Thrombocytopenia is a pathological condition of the body, which is characterized by a decrease in the number of platelets in the bloodstream and is accompanied by increased bleeding.
Scientists say that thrombocytopenia is quite common. On average, this is from 10 to 130 cases, out of 1000 blood tests. (https://nbuv.gov.ua/UJRN/simmed_2017_2_28).
Normally, a healthy person has 150-320*109/l platelets in the blood. Their main task is to respond to any damage to the integrity of the skin or mucous membranes. They go to the site of injury, are activated and begin to form small blood clots, which close the gap. But there are diseases that lead to a decrease in the number of these cells.
This can occur by causing pathological destruction of platelets, problems with the formation of new ones and increased use of existing cells.
Thrombocytopenia can occur as an independent disease or as a separate symptom of various diseases that affect the blood coagulation system.
Causes of thrombocytopenia
There are 3 main mechanisms for the development of thrombocytopenia: impaired platelet formation, their redistribution in the spleen, or accelerated consumption. Therefore, there can be many reasons for this disease. Most often, the development of thrombocytopenia is influenced by the following factors:
- Hereditary diseases
that provoke pathological bleeding: Bernard-Sourya syndrome, May-Hegglin, TAR; - Pathologies that prevent the creation of new platelets
: bone marrow disorders, oncology, leukemia, reaction to chemical and radioactive elements, alcohol consumption; - Diseases in which the body rapidly consumes platelets
: DIC syndrome, immune disorders; - Enlarged spleen
. The spleen is a depot for platelets. This is where they are stored. If the organ enlarges, it takes a significant amount of red blood cells from the bloodstream. Bone marrow will not be able to compensate for such a deficiency; - Autoimmune factors
. When the immune system is impaired, the body begins to independently destroy its own platelets. This can occur due to systemic lupus erythematosus, encephalomyelitis; - Taking certain medications
. The active ingredients in medications can destroy platelets and interfere with their production by the bone marrow. Long-term use of cytostatics always leads to a similar consequence.
Where to get a blood test for PDW
We have no doubt that you take your own health seriously and value the quality of life that is possible in the absence of disease. Blood tests are one of the good and useful habits, and you are a frequent visitor to the laboratory of your favorite medical clinic. It is recommended to undergo a check-up at least for the basic parameters of blood composition and quality at least twice a year.
If we talk directly about the study of the width of platelet distribution, this index is a mandatory part of the OAC for the platelet formula and is submitted to any medical center. clinic.
Perhaps there is no time to visit a doctor for no reason, solely for preventive purposes, so we offer a more convenient way: the tests will be carried out in one of the laboratories of medical clinics, but the collection of biomaterial will be carried out at your home in a calm environment for you or at a specified location .
- Sterile;
- Personnel of the highest category with medical education and work experience;
- Up to 50 research parameters;
- Free with bioniq BALANCE subscription
Information from the analysis is a priority principle for creating a personalized complex of micronutrients, vitamins needed specifically at the current moment.
Thrombocytopenia in cancer patients
Thrombocytopenia is a problem that is familiar to many cancer patients. It develops due to chemotherapy: due to the use of platinum drugs (carboplatin, cisplatin, oxaliplatin) and gemcitabine. Each drug has its own mechanism for the development of thrombocytopenia:
- Platinum preparations
. These are alkylating agents that affect stem cells. Because of this, the production of platelets, as well as leukocytes and red blood cells, is suppressed; - Cyclophosphamide
. Affects the formation of megakaryocytes, from which platelets are subsequently formed; - Bortezomib
. Disturbs the process of separation of platelets from megakaryocytes; - Some medications cause platelet death
.
Radiation therapy also causes thrombocytopenia: it impairs bone marrow function, leading to low red blood cell levels. Thrombocytopenia develops especially often after radiation therapy in the pelvic area.
The likelihood of developing thrombocytopenia is even higher when radiation and chemotherapy are administered simultaneously. Certain tumors can also contribute to the development of this disease: lymphoma and leukemia. In this case, cancer cells quickly attack the red bone marrow, replacing its tissue with pathological ones. Less commonly, thrombocytopenia develops with damage to the bones, mammary glands, prostate and spleen.
When the level of platelets in the blood of cancer patients decreases, doctors need to determine the exact causes of this phenomenon. It may be necessary to change the treatment regimen or replace medications. Due to thrombocytopenia, the patient’s well-being significantly worsens, and difficulties arise in the treatment of oncology. Among them:
- When platelets decrease to less than 100*109 per liter
, the risk of bleeding increases; - Less than 50*109 per liter
– surgical interventions are not possible due to the risk of bleeding; - Less than 10*109 per liter
– multiple spontaneous bleeding occurs.
Thrombocytopenia
Thrombocytopenia - what is it?
We will talk about a violation of hemostasis, more precisely, its platelet component, which is characterized by the fact that the number of platelets per unit volume of blood decreases.
Occurs:
- High bleeding from the skin and mucous membranes;
- Bruises and hemorrhagic rashes form;
- Bleeding.
In order to eliminate the problem, it is necessary to resort to drug therapy, splenectomy, and extracorporeal blood purification.
Why do pathologies appear?
All causes of pathologies are divided into two groups:
- Congenital;
- Purchased.
If the pathology is congenital, then it is part of hereditary syndromes, for example, Wiskot-Aldrich syndrome.
With the development of pathology in these cases, as a rule, qualitative changes in platelets also occur.
The causes of acquired pathology are quite diverse: lymphomas, sarcoidosis, portal hypertension, splenic tuberculosis, alcoholism, etc.
The most significant group includes pathologies caused by increased platelet destruction. Moreover, they develop both as a result of the mechanical destruction of platelets and the immune component.
- Alloimmune pathology is provoked by transfusion of blood of a different group;
- Transimmune pathology occurs due to the fact that maternal antibodies penetrate to the fetus through the placenta;
- Autoimmune pathology is a consequence of the production of antibodies to one’s own unchanged antigens;
- Heteroimmune pathology occurs due to the fact that antibodies act against foreign antigens that are fixed on the surface of platelets.
- Drug-induced pathology is a consequence of taking sedatives, antibacterial or sulfonamide drugs, and some others.
Note that a slight decrease in the number of platelets can be caused by vaccination or viral infections.
Pathologies that arise due to platelet deficiency develop when there is an insufficient number of stem cells, and thrombocytopenia occurs. This condition may be affected by:
- Aplastic anemia;
- Leukemia;
- Myelofibrosis;
- Presence of metastases in the bone marrow;
- Chemotherapy treatment, some other things.
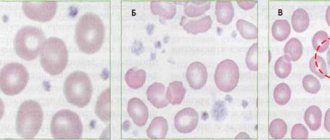
There are indicators of the severity of thrombocytopenia:
- First stage (satisfactory hemostasis). With it, the platelet count is 150-50x109/l;
- Second stage (sