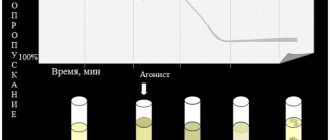
Increased aggregation is a marker of hyperaggregation syndrome and thrombophilia. The most commonly used are the Born turbidimetric method, based on recording changes in the light transmission of platelet-rich plasma, and the method for studying platelet aggregation, based on the analysis of light transmission fluctuations caused by a random change in the number of particles in the optical channel.
Material for research.
Citrate platelet rich plasma
Research method
is determined by the operating procedure on a particular type of aggregometer.
Solutions of ADP, ristocetin, collagen, adrenaline, and arachidonic acid are most often used as inducers. Solutions of thrombin, serotonin, etc. can also be used.
Platelet aggregation with ADP
Exposure to small doses of ADP (usually 1*10-7 mol) leads to the formation of a double wave of aggregation. The first phase (primary wave) depends on added exogenous ADP, and the second phase (secondary aggregation wave) occurs due to the release reaction of intrinsic agonists contained in platelet granules. Large doses of ADP (usually 1*10-5 mol) lead to the merging of the first and second waves of aggregation.
When analyzing aggregograms, attention is paid to the general nature of aggregation (single-wave, two-wave; complete, incomplete; reversible, irreversible) and the rate of aggregation. The appearance of two-wave aggregation upon stimulation of ADP at concentrations that normally cause reversible aggregation (usually 1-5 µmol) indicates an increase in platelet sensitivity, and the development of single-wave incomplete (and often reversible) aggregation upon stimulation of ADP at concentrations of 10 µmol or more indicates an increase in platelet sensitivity. impaired platelet release reaction.
Treatment
Acquired thrombocytopathies can be treated with medication. Therapy is based on the use of hemostatic drugs to reduce bleeding, hemostatic herbs, and metabolic agents. Prevention of exacerbations is carried out at least 2 times in 12 months.
The list of drugs for the treatment of hemorrhagic diathesis includes:
- Calcium gluconate;
- Aminocaproic acid;
- ATP;
- Folic acid;
- Sodium etamsylate, etc.
Stopping bleeding in cases of coagulation disorders can be done by topical application of aminocaproic acid. Bleeding from the nasal cavity is well stopped with the help of special sponges on which hemostatic substances are applied.
Therapy for aggregation disorders should not be purely symptomatic. For a complete recovery of the patient, first of all, it is necessary to cope with the underlying disease that led to the appearance of the pathology.
Also, to maintain the optimal fluid composition of the blood, it is important to drink at least 2 - 2.5 liters of water per day. This will prevent vasoconstriction and blood thickening, thereby improving blood circulation.
Platelet aggregation with ristocetin
Determination of platelet aggregation with ristocetin in plasma is used to quantify von Willebrand factor. The method is based on the ability of ristocetin to stimulate in vitro the interaction of von Willebrand factor with platelet glycoprotein Ib. In most cases of von Willebrand disease, there is a violation of ristocetin aggregation with a normal response to the effects of ADP, collagen and adrenaline. Disturbances in ristocetin aggregation are also detected in Bernard-Soulier disease. For differentiation, a test with the addition of normal plasma is used: in von Willebrand disease, after the addition of normal plasma, ristocetin aggregation is normalized, while in Bernard-Soulier syndrome this does not happen. Ristocetin-induced platelet agglutination is reduced in most cases of von Willebrand disease, except type IIB.
References
- Clinical laboratory diagnostics, National guidelines, Volume 1, Dolgov V.V., Menshikov V.V., 2012, pp. 761-765
- Kozlovsky V. I., Kovtun O. M., Seroukhova O. P., Detkovskaya I. N., Kozlovsky I. V. Research methods and clinical significance of platelet aggregation. Focus on spontaneous aggregation // Vestnik VSMU. 2013. No. 4.
- Puri RN, Colman RW.ADP-induced platelet activation.Crit Rev BiochemMol Biol. 1997;32(6):437-502. doi: 10.3109/10409239709082000. PMID: 9444477.
