods are used.
Lumbar puncture – makes it possible to detect subarachnoid hemorrhage with a high degree of probability. On the first day after hemorrhage, the cerebrospinal fluid is intensely and evenly colored with blood; after a few days it becomes xanthochromic. Puncture is contraindicated if the patient has an intracranial space-occupying process (hematoma, massive ischemic focus), since even a small removal of cerebrospinal fluid can lead to the development of acute dislocation of the brain stem. In order to avoid this, patients with clinical manifestations of an intracranial space-occupying process should undergo echoencephaloscopy or computed tomography of the brain before lumbar puncture.
Computed tomography of the brain (CT) is the leading method for diagnosing NSAH, especially in the first day of the disease. Using CT, not only the presence of hemorrhage is determined, but also its intensity, prevalence, the presence and volume of intracerebral hematoma and intraventricular hemorrhage, foci of ischemia, the severity and nature of hydrocephalus, and dislocation syndrome.
In addition, with the help of CT of the brain, it is sometimes possible to establish the true cause of hemorrhage, topographic-anatomical relationships, especially if the study is supplemented with contrast enhancement and 3D reconstruction.
The detection rate of NSAC in the first 12 hours after hemorrhage using CT reaches 95.2%, within 48 hours - 80-87%, on days 3-5 - 75%, on days 6-21 - only 29%. Severe basal SAH is almost always prognostically unfavorable, since in almost all patients it is accompanied by the development of vasospasm, leading to the development of ischemia. The high information content of brain CT and the prognostic significance of the results obtained, as well as the speed of the study, make this method mandatory when examining patients with ruptured cerebral aneurysms (Fig. 3).
A)
b)
V)
Rice. 3. a) Computed tomography of the brain. Massive basal subarachnoid hemorrhage due to rupture of an aneurysm of the anterior communicating artery (indicated by arrows); b) CT angiography of intracranial arteries (2D reformation). Fusiform aneurysm of the right internal carotid and anterior cerebral arteries. c) CT angiography of intracranial arteries (3D reformation). Saccular aneurysm of the bifurcation of the left internal carotid artery. Aneurysms are indicated by arrows.
Magnetic resonance imaging (MRI) - this diagnostic method has high sensitivity and specificity. If CT of the brain has excellent detection of SAH and aneurysms in the acute period of hemorrhage, then MRI is indispensable in detecting hemorrhages in the subacute and chronic periods. Verification of aneurysms with magnetic resonance angiography (MR-AG) reaches 80-100%, which allows in some cases to abandon traditional invasive cerebral angiography (CAG) when for some reason it is contraindicated (for example, with individual intolerance to iodine preparations) (Fig. . 4).
A)
b)
Rice. 4. a) Magnetic resonance imaging. Partially thrombosed aneurysm of the right internal carotid artery. b) MR angiography of intracranial arteries. Saccular aneurysm of the anterior communicating artery. Aneurysms are indicated by arrows.
During an MRI examination, the hemorrhage appears as hyperintense (bright) or hypointense (dark) on the resulting images, depending on the duration of the hemorrhage.
Also, MRI of the brain with a high degree of reliability allows you to verify ischemia and determine its nature.
Digital subtraction cerebral angiography is the “gold standard” for the most accurate identification of the cause of hemorrhage. It is mandatory to study two carotid and two vertebral basins in direct, lateral and oblique projections.
Cerebral angiography can not only detect an aneurysm (Fig. 5), but also vascular spasm (Fig. 9b).
A)
b)
Rice. 5. Cerebral angiography. a) Cerebral angiogram in direct projection. Aneurysm of the left internal carotid artery. b) Cerebral angiogram in lateral projection. Aneurysm of the anterior communicating artery. Aneurysms are indicated by arrows.
Electroencephalography (EEG) is an instrumental diagnostic method that allows you to identify disturbances in the electrical activity of the brain. When recording the electrical activity of the brain in SAH, the type of EEG is determined. Determining the type of disturbance in the electrical activity of the brain allows us to clarify the timing of the operation.
