With fat embolism (FE), embolization of the microvasculature occurs with fat droplets. First of all, the capillaries of the lungs and brain are involved in the pathological process. Which is manifested by the development of acute respiratory failure, hypoxemia, ARDS of varying severity, diffuse brain damage. Clinical manifestations usually develop 24 to 72 hours after injury or other exposure.
- Common causes of PVCs
- Rare causes of PVCs
- Diagnosis of PVCs
- Main manifestations of fat embolism
- Treatment
- Prevention of fat embolism
In typical cases, the clinical manifestations of PVCs develop gradually, reaching their maximum approximately two days after the first clinical manifestations. The fulminant form is rare, but death can occur within a few hours of the onset of the disease. PVCs are more common in young patients, but mortality is higher in older patients.
There is an opinion that if the patient was in a state of deep alcoholic intoxication at the time of the injury, PVCs rarely develop. There are several theories on the mechanism of occurrence of fat embolism (mechanical, colloidal, biochemical), but, most likely, in each specific case different mechanisms leading to PVCs are implemented. Mortality, based on the number of diagnosed cases, is 10-20%.
Rare causes of PVCs
- Hip replacement;
- Intramedullary osteosynthesis of the femur with massive pins;
- Closed reduction of bone fractures;
- Extensive surgical interventions on tubular bones;
- Extensive soft tissue injury;
- Severe burns;
- Liposuction;
- Bone marrow biopsy;
- Fatty liver degeneration;
- Long-term therapy with corticosteroids;
- Acute pancreatitis;
- Osteomyelitis;
- Introduction of fat emulsions.
Diagnosis of PVCs
Symptoms of fat embolism:
- Patients may complain of vague chest pain, lack of air, and headache.
- There is an increase in temperature, often above 38.3º C. Fever in most cases is accompanied by a disproportionately high tachycardia.
- Most patients with PVCs are drowsy and have oliguria.
If patients, 1-3 days after a skeletal injury, have increased body temperature, drowsiness and oliguria, then the presence of PVCs should first be assumed.
Folk remedies
Photo: narodnymi.com
Fat embolism always occurs as a consequence of injury or severe somatic illness. Under no circumstances should you self-medicate, but should go to a medical institution where specialized medical care will be provided. In its absence, the probability of death is high.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Main manifestations of fat embolism
- Arterial hypoxemia (PaO2 <60-70 mm Hg, SpO2 <90-92%);
- Signs of ARDS (usually with severe PVCs);
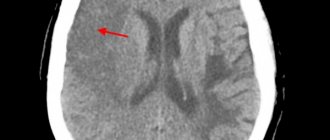
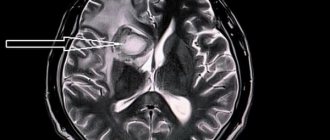
- Dysfunction of the central nervous system (motor restlessness, convulsions, delirium, coma). It is characteristic that after normalization of oxygenation, there is no noticeable regression of neurological symptoms;
- Petechial rashes develop 24-36 hours after injury in 30-60% of patients with PVCs. They are localized in the upper half of the body, more often in the axillary region. Hemorrhages on the oral mucosa, eye membranes and conjunctiva are also characteristic. The rash usually disappears within 24 hours;
- Sudden decrease in hemoglobin on days 2-3;
- Thrombocytopenia, or rapid decrease in platelet count, decrease in fibrinogen levels;
- Detection of neutral fat in blood, urine, cerebrospinal fluid, sputum (fat is detected in alveolar macrophages);
- Detection of fat during skin biopsy in the area of petechiae;
- Detection of retinal fatty angiopathy.