- Murugappa S, Kunapuli SP. The role of ADP receptors in platelet function.FrontBiosci. 2006 May 1;11:1977-86. doi:10.2741/1939. PMID: 16368572.
- Barbara Lunghi, Anna Lecchi, Rosa Santacroce, Mariangela Scavone, Rita Paniccia, Andrea Artoni, Christian Gachet, Giancarlo Castaman, Maurizio Margaglione, Francesco Bernardi, Marco Cattaneo. Severe bleeding and absent ADP-induced platelet aggregation associated with inherited combined CalDAG-GEFI and P2Y12 deficiencies.Haematologica 2020;105(7):e361-e364
Platelet aggregation with collagen
Platelet aggregation with collagen has a fairly pronounced latent phase, during which phospholipase C is activated. Depending on the concentration of the reagent used, the duration of this phase can be 5-7 minutes. After the end of this period, processes occur in platelets that lead to the formation of second messengers, as a result of which the secretion of platelet granules and the synthesis of thromboxane A2 develop, which is accompanied by a sharp increase in interplatelet interaction.
In laboratory and clinical practice, collagen is most often used in a final concentration of 50 μg/ml, however, collagens from different companies may have different activities, which must be taken into account when using them.
Features of clotting in children
In recent years, the phenomenon of hyperaggregation has been observed not only in adults, but also in children. In a child, the causes of this pathology can be hereditary or acquired.
The main reasons for increased platelet activity in children:
- blood diseases;
- viruses and infectious agents;
- surgical interventions.
Children in the first year of life may have hyperaggregation due to dehydration or anemia.
In adolescents, the same phenomenon is provoked by stress and age-related changes.
The main manifestation of hypoaggregation in children is an increase in nosebleeds, the causeless appearance of bruises and hemorrhages.
In teenage girls, this can be caused by heavy bleeding during menstruation.
To prescribe treatment, it is important to determine the pathology that caused the symptoms. In some cases, a simple correction of the diet will suffice.
In others, only high-quality drug treatment will be needed. The latter is prescribed by a hematologist, taking into account age characteristics and severity of the disease.
Platelet aggregation with adrenaline
Adrenaline, upon contact with platelets, interacts with α2-adrenergic receptors, which causes inhibition of adenylate cyclase. It is possible that the mechanism underlying the implementation of the effect of adrenaline and the development of the first wave of aggregation does not depend on the formation of thromboxane A2, the release reaction or the synthesis of platelet aggregation factor, but is associated with the ability of adrenaline to directly change the permeability of the cell membrane to calcium ions. The second wave of aggregation occurs as a result of the release reaction and production of thromboxane A2.
Indications for analysis
Platelet aggregation is studied when:
- hemorrhagic disorders (increased bleeding);
- thrombophilia (coagulation disorder with an increased risk of thrombosis);
- severe atherosclerosis;
- diabetes mellitus;
- before performing surgical interventions;
- during pregnancy;
- when monitoring the effectiveness of anticoagulant and antiplatelet therapy.
Also, this study is important in the diagnosis of hereditary hemorrhagic thrombocytopathies.
Platelet aggregation with arachidonic acid
Arachidonic acid is a natural aggregation agonist, and its action is mediated by the effects of prostaglandins G2 and H2, thromboxane A2, and includes activation of both phospholipase C with subsequent formation of second messengers, mobilization of intracellular calcium and expansion of the cell activation process, and phospholipase A2, which directly leads to release of endogenous arachidonic acid. Platelet aggregation with arachidonic acid occurs quite quickly, so the curve characterizing this process is often single-wave in nature.
To induce aggregation of blood platelets, arachidonic acid is used in concentrations of 10-3-10-4 mol. When working with arachidonic acid, it should be taken into account that in air this substance oxidizes very quickly.
An aggregation test with arachidonic acid is recommended in cases of using drugs that affect the aggregation reaction (for example, acetylsalicylic acid, penicillin, indomethacin, delagil, diuretics), which must be taken into account when assessing the research results.
What is the blood coagulation system?
The blood coagulation system is part of the general hemostasis system, which is responsible for maintaining blood in a normal liquid state and preventing blood loss.
The hemostatic system includes the coagulation and anticoagulation systems, the balance between which ensures the normal functioning of the circulatory system.
When bleeding occurs, coagulation processes begin to work more efficiently; when the blood becomes too thick, anticoagulation processes begin to work.
In order for the blood to clot in case of bleeding, the interaction of the following components is necessary:
- walls of blood vessels;
- platelets and other blood cells;
- plasma enzymes and other substances.
Causes of hypoaggregation
Among the culprit factors are the following options.
Thrombocytopathy
Develops as a primary or secondary pathological process. Accompanied by a decrease in the functionality of formed cells. This is a rather complex disease from a therapeutic point of view.
Treatment. Loading doses of glucocorticoids are prescribed. This often has its effects. Drugs such as Prednisolone and Dexamethasone are indicated as first-line drugs.
They are used in short courses so as not to provoke deterioration or side effects. Condition monitoring is required. Regular screening is indicated. For these purposes, repeat blood tests are prescribed every week. Plus or minus.
Thrombocytopenia
It occurs against the background of genetic, hereditary changes. The pathological process is difficult to treat. In the initial phase of therapy, glucocorticoids are prescribed.
In half of the clinical cases, stable remission can be achieved by removing the spleen.
Atrombia
In this pathological process, the functions of the membrane receptor for special coagulation factors are lost. The result is the inability of the formed cell to respond to an external stimulus. Accordingly, the disorder is difficult to correct. This is a hereditary anomaly.
Treatment. Special preparations. Glucocorticoids are usually prescribed. Vitamin and mineral complexes also play a large role. But only as support, not primary therapy.
Thrombasthenia
In general, the process is similar to the previous one. There is a disorder of the membrane receptor and its functioning. Often it is absent altogether, therefore it does not respond to fibrinogen.
Violations are observed even at the adhesion stage, the disorder is severe. Dangerous bleeding occurs.
The treatment is identical. Plus, hemostatic medications are used.
Hereditary pathological processes
For example, von Willebrand disease, Bernard-Soulier, Wiskott-Aldrich. They differ in clinical course. In the first case, the ability to adhere is lost, in the second and third, the normal shape and structure of platelets is disrupted, which becomes a problem and causes hypoaggregation.
Effective treatment is not possible. Hemostatic drugs are prescribed. In the case of these diseases, a careful lifestyle is indicated. Less physical activity so as not to provoke injuries, damage and bleeding.
Diabetes mellitus and endocrine diseases
They cause clotting disorders because the entire hormonal balance is affected. Therapy depends on the specific diagnosis.
Sepsis
Acute generalized pathological process. Accompanied by tissue inflammation. Treatment involves the use of loading doses of antibiotics.
If an increase in the indicator promises thrombosis, then a decrease in platelet aggregation is fraught with bleeding. This is no less dangerous phenomenon.
Additional examinations
Activities help make the correct diagnosis. Among the possible options:
- Oral interview with a hematologist. Outside doctors are hired as needed.
- Collecting a life history. Habits, congenital and acquired disorders and other important points.
- Ultrasound of the digestive tract.
- Plain radiography of the chest.
- Genetic consultation.
- Blood tests: general, biochemical, hormones and coagulogram. To track all possible deviations.
- Advanced glucose tolerance test. Sugar curve. Helps detect diabetes.
- Blood pressure measurement. This includes 24-hour monitoring.
Aggregation is the process of platelets gathering to further close the resulting wound. This is an important physiological phenomenon. A special analysis helps to identify all possible abnormalities and begin timely treatment.
What role does this process play in the body?
Aggregation is not the only stage in stopping hemorrhage. This is only one component of hemostasis - a complex of physiological mechanisms that maintain the fluid state of the blood and minimize its loss when the vascular bed is damaged.
It is divided into 2 types:
- Vascular-platelet – stops hemorrhages from small vessels. For this, a microcirculatory hemostatic mechanism is sufficient.