So, with EEG types I and II, surgical interventions for ruptured aneurysms have a favorable prognosis. In type III, surgical intervention is not advisable, although it is possible with a high risk of re-rupture of the aneurysm. Type IV is the most unfavorable prognostically. There are pronounced disturbances in the electrical activity of the brain. Surgery with this type of EEG can only be performed for health reasons (for example, in case of acute compression of the brain by a hematoma) (Fig. 6).
a) b)
Rice. 6. EEG in case of rupture of a cerebral aneurysm: a) type I; b) IV type.
An electroencephalographic study in a situation where there are multiple aneurysms and it is unclear which of them is the cause of the hemorrhage, makes it possible to identify a ruptured aneurysm (usually by the predominance of changes in electrical activity in a particular area of the brain).
Transcranial Dopplerography (TDCG) is a method that can significantly expand the diagnosis of vasospasm. With TDCG, it is possible to determine the linear blood flow velocity (LBV) in the main arteries of the brain, the severity of spasm (the degree of narrowing of the artery lumen), the localization of spasm and the dynamics of its development. When the linear speed of blood flow through the arteries of the base of the brain increases above 120 cm/s, vascular spasm is considered moderate; when the blood flow speed exceeds 200 cm/s, it is pronounced. Angiospasm is assessed as non-widespread if it covers 1-2 arteries of the circle of Willis, and widespread when there is spasm of 3 or more arteries (Fig. 7).
a) b)
Rice. 7. a) TCD, norm: average blood flow velocity in the middle cerebral artery – 90 cm/s; b) TCD, vasospasm: the average blood flow velocity in the middle cerebral artery is 260 cm/s.
With increasing vascular spasm and the presence of clinical manifestations, surgical intervention is possible only with increasing dislocation of the brain due to intracranial hematoma or ischemia causing mass effect.
6. Complications of non-traumatic subarachnoid hemorrhage
The most common complications of subarachnoid hemorrhage due to aneurysm rupture include the following:
- Recurrent rupture of the aneurysm (Fig. 8).
A)
b)
V)Rice. 8. a) CT scan of the brain. First rupture of anterior communicating artery aneurysm. b) Cerebral angiography, lateral projection, aneurysm of the anterior communicating artery is indicated by an arrow. c) CT scan of the finished brain. Repeated rupture (after 3 days) of the anterior communicating artery aneurysm (hemorrhage is indicated by an arrow).
- Cerebral vasospasm (peak development 3-14 days after aneurysm rupture).
- Cerebral ischemia develops in more than 60% of patients with SAH, and in 15-17% of patients it is the main cause of death after aneurysm rupture (Fig. 9).
A)
b)
V)Rice. 9. a) CT scan of the brain. Massive basal subarachnoid hemorrhage (indicated by arrows). b) Cerebral angiogram, oblique projection, a ruptured aneurysm of the anterior communicating artery is indicated by a thick arrow, spasm of the anterior cerebral artery is indicated by two thin arrows. c) CT scan of the brain. Foci of ischemia as a result of widespread decompensated cerebral vasospasm are indicated by arrows.
- Internal hydrocephalus, caused by occlusion of the cerebrospinal fluid ducts, occurs in 25-27% of patients (Fig. 10).
Rice. 10. Massive basal SAH with intraventricular hemorrhage and the development of internal hydrocephalus.
7. Assessment of the severity of the patient’s condition
With all the diversity of the clinical picture of the course and complications of subarachnoid hemorrhage, only a few classifications of the severity of the patient’s condition are used in practice (Tables 1 and 2).
Table 1.
Assessment of level of consciousness using the Glasgow Coma Scale (recommended for ages 4 years and older).
| Points (3-15) | Opening your eyes | Voice contact | Physical activity |
| 6 | — | — | Executing commands |
| 5 | — | Orientation | Localization of pain (targeted) |
| 4 | Spontaneous | Confusion | Withdrawal of a limb (non-targeted) |
| 3 | To appeal | Inadequate (unintelligible words) | Limb flexion (decortication) |
| 2 | For pain* | Inappropriate (inarticulate sounds) | Limb extension (decerebration) |
| 1 | No | No | No# |
* when checking eye opening for pain, peripheral stimulation should be used (a painful grimace during central pain stimulation leads to squinting of the eyes) # in the absence of a motor response, it is necessary to exclude damage to the spinal cord.
Table 2.
Assessment of the severity of patients’ condition using the W. Hunt – R. Hess scale, 1968.
| Degree | Description |
| I | Asymptomatic, or mild headache and mild neck stiffness. |
| II | Moderate or severe headache, stiff neck, paresis of the cranial nerve (oculomotor). |
| III | Stupefaction, drowsiness, confusion. Moderate neurological deficit. |
| IV | Stupor, moderate or severe hemiparesis, early decerebrate rigidity. |
| V | Coma of varying depth, decerebrate rigidity. |
- in the presence of a serious general disease (hypertension, diabetes mellitus, severe atherosclerosis, chronic obstructive pulmonary disease) or severe vasospasm, the assessment of the severity of the patient’s condition is increased by one degree
- the original work did not take into account the age of the patients, the location of the aneurysms, or the time since the hemorrhage; The severity of the patients was assessed upon admission and before surgery.
The creation of such scales for assessing the severity of the condition is due to the need to standardize data on the study of examination results, conservative and surgical treatment of patients with NSAH, and prognosis of the outcome of the disease.
8. Surgical treatment of aneurysms
The choice of treatment tactics is determined by the location of the aneurysm, the presence or absence of its rupture, the time period from the moment of hemorrhage, the clinical condition of the patient, and the presence of complications.
Surgical treatment is indicated for all patients with aneurysms.
For patients with unruptured aneurysms, the timing of surgery is usually not of great importance, since the probability of aneurysm rupture is 1-2% per year. It is important that the operation is performed in a vascular center that has experience in such operations, minimal rates of mortality, disability, and complications.
Patients with ruptured aneurysms should strive to perform surgical treatment to exclude the aneurysm from the bloodstream as early as possible, since the risk of re-hemorrhage in the first two weeks from a ruptured aneurysm is 15-25%.
In the acute (up to 3 days) and acute period of NSAH (up to 14 days), due to rupture of an aneurysm, surgical treatment is performed for patients with an uncomplicated course of the disease (I-II, III degree of severity according to HH), a compensated condition of the patient, as well as for patients those at risk of recurrent bleeding from the aneurysm or the development of clinically significant vasospasm.
Also, according to vital indications, patients with IV-V severity of H-H are operated on, who have acute compression of the brain by a hematoma, severe occlusive hydrocephalus with dislocation of the brain stem, and extensive foci of ischemia. In such patients, surgery is considered as a stage of resuscitation.
In the delayed period of SAH (after 14 days), surgical treatment of patients is performed in case of a complicated course of the disease due to vasospasm with a severe condition (HH IV, V degree of severity according to HH) after improvement of the patient’s condition, as well as in the presence of an aneurysm of a hard-to-reach localization.
The presence of such serious complications in the patient as re-rupture of the aneurysm and the development of vasospasm significantly influence the choice of successful surgical tactics.
If the aneurysm ruptures again, in the case of a compensated condition of the patient, emergency surgery is indicated to exclude the aneurysm from the bloodstream. If it is impossible to carry it out due to the severity of the condition, stay in the neurointensive care unit and perform palliative operations: installation of intracranial pressure sensors, drainage of the ventricular system of the brain, installation of microdialysis and tissue oxygen tension sensors.
The tactics of surgical treatment of ruptured aneurysms in the acute period of hemorrhage with the development of cerebral vasospasm is one of the most difficult issues in aneurysm surgery.
The form of development of cerebral ischemia is decisive: with a compensated form of cerebral ischemia, patients can be operated on immediately after identifying an aneurysm; with a subcompensated form of cerebral ischemia, a wait-and-see approach is advisable in patients in accordance with the dynamics of ischemia; with decompensated cerebral ischemia, surgical intervention must be postponed and treated patients in neuroreanimation.
Currently, two main methods are used to exclude aneurysms from the bloodstream:
- open microsurgery
- endovascular intervention.
In some cases, in patients in serious condition, combined treatment is used - first, endovasal embolization of the aneurysm (to prevent re-hemorrhage), then, after the patient’s condition improves, open intervention.
An open microsurgical operation is performed under general anesthesia, with the obligatory use of an operating microscope and microsurgical equipment (Fig. 11).
a B C D E)
Rice. 11. Operating room equipment for microsurgical operations: a) operating table and rigid head fixation bracket (Mayfield-Kiss); b) operating microscope OPMI Neuro on the NC 4 platform; c) “Cellsaver” blood reinfusion apparatus and Karl Storz endoscopic stand; d) electrotrephine Aesculap; e) Stryker electric trepan.
Open surgery includes several stages:
- Trepanation of the skull
- Opening the dura mater
- Arachnoid dissection with isolation of the great vessels of the base of the brain and aneurysm
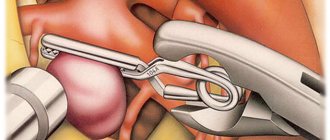
- Switching off the aneurysm from the bloodstream by clipping (Fig. 12)
- Closure of the surgical wound.
Rice. 12. Intraoperative photo. Pterional anterolateral subfrontal approach on the left. A ruptured aneurysm of the anterior communicating artery was clipped. The aneurysm dome and clip are indicated by arrows.
The rate of exclusion of aneurysms from the bloodstream during open operations reaches 98% (Fig. 13).
a) b)
Rice. 13. Clipping of an aneurysm of the left internal carotid artery: a) cerebral angiography before surgery, an aneurysm (arrow) of the supraclinoid section of the left internal carotid artery was detected; b) cerebral angiography after surgery, the aneurysm is not contrasted, the arrow indicates the clips on the neck of the aneurysm.
To control the radicality of aneurysm clipping and preserve blood flow along the functionally significant branches of the main arteries of the base of the brain, intraoperative Doppler sonography is used (Fig. 14).
a B C)
Rice. 14. Use of intraoperative Dopplerography when clipping an aneurysm of the left middle cerebral artery: a) intraoperative photograph: aneurysm (arrow) of the fork of the left middle cerebral artery with turbulent blood flow according to intraoperative Dopplerography; b) intraoperative photograph: the aneurysm of the bifurcation of the left middle cerebral artery is clipped, a microsensor (arrow) is installed on the M1 segment of the middle cerebral artery to record blood flow in it; c) intraoperative photograph: in the clipped aneurysm (arrow), blood flow is not recorded according to intraoperative Dopplerography; normal blood flow is preserved along the M2 segment of the left middle cerebral artery.
Endovasal intervention is performed when it is impossible to clip the aneurysm during open intervention, in case of aneurysms of difficult-to-reach localization (aneurysms of the vessels of the vertebrobasilar region, aneurysms of the internal carotid artery proximal to the ophthalmic segment), in elderly patients (over 75 years old). Endovasal surgery involves inserting a detachable Serbinenko balloon-catheter or electrically detachable Guglielmi platinum microspirals into the aneurysm cavity. Thanks to microcoils, thrombus formation occurs in the cavity of the aneurysm, as a result of which it is switched off from the bloodstream.
The rate of exclusion of aneurysms from the bloodstream during endovasal interventions is more than 85% (Fig. 15, 16).
Rice. 15. Diagram of aneurysm occlusion with microcoils.
A)
b)
Rice. 16. Embolization of basilar artery aneurysm. a) Cerebral angiogram, lateral projection, the arrow indicates the aneurysm of the basilar artery. b) Cerebral angiogram, lateral projection, the arrow indicates the aneurysm after embolization with microcoils.
9. Postoperative management
From the operating room, regardless of the severity of the condition, the patient is transferred to the neurointensive care unit. This department monitors the patient’s condition and prevents complications. If within 24 hours the patient’s condition is assessed as satisfactory or moderate, he is transferred to the neurosurgical department. If there is a deterioration in the condition, then an emergency CT scan of the brain, TDCG, is performed. Based on the results of these examinations, further tactics for patient management are determined.
10. Outcomes
Surgical activity for ruptured aneurysms in our clinic is 82–90%. For most patients, exclusion of aneurysms from the bloodstream is performed openly (92%), endovascularly – 8%. The overall postoperative mortality rate is 10-12%.
How is it diagnosed?
Since an arterial aneurysm can occur without significant symptoms, it is necessary to pay special attention to the first signs in women and men. A neurologist must diagnose the disease based on the examination, the diagnostic results obtained and the study of cerebrospinal fluid.
During a neurological examination, focal and meningeal symptoms are detected. Based on the location of complaints, it is possible to determine presumably where the pathological focus is located.
The neurologist obtains accurate information about the patient’s condition using the following studies:
- X-ray of the skull. A cerebral aneurysm is characterized by signs of bone tissue destruction.
- Computed tomography, magnetic resonance imaging of the brain.
- Angiography. Basic information about the location, shape and size of the brain aneurysm can be obtained.
- Lumbar puncture. The study reveals blood in the cerebrospinal fluid, which indicates the presence of hemorrhage.
Specialists carry out differential diagnosis of cerebral aneurysm. It is important to make an accurate diagnosis in a short time. This will avoid the adverse effects of a brain aneurysm. It is necessary to differentiate an aneurysm from tumor-like processes, cysts and abscesses.
Principles of treatment
Aneurysm treatment is carried out by a neurologist. The operation is performed only by a neurosurgeon. Surgical methods are aimed primarily at preventing aneurysm rupture, which can result in the death of the patient. Conservative therapy for this pathology is used to slow the progression of the disease.
Surgical treatment of a cerebral aneurysm involves two types of main operations: clipping and endovascular occlusion. Surgery prevents the aneurysm from rupturing. A radical method of treatment is the removal of arteriovenous malformation during a microsurgical operation.
Aneurysm clipping
Aneurysm clipping is an open operation during which the neurosurgeon blocks blood flow in a certain area of the vessel and applies a clip. At the stage of preparation for surgery, specialists prescribe a procedure that allows them to stabilize the patient’s condition and minimize the risk of possible complications. Preventive examination makes it possible to identify possible disorders and diseases that can lead to adverse consequences of surgical intervention.
The operation is performed using modern microsurgical techniques through a small trepanation hole. During surgery, the neurosurgeon prevents rupture of the wall of the malformation.
After isolating the neck of the aneurysm, the specialist places a clip on it. Additional control with Doppler ultrasound allows you to assess the state of blood flow and ensure the effectiveness of the operation.
Treatment of an aneurysm using the clipping method is considered quite complex and should only be performed by an experienced neurosurgeon. A qualified specialist will do everything possible to ensure accurate and technically correct application of the clip. Otherwise, dangerous complications and a long rehabilitation period cannot be avoided.
The clip is applied to the neck of the aneurysm vessel. The accuracy of the neurosurgeon’s actions is confirmed by conducting high-quality diagnostics (Dopplerography) during the procedure.
Endovascular occlusion
During endovascular occlusion of an aneurysm, the neurosurgeon blocks the lumen of the dilated vessel with a special implant. The operation is used when clipping is not possible, for example, when the aneurysm is spindle-shaped. During surgery, a specialist inserts a catheter balloon through the femoral artery using angiographic control. It closes the lumen of the aneurysm. You can also use a microspiral to perform thrombosis. The choice remains with the attending physician. The microspiral in the cavity of the affected vascular area forms blood clots, which clog the lumen of the vessel and shut off the aneurysms from the blood circulation.
