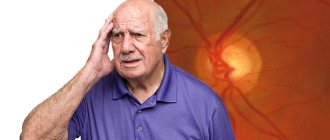
If adequate treatment for high blood pressure is not carried out, there is a high risk of developing severe complications - such as, for example, cerebral hemorrhage, myocardial infarction, etc. Sometimes with high blood pressure, so-called hypertensive retinal angiopathy is observed, which is characterized by damage to blood vessels, providing nutrition to the retina. In advanced cases, hemophthalmos (in other words, hemorrhage in the eye), retinal detachment and blindness may develop.
What it is?
Hypertensive angioretinopathy (HAR) is a pathological change in the vessels of the fundus and the retina itself against the background of hypertension1.
High blood pressure (hypertension) causes a narrowing of blood vessels throughout the body, including the tiny thin vessels that supply blood to the retina. Fundus examination for hypertension is a mandatory examination and allows detecting changes in the early stages of hypertension1.
As a result, your vision may deteriorate. The higher your blood pressure and the longer it is elevated, the higher your risk of developing GAP. The most deplorable outcome of GAD is complete loss of vision.
Hypertension is a chronic disease in which blood vessels narrow. Subsequently, organic changes in blood vessels appear in the form of atherosclerosis. Against this background, blood supply and nutrition to organs is disrupted. Pathological changes occur. One of the main symptoms of hypertension is increased blood pressure2.
It is damaged blood vessels that lead to many health problems. Against the background of impaired blood flow, hemorrhage or swelling of the retina may occur. Retinal hemodynamic disturbances have diagnostic and prognostic significance in assessing the course of hypertension3.
Classification of pathology
According to the nature of damage to the visual organ, retinal angiopathy of the hypertensive type has several degrees of development. The typology of hypertensive angiopathy given in the table is based on data from an ophthalmologist examination:
| Angiopathy degree | Nature of the pathology | Clinical picture |
| Retinal angiopathy degree I | physiological |
There are no obvious symptoms; the patient is usually unaware of the development of pathological processes. |
| Retinal angiopathy degree II | organic |
The patient experiences discomfort and a burning sensation. There is a sharp decrease in visual function. |
| Retinal angiopathy degree III | angioretinopathy |
There are intense degenerative transformations of the arteries and retina, leading to its complete/partial detachment. Threatens vision loss. |
Since hypertension affects the vascular system of the entire body, retinal angiopathy of both eyes develops over time.
Therefore, when diagnosing hypertension, you need to undergo regular examinations with an ophthalmologist in order to detect the pathology at the initial stage and begin timely treatment. The advanced course of hypertensive angiopathy can provoke microinfarctions of the fundus, as a result of which vision deteriorates significantly and the eyes become cloudy. If treatment is not carried out properly, then there is a high risk of developing irreversible damage to the visual organ.
Symptoms
Symptoms usually do not appear until late in the disease and include1:
- Decreased vision: You see blurry or just worse than before
- Significant redness of the eyes: as a rule, it is associated with rupture of the blood vessels of the conjunctiva (atherosclerotically damaged), which could not withstand the increased pressure
- Double vision: You see double
- Headaches: occur due to impaired blood flow
Seek medical help immediately if you have hypertension and suddenly have decreased vision!
Risk factors
Hypertensive angioretinopathy usually occurs after your blood pressure has been persistently high for a long time. There are several factors that increase the risk of developing this disease4.
- Lack of physical activity. It harms already damaged vessels. But everything needs to be done in moderation: some exercises can increase blood pressure even more.
- Overweight. The fact is that pressure increases with increasing body weight.
- Constant stress. Stress affects the cardiovascular system and also increases blood pressure.
- Alcohol and smoking. Abuse of both negatively affects the entire body: including the condition of blood vessels.
- Heredity. Predisposition to hypertension is inherited. Several dozen genes are responsible for this, which together increase the risk of cardiovascular disease. Accordingly, the risk of developing hypertensive retinopathy also increases.
Reasons for the development of angiopathy
The following reasons can lead to angiopathy:
- Diabetes.
- Hypertension.
- Endocrine diseases.
- Cervical osteochondrosis.
- Atherosclerosis.
- Blood diseases.
- Injuries.
- Elderly age.
- Smoking, alcohol abuse.
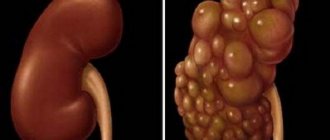
It is important to understand that retinal angiopathy Retina
- the inner layer of the eye, an important part of the visual analyzer. It is she who is responsible for the process of converting light into a nerve impulse, which is transmitted to the brain. does not occur on its own - it is always the result of the development of another general disease of the body.
Stages
The grade and stages of angioretinopathy are usually presented on a scale of 1 to 4. The scale is called the Keith-Wagener-Barker classification system. In Russia it is customary to use the classification of M.L. Krasnova.
Here are the four degrees of hypertensive angioretinopathy2:
- Grade I - hypertensive angiopathy: the retinal arteries narrow, the retinal veins dilate, and vascular tortuosity appears. In this case, the person does not feel any discomfort, there are no symptoms.
- Degree II - hypertensive angiosclerosis: there is a more serious narrowing of the arteries, thickening of the arterial walls. Narrow constrictions appear - known as symptoms of arteriovenous crossover. In some cases, vision may deteriorate.
- Grade III - hypertensive retinopathy: the most common symptom is retinal hemorrhages. Retinal edema also appears. Vision deteriorates, the degree of deterioration varies.
- Grade IV - hypertensive neuroretinopathy: At this stage, swelling of the optic nerve and the center of the retina - the macula - may begin. A person may be at risk of complete loss of vision.
Fundus changes in hypertension
Nesterov AP The article consists of the lecture for physicians and ophthalmologists. Symptoms of functional changes in the central retinal vessels, features of hypertonic angiosclerosis of retinal vessels, peculiarities of hypertonic retinopathy and neuroretinopathy are discussed in the article and recommendations for treatment of the hypertonic retinopathy are given.
The frequency of fundus lesions in patients with essential hypertension (HD), according to various authors, varies from 50 to 95% [1]. This difference is caused partly by age and clinical differences in the patient population studied, but mainly by the difficulty of interpreting the initial changes in the retinal vessels in hypertension. Internists attach great importance to such changes in the early diagnosis of hypertension, determining its stage and phase, as well as the effectiveness of the therapy. The most interesting in this regard are the studies of R. Salus. In a well-organized experiment, he showed that the diagnosis of headache, made by him based on the results of ophthalmoscopy, turned out to be correct only in 70% of cases. Misdiagnosis is associated with significant interindividual variation in retinal vessels in healthy individuals, and some of the variations (relatively narrow arteries, increased vascular tortuosity, crossover sign) may be misinterpreted as hypertensive changes. According to the observations of O.I. Shershevskaya [7], during a single check of an unselected contingent of HD patients, specific changes in the retinal vessels are not detected in 25–30% of them in the functional period of the disease and in 5–10% in the late phase of the disease. Vessels of the retina and optic nerve The central retinal artery (CRA) in its orbital section has a structure typical of medium-sized arteries. After passing through the cribriform plate of the sclera, the thickness of the vascular wall is halved due to thinning (from 20 to 10 µm) of all its layers. Within the eye, the CAS is repeatedly divided dichotomously. Starting from the second bifurcation, the branches of the CAS lose their inherent characteristics of arteries and turn into arterioles. The intraocular part of the optic nerve is supplied mainly (with the exception of the neuroretinal layer of the optic disc) from the posterior ciliary arteries. Posterior to the lamina cribrosa of the sclera, the optic nerve is supplied by centrifugal arterial branches originating from the CAS and centropetal vessels originating from the ophthalmic artery. The capillaries of the retina and optic disc have a lumen with a diameter of about 5 µm. They start from precapillary arterioles and connect to venules. The endothelium of the capillaries of the retina and optic nerve forms a continuous layer with tight junctions between cells. Retinal capillaries also have intramural pericytes, which are involved in the regulation of blood flow. The only blood collector for both the retina and the