Sources
- Kuzmichev D. E., Skrebov R. V., Viltsev I. M., Chirkov S. V. Fat embolism. 2014. Problems of expertise in medicine;
- Yakovlev V.N., Marchenkov Yuri Viktorovich, Panova N.S., Alekseev V.G., Moroz V.V. Fat embolism. 2013. General resuscitation;
- Gabdullin M. M., Mitrakova N. N., Gatiatulin R. G., Rozhentsov A. A., Koptina A. V., et al. Fat embolism syndrome. 2012. Modern technologies in medicine;
- Litvinenko Stanislav Grigorievich, Ladeishchikov V. M., Popov A. V. Laboratory diagnosis of fat embolism. 2012. Clinical laboratory diagnostics;
- Yakovlev Alexey Yurievich, Pevnev A.A., Nikolsky V.O., Galanina T.A., Prokin E.G., et al. Metabolic prevention of fat embolism. 2021. Anesthesiology and resuscitation;
- Danilova E.V. Fat embolism syndrome. 2015. Forensic medicine.
Video from YouTube on the topic of the article:
Treatment
Many therapies that have been proposed for the treatment of PVC have been ineffective: glucose administration to reduce the mobilization of free fatty acids, ethanol administration to reduce lipolysis. Severe injuries are often accompanied by the development of coagulopathy. In the first few days (usually within three days), the administration of heparin (including low molecular weight heparins) increases the risk of bleeding, increases the concentration of fatty acids in plasma, and, in most cases, is not indicated.
There is no evidence that commonly prescribed drugs for the treatment of PVCs, such as Essentiale, lipostabil, nicotinic acid, hepasol, contrical, sodium hypochlorite, can improve treatment outcomes. So treatment is mainly symptomatic.
Maintaining PaO2 > 70-80 mm Hg. Art., SpO2 ≥ 90 ≤ 98% – the goal of respiratory therapy. In mild cases, oxygen therapy through nasal catheters is sufficient. The development of ARDS in patients requires special approaches and mechanical ventilation regimens.
Reasonable limitation of the volume of infusion therapy and the use of diuretics can reduce the accumulation of fluid in the lungs and help reduce ICP. Until the patient's condition stabilizes, saline solutions (0.9% sodium chloride, Ringer's solution) and albumin solutions are used. Albumin not only effectively restores intravascular volume and slightly reduces ICP, but also by binding fatty acids may be able to reduce the progression of ARDS.
For severe cerebral manifestations of PVCs, sedative therapy and artificial ventilation are used. There is a certain correlation between the depth of the coma and the degree of increase in ICP. The management of these patients is in many ways similar to the management of patients with traumatic brain injury of another origin. It is necessary to prevent body temperature from rising above 37.5°C, for which non-steroidal analgesics are used, and, if necessary, physical cooling methods.
Broad-spectrum antibiotics are prescribed, usually 3rd generation cephalosporins, as initial therapy. If clinically significant coagulopathy develops, the use of fresh frozen plasma is indicated.
The effectiveness of corticosteroids in the treatment of PVCs has not been proven. But they are often prescribed in the hope that they will be able to prevent further progression of the process. For PVCs, corticosteroids are recommended in high doses. Methylprednisolone 10-30 mg/kg bolus over 20-30 minutes. Then 5 mg/kg/hour by dispenser for 2 days. If methylprednisolone is not available, other corticosteroids (dexamethasone, prednisolone) are used in equivalent dosages.
Prevention of fat embolism
Prevention of PVCs is indicated for patients with fractures of two or more long tubular bones of the lower extremities and fractures of the pelvic bones. Preventive measures include:
- Effective and early elimination of hypovolemia and blood loss;
- Adequate pain relief;
- Early, in the first 24 hours, surgical stabilization of fractures of the pelvis and large tubular bones is the most effective preventive measure.
The frequency of complications in the form of PVCs and ARDS increased significantly (4-5 times) if surgical intervention was postponed to a later time. Note that chest trauma and traumatic brain injury are not a contraindication to early intramedullary osteosynthesis of long bones. The effectiveness of corticosteroids for the prevention of PVCs and post-traumatic hypoxemia has been proven, although the optimal regimens and doses of drugs have not been established. Methylprednisolone is used more often - 15-30 mg/kg/day. within 1-3 days. But there is data confirming the effectiveness of lower doses: methylprednisolone at a dose of 1 mg/kg every 8 hours for 2 days. Corticosteroids are especially indicated if early fracture stabilization has not been achieved.
Description
Fat embolism is an extremely dangerous condition in which particles of adipose tissue enter the body’s circulatory system, causing life-threatening and health-threatening complications.
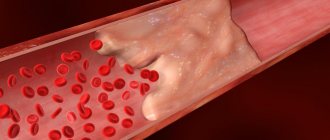
Fat embolism develops most often with injuries to the extremities, including during surgical interventions, when long tubular bones are fractured. Also, a similar condition can develop with multiple pelvic fractures. The sharp edges of the bone fragment damage the vessels lying next to the bone, and the fatty components of the yellow bone marrow enter the vascular bed from the medullary canal. A similar condition, which is called fat embolism syndrome, can occur in conditions such as sepsis, acute pancreatitis, shock of various origins, prolonged compression syndrome, crush injuries of subcutaneous fat, sickle cell anemia and diabetes mellitus. Entering the circulatory system, fat particles in the form of small bubbles that can connect and increase in size enter the vessels of the lungs. In the lungs, fat emboli clog a vessel, depriving one or more areas of the lung of blood supply. Because of this, it is often difficult to immediately make a correct diagnosis, because the symptoms of fat embolism are similar to pulmonary embolism or pneumonia. There are two stages in the development of fat embolism syndrome.
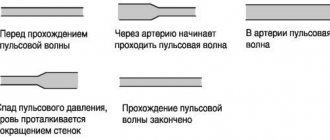
The first is the mechanical stage. Fat from yellow bone marrow or damaged loose subcutaneous fat enters the vascular bed due to a local increase in pressure. In normal condition, the pressure of the bone marrow canal does not exceed 50 millimeters of mercury. Against the background of the general serious condition of the patient, the pressure inside the bone can increase from 50 to 100 millimeters of mercury. Because of this, fat droplets (globules) exit through the capillaries that feed the bone into the bloodstream. The body responds to the appearance of fat emboli in the blood with the active production of fat-dissolving enzymes, the active release of fat from fat depots and the development of an inflammatory reaction in places where the emboli have entered the bloodstream. It has been proven that fat emboli can be detected in the pulmonary capillaries within a few seconds, after injury or surgical manipulation in the bone marrow canal.
The second stage is called biochemical. Leading pathological processes occur in the lungs, since they are a kind of blood filter. Large fatty particles, 10 micrometers or more in size, are not able to pass through the capillaries. Therefore, they remain in the lungs, clogging blood vessels and thus reducing blood flow in certain areas. Smaller emboli pass through the lungs and enter the systemic circulation. Under the influence of enzymes, fat drops are converted into fatty acids, which have a destructive effect on the inner lining of blood vessels. This causes intravascular inflammation, which causes the accumulation of various substances in the blood that negatively affect the general condition of the patient.
The amount of proteins and phosphate compounds in the blood and their functional state affects the fat droplets circulating in the blood. When the metabolism of phosphates and proteins is disrupted, the surface tension of fat emboli changes, which leads to their fusion into larger particles. Because of this, active formation of microthrombi occurs in the blood, intravascular coagulation develops, severe intoxication syndrome develops, and the membranes of the cells that make up the walls of blood vessels are damaged. However, if the described mechanisms of damage have not started, then the presence of small fat droplets in the bloodstream may not appear in any way.
After passing through the pulmonary circulation (pulmonary vessels), small fat drops are able to merge into larger drops and affect not only the lungs, but also other organs with a wide network of microcapillaries. This may also be due to the ability of fat droplets to change their shape - to stretch and deform to the shape of the vessel. The target organs that will be primarily affected by fat embolism syndrome include the brain, retina, kidneys, and skin.
Fat embolism is divided into the following forms:
- Fulminant, which leads to death within a few minutes after fatty elements enter the bloodstream;
- Spicy. With this form of fat embolism, clinical manifestations develop several hours after injury;
- Subacute, with a period of clinical well-being from 12 to 72 hours.
Fat embolism may develop 14 or more days after injury. Most likely, such cases are associated with violation of the rules of immobilization (immobility) of the injured limb.