Technology
Currently available clipping devices consist of a manual catheter delivery system that allows the design of stainless steel clips with two serrated jaws to mechanically compress the targeted vessels and/or close the mucosal defect by tightening the tissue. The clip has no chemical or thermal effect to damage the mucosa, and thus clipping causes minimal trauma to the mucosa. The applied clips are spontaneously rejected into the lumen of the organ after about 2-3 weeks and naturally leave the human body. Complications caused by clipping are extremely rare.
Rehabilitation after surgical treatment of an aneurysm
The rehabilitation period takes place under the supervision of specialists. Professionals do everything necessary to prevent the occurrence of postoperative complications. The patient remains in the intensive care unit for several days under the constant supervision of specialists. Afterwards, the patient is transferred to a general ward, where strict bed rest must be observed for some time. The return to a normal lifestyle occurs gradually.
If the patient's well-being worsens after surgery, transcranial Doppler ultrasound may be prescribed. Rehabilitation is aimed primarily at preventing vasospasm and increased blood pressure. Specialists also monitor the general condition of the cardiovascular system and, if necessary, prescribe osmodiuretics to eliminate swelling of the brain tissue. Additionally, anti-inflammatory therapy is carried out.
Rehabilitation after surgical treatment of an aneurysm necessarily includes a program to restore impaired body functions and further socialize the patient. The recovery period lasts at least 6 months. With the help of high-quality rehabilitation, it is possible, among other things, to eliminate the adverse consequences of surgical treatment.
Rehabilitation measures include physiotherapy, massage, and the implementation of an individually selected rehabilitation program. After endoscopic clipping, the patient can return to normal life within a few weeks.
Forecast for life
The prognosis of the disease depends on the location of the vascular protrusion and its size. The initial condition of the patient also has a huge impact. The mortality rate in case of rupture of a cerebral aneurysm exceeds 30-50%. Surviving patients sometimes retain the consequences of the condition in the form of movement restrictions, cognitive impairment and a significant decrease in quality of life. Mortality after recurrent hemorrhage exceeds 70%.
Therefore, it is so important to carry out surgical treatment in time, turning to a qualified neurosurgeon. The operation is postponed only if there are certain medical indications.
Successful neurosurgical operations are carried out at the Burdenko Research Institute. Patients with signs of an aneurysm or suspected aneurysm are admitted here. At the Institute of Neurosurgery, it is possible to carry out comprehensive diagnostics using the latest technology and further treatment of identified diseases.
Aneurysm in Israel: prices for treatment
The cost of treating a cerebral aneurysm in Israel is 30-50% cheaper than in Europe and America, with the highest level of treatment and diagnostic process. Prices for treatment of a cerebral aneurysm are determined strictly individually, so from our consultants you can only find out the approximate cost of surgery to remove a cerebral aneurysm.
Diagnostic prices from $3000
from $3000 to $35000
Brain aneurysm
| Type of service | Prices |
| Diagnostics | from $3000 |
| Operation | from $35000 |
To find out the exact prices for treatment, please provide your phone number and a clinic representative will contact you as soon as possible.
|form|
Cerebral aneurysm in Israel: benefits of treatment
- Thanks to modern equipment and highly qualified staff of our clinic, we are able to detect pathology in the initial stages of development, which contributes to successful treatment.
- Only surgical treatment of a brain aneurysm in Israel will help to avoid serious consequences. The surgeons working at the Assuta clinic are world-class specialists, which guarantees a successful outcome of the operation.
- Our clinic always uses an individual approach when choosing treatment methods. Therefore, in the fight against disease, victory is always on our side.
- The promptness of medical care provided by Israeli doctors will help avoid danger. We achieve success even when in the CIS the patient is considered hopeless.
- Our prices
Treatment of cerebral aneurysm in Israel: reviews
Igor, 39 years old, Kharkov When a threat to my life arose due to a ruptured brain aneurysm, I did not hesitate and went to Israel to the Assuta clinic. Diagnostics in 3 days is not fiction, but the truth. The operation also lasted about an hour. After the operation, I immediately stood up on my own and felt fine. I am very glad that I put my health in the hands of real professionals.
- 5
- 4
- 3
- 2
- 1
(12 votes, average: 5 out of 5)