optic disc is the central retinal vein (CRV). The adverse effects of various factors on retinal blood circulation are smoothed out due to vascular autoregulation, which ensures optimal blood flow using local vascular mechanisms. This blood flow ensures the normal course of metabolic processes in the retina and optic nerve. Pathomorphology of retinal vessels in HD Pathomorphological changes in the initial transient stage of the disease consist of hypertrophy of the muscle layer and elastic structures in small arteries and arterioles. Stable arterial hypertension leads to hypoxia, endothelial dysfunction, plasmatic saturation of the vascular wall with subsequent hyalinosis and arteriolosclerosis [3]. In severe cases, fibrinoid necrosis of arterioles is accompanied by thrombosis, hemorrhages and microinfarctions of retinal tissue. Retinal vessels in hypertension Two vascular trees are clearly visible in the fundus: arterial and venous. It is necessary to distinguish: (1) the severity of each of them, (2) the characteristics of branching, (3) the ratio of the caliber of arteries and veins, (4) the degree of tortuosity of individual branches, (5) the nature of the light reflex on the arteries. The severity and richness of the arterial tree depend on the intensity of blood flow in the central nervous system, refraction and the condition of the vascular wall. The more intense the blood flow, the better the small arterial branches are visible and the more branched the vascular tree. With hypermetropia, the retinal vessels appear wider and brighter during ophthalmoscopy than with emmetropia, and with myopia they become paler. Age-related thickening of the vascular wall makes small branches less noticeable, and the arterial tree of the fundus in elderly people looks depleted. With hypertension, the arterial tree often looks poor due to tonic contraction of the arteries and sclerotic changes in their walls. Venous vessels, on the contrary, often become more pronounced and acquire a darker, more saturated color (Fig. 4, 1, 5). It should be noted that in some cases, provided that the elasticity of the blood vessels is preserved, patients with hypertension experience not only venous, but also arterial congestion. Changes in the arterial and venous vascular beds also manifest themselves in changes in the arteriovenous ratio of retinal vessels. Normally, this ratio is approximately 2:3; in patients with hypertension it often decreases due to narrowing of the arteries and dilation of the veins (Fig. 1, 2, 5). Narrowing of retinal arterioles in hypertension is not a necessary symptom. According to our observations [3], pronounced narrowing, which can be determined clinically, occurs only in half of the cases. Often only individual arterioles narrow (Fig. 2, 5). The unevenness of this symptom is characteristic. It is manifested by asymmetry of the state of the arteries in paired eyes, narrowing of only individual vascular branches, and uneven caliber of the same vessel. In the functional phase of the disease, these symptoms are caused by unequal tonic contraction of the vessels, in the sclerotic phase - by uneven thickening of their walls. Much less often than narrowing of the arteries, with hypertension, their dilation is observed. Sometimes both narrowing and dilation of arteries and veins can be seen in the same eye and even on the same vessel. In the latter case, the artery takes on the appearance of an uneven chain with swellings and interceptions (Fig. 5, 7, 9). One of the common symptoms of hypertensive angiopathy is disruption of the normal branching of the retinal arteries. Typically, the arteries branch dichotomously at an acute angle. Under the influence of increased pulse beats in hypertensive patients, this angle tends to increase, and it is often possible to see branching of the arteries at right or even obtuse angles (“bull horns symptom”, Fig. 3). The greater the branching angle, the greater the resistance to blood movement in this zone, the stronger the tendency to sclerotic changes, thrombosis and disruption of the integrity of the vascular wall. High blood pressure and large pulse amplitude are accompanied by an increase in not only lateral, but also longitudinal stretching of the vascular wall, which leads to lengthening and tortuosity of the vessel (Fig. 5, 7, 9). In 10–20% of patients with hypertension, tortuosity of the perimacular venules is also observed (Gwist's sign). The Hun–Salus intersection symptom is essential for the diagnosis of fundus hypertonicity. The essence of the symptom is that at the point of intersection of the venous vessel with a condensed artery, partial compression of the latter occurs. There are three clinical grades of this symptom (Fig. 4). The first degree is characterized by a narrowing of the lumen of the vein under the artery and near the intersection of the vessels. A feature of the second degree is not only partial compression of the vein, but also its displacement to the side and into the thickness of the retina (“arch symptom”). The third degree of vascular decussation is also characterized by an arch symptom, but the vein under the artery is not visible and seems completely compressed. The symptom of decussation and venous compression is one of the most common in hypertension. However, this symptom can also be found in retinal arteriosclerosis without vascular hypertension. Symptoms pathognomonic for retinal arteriosclerosis in hypertension include the appearance of side stripes (“cases”) along the vessel, symptoms of “copper” and “silver” wire (Fig. 5). The appearance of white lateral stripes is explained by thickening and decreased transparency of the vascular wall. The stripes are visible along the edge of the vessel, since there is a thicker layer of the wall and a thinner layer of blood compared to the central part of the vessel. At the same time, the light reflex from the front surface of the vessel becomes wider and less bright. The symptoms of copper and silver wire (the terms were proposed by M. Gunn in 1898) are interpreted ambiguously by various authors. We adhere to the following description of these symptoms. The copper wire symptom is found mainly on large branches and is characterized by an expanded light reflex with a yellowish tint. The symptom indicates sclerotic changes in the vessel with a predominance of elastic hypertrophy or plasmatic impregnation of the vascular wall with lipoid deposits. The silver wire symptom appears on arterioles of the second or third order: the vessel is narrow, pale, with a bright white axial reflex, often it seems completely empty. Retinal hemorrhages Hemorrhages in the retina during hypertension occur by diapedesis of red blood cells through the altered wall of microvessels, rupture of microaneurysms and small vessels under the influence of increased pressure or as a consequence of microthrombosis. Especially often, hemorrhages occur in the layer of nerve fibers near the optic disc. In such cases, they look like radially arranged strokes, stripes or flames (Fig. 9). In the macular zone, hemorrhages are located in the Genly layer and have a radial location. Much less often, hemorrhages are found in the outer and inner plexiform layers in the form of irregularly shaped spots. Retinal “exudates” Hypertension is especially characterized by the appearance of soft exudates resembling cotton wool. These grayish-white, loose-looking, anteriorly protruding lesions appear predominantly in the parapapillary and paramacular zones (Fig. 8, 9). They arise quickly, reach maximum development within a few days, but never merge with each other. During resorption, the focus gradually decreases in size, flattens and fragments. Cotton wool lesion is an infarction of a small area of nerve fibers caused by microvascular occlusion [8, 9]. As a result of the blockade, axoplasmic transport is disrupted, nerve fibers swell, and then fragment and disintegrate [10]. It should be noted that such lesions are not pathognomonic for hypertensive retinopathy and can be observed with congestive discs, diabetic retinopathy, CVS occlusion, and some other retinal lesions in which necrotic processes develop in the arterioles. Unlike cotton wool-shaped lesions, hard exudates in hypertension have no prognostic value. They can be dotted or larger, round or irregular in shape (Fig. 7, 8), located in the outer plexiform layer and consist of lipids, fibrin, cellular debris and macrophages. It is believed that these deposits arise as a result of the release of plasma from small vessels and subsequent degeneration of tissue elements. In the macular region, solid lesions have a banded shape and a radial arrangement, forming a complete or incomplete star figure (Fig. 8, 9). They have the same structure as other solid lesions. As the patient's condition improves, the star's figure may dissolve, but this process takes a long time - over several months or even several years. Swelling of the retina and optic disc Swelling of the retina and optic disc, combined with the appearance of soft lesions, indicates a severe course of hypertension (Fig. 7, 9). Edema is localized mainly in the peripapillary zone and along the course of large vessels. With a high content of proteins in the transudate, the retina loses transparency, becomes grayish-white and the vessels are covered in places with edematous tissue. Swelling of the optic disc can be expressed to varying degrees - from slight blurring of its contour to a picture of a developed stagnant disc. Congestive disk in hypertension is often combined with peripapillary retinal edema, retinal hemorrhages and cotton wool lesions (Fig. 9). Visual functions Decreased dark adaptation is one of the earliest functional signs in hypertensive retinopathy [5]. At the same time, there is a moderate narrowing of the isopter and the boundaries of the visual field, as well as an expansion of the “blind spot”. With severe retinopathy, scotomas localized in the paracentral region of the visual field can be detected. Visual acuity decreases much less frequently: with ischemic maculopathy, macular hemorrhages, with the occurrence of edematous maculopathy and with the formation of the epiretinal membrane in the late stage of neuroretinopathy. Classification of hypertensive changes in the fundus Currently, there is no generally accepted classification of hypertensive angioretinopathy. In Russia and neighboring countries (former republics of the USSR), the most popular classification is M.L. Krasnov and its modifications. M.L. Krasnov [4] identified three stages of fundus changes in hypertension: 1. hypertensive angiopathy, characterized only by functional changes in the retinal vessels; 2. hypertensive angiosclerosis; 3. hypertensive retino- and neuroretinopathy, which affects not only the vessels, but also the retinal tissue, and often the optic disc. The author divided retinopathy into 3 subgroups: sclerotic, renal and malignant. The most severe changes in the retina are observed in renal and especially malignant forms of headache (Fig. 9). The stages of hypertension and the prognosis for the patient’s life are determined by the height of blood pressure and the severity of vascular changes in the kidneys, heart and brain. These changes are not always parallel with retinal lesions, but there is still a certain relationship between them. Therefore, multiple hemorrhages in the retina, the appearance of areas of ischemia, non-perfused zones, cotton-wool exudates, as well as pronounced swelling of the optic disc and peripapillary retina indicate the severe progressive nature of the disease and the need to change and intensify therapeutic measures. Treatment of hypertensive neuroretinopathy Therapy of hypertensive (neuro)retinopathy consists of treating the underlying disease. To reduce retinal ischemia, vasodilators are used, which dilate mainly the vessels of the brain and eye (Trental, Cavinton, Xavin, Stugeron). Oxygen inhalation is often used to reduce hypoxia. However, oxygen can cause retinal vasoconstriction [6]. Therefore, we prefer to prescribe carbogen inhalations, which in addition to oxygen contains carbon dioxide (5–8%). Carbon dioxide has a strong vasodilatory effect on the vessels of the brain and eyes. To improve blood rheology and prevent the occurrence of thrombosis, antiplatelet agents are used. It should be taken into account that elimination of retinal ischemia can lead to the development of post-ischemic reperfusion syndrome, which consists of excessive activation of free radical processes and lipid peroxidation. Therefore, constant intake of antioxidants (alpha-tocopherol, ascorbic acid, veton, diquertin) is essential. The use of angioprotectors, especially doxium, is useful. Preparations containing proteolytic enzymes (Wobenzym, papain, recombinant prourokinase) are used to resolve intraocular hemorrhages. For the treatment of retinopathy of various origins, transpupillary irradiation of the retina using a low-energy infrared diode laser is prescribed.
Literature 1. Vilenkina A.Ya. // Collection of materials from NIIGB im. Helmholtz. – M., 1954. – P. 114–117. 2. Katsnelson L.A., Forofonova T.I., Bunin A.Ya. // Vascular diseases of the eye. – M. 1990. 3. Komarov F.I., Nesterov A.P., Margolis M.G., Brovkina A.F. // Pathology of the organ of vision in common diseases. – M. 1982. 4. Krasnov M.L. // Vestn. ophthalmol. – 1948. – No. 4., pp. 3–8. 5. Rokitskaya L.V. // Vestn. ophthalmol. – 1957. – No. 2. – P. 30–36. 6. Sidorenko E.I., Pryakhina N.P., Todrina Zh.M. // Physiology and pathology of intraocular pressure. – M. 1980. – P. 136–138. 7. Shershevskaya O.I. // Eye damage in some cardiovascular diseases. – M. 1964. 8. Harry J., Ashton N. // Trans. Ophthalmol. Soc. UK. – 1963. – V. 83. – P. 71–80. 9. McLeod D. // Brit. J. Ophthalmol. – 1976. – V. – 60. – 551–556. 10. Walsh JB // Ophthalmology. – 1982. – V. – 89. – P. 1127–1131.
Diagnostics1,2
Anamnesis
If GAR is suspected, the ophthalmologist must carefully collect an anamnesis - your medical history. Particular attention should be paid to hypertension and your family members with this disease. This is a simple survey, during which it is better not to hide anything: this will help the doctor make the correct diagnosis.
Ophthalmoscopy
An ophthalmoscope shines light through the pupil to check the back of the eye for changes in the retina, including narrowing of blood vessels. The doctor will also check if fluid is leaking from your blood vessels as indicated. This is a painless procedure that will take no more than 10 minutes.
Fluorescein angiography
First, you are given special eye drops to dilate your pupils. Fluorescein dye will then be injected into your vein. Next, pictures are taken while the dye circulates through the eyes. Fluorescein may leak into the retina or stain altered blood vessels if there is an abnormality.
Complications
People with hypertensive retinopathy are at risk of developing retinal complications. These include the following2,3:
- Ischemic optic neuropathy occurs when high blood pressure interferes with normal blood flow in the eyes, causing damage to the optic nerve. As a result, the brain cannot form an image normally.
- Retinal artery occlusion occurs when the arteries that carry blood to the retina become blocked by blood clots. When this happens, the retina does not have enough oxygen or blood. This leads to loss of vision.
- Malignant hypertension is a rare disease that causes a sudden increase in blood pressure, affecting vision and causing sudden loss of vision. This is a potentially life-threatening condition.
Patients with GAD are also at increased risk of stroke or heart attack. One study found that people with GAD are more likely to have a stroke than people without the condition.
Treatment
Effective treatment includes reducing high blood pressure with medications and lifestyle changes.
To keep your blood pressure under control, you need4:
- Exercise regularly
- Avoid coffee and alcohol
- Reduce the amount of salt in your diet
- Lose weight if you are overweight
Your doctor may also prescribe blood pressure medications: diuretics, beta blockers, or ACE inhibitors.
Bibliography:
- Kiseleva T. N., Ezhov M. V. et al. Retinal circulation disturbances in arterial hypertension. Pharmateka. 2014; 20: 14-18.
- Moshetova L., Vorobyova I. et al. Hypertensive angioretinopathy: clinical and morphological manifestations, diagnosis. Doctor. 2018; 3: 82-84.
- Zadionchenko V. S., Adasheva T. V. et al. The eye is a mirror of cardiovascular pathology. Evolution of ideas about hypertensive retinopathy. Rational pharmacotherapy in cardiology. 2010; 6 (6): 853-858.
- Arterial hypertension in adults. Clinical recommendations. Approval year 2021.
THE INFORMATION PROVIDED ON THE SITE DOES NOT CONSTITUTE AND DOES NOT REPLACE PROFESSIONAL ADVICE
Treatment of hypertensive retinal angiopathy in Moscow
Effective treatment of angiopathy associated with hypertension is impossible without correction of high blood pressure. Every patient with hypertension should have their blood pressure measured twice daily (i.e., morning and evening); This data will allow you to select the optimal dosage of drugs, allowing you to avoid strong surges in pressure throughout the day and maintain performance.
You need to adjust your daily routine, avoid overwork and stressful situations, and spend more time outdoors. In addition, with hypertensive retinal angiopathy, prolonged work at the computer, as well as other eye strain, is contraindicated.
The following medications are used to treat hypertensive retinal angiopathy:
- dilating vessels;
- preventing the formation of blood clots;
- protecting the vascular wall;
- antioxidants;
- for resorption of exudates in the retinal area.
Services for diagnosis and treatment of hypertensive retinal angiopathy in Moscow are provided by our Okomed clinic. The best ophthalmologists will check the condition of your eyes and, based on the diagnostic data obtained, will provide effective treatment for the disease.