- Coagulation – stops hemorrhages from large vessels. This requires activation of the clotting factor.
Hemostasis can be complete only if both designated mechanisms function normally and interact with each other. Then, when a vessel is damaged, a whole chain of reactions is activated, which will lead to the formation of a blood clot and blockage of the bleeding site.
It will be headed by vascular spasm. It will ensure a decrease in systolic pressure in the affected bloodstream, which will slow down blood loss.
Then the endothelial cells lining the walls of the vessel from the inside will be involved in the process. They will begin to produce anticoagulants, which will prevent the uncontrolled growth of a blood clot, and procoagulants, which will activate platelets and increase their adhesive properties. From this moment the formation of a traffic jam will begin.
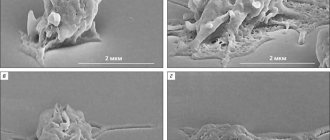
Platelets will rush to the wound surface - their adhesion (adhesion to the vessel wall) and agglutination (sticking together) will begin.
At the same time, blood cells will produce:
- active substances that will increase spasm of the vessel walls, which will lead to a decrease in the speed of blood flow;
- platelet factors that will trigger the coagulation mechanism;
- thromboxane A2 and the nucleotide adenosine diphosphate (ADP) are adhesion stimulators.
The thrombus, consisting of sticky plates, will begin to grow. The platelets will continue to aggregate until the clot closes the gap in the vessel.
The resulting plug is characterized by reduced permeability to blood plasma, but is not reliable. Fibrin, an insoluble protein, will help strengthen it. Its threads will entwine platelets, compacting the glued mass - a full-fledged blood clot will form.
At the same time, the blood platelets will release the thrombostenin factor, which will tightly fix the plug. It will block the lumen in the vessel and prevent blood loss.
The destruction of the formed thrombus will be ensured by the fibrinolysis system, the main role of which is the dissolution of fibrin threads. It will also prevent excessive platelet aggregation and the formation of pathological plugs in entire vessels.
Causes of hyperaggregation
When talking about factors, there is one important point to keep in mind. All the diagnoses listed below are also possible examination findings. The previous list is incomplete.
Hyperaggregation is a condition in which the rate of platelet crowding is increased. Why is this happening.
Hypercoagulability syndrome
Considered to be a congenital anomaly. Accompanied by an overreaction to intrinsic coagulation factors. The violation is clearly visible from the results of the collagen test.
Treatment is carried out under the supervision of a hematologist. Antiplatelet agents of the acetylsalicylic acid group are prescribed. Short course.
If the disorder is persistent, safer drugs are used. For example, Ticlopidine, Clopidogrel long-term regimen.
The issue is complex and is decided by a doctor.
Reduced sensitivity to Aspirin
And derivatives of acetylsalicylic acid. It occurs quite rarely, the patient does not notice the problem. The change is detected when treated with drugs based on this substance.
As a rule, resistance is secondary and occurs against the background of other diseases. Be it viscous platelet syndrome or other conditions.
Treatment. Treated with antiplatelet agents. Non-aspirin drugs are prescribed.
Congenital disorders
Hereditary disorders. For example, some forms of thrombocytopathy. These conditions are difficult to treat. Complex therapy is required. The selection is carried out in the hospital.
As a rule, patients cannot fully recover because of a genetic disorder. That is, a violation in the very foundation of the body.
Drug treatment
Drugs of several groups. Non-steroidal anti-inflammatory drugs, antibiotics, hormonal contraceptives, glucocorticoids, diuretics.
This is just a small part. Typically, changes in adhesion and aggregation are directly indicated in the annotation as side effects.
The treatment is simple. Consists of canceling the current therapy regimen. Prescribing other drugs. Those that will not so intensely affect the speed and quality of coagulation.
Platelet hyperaggregation is a dangerous pathological process, since there is a high probability of rapid clotting and the formation of special blood clots (thrombi).
They can clog blood vessels, cause necrosis or death from complications. There is no point in joking with pathological changes. You need to see a doctor.
Read more about the types of thrombosis, treatment methods and complications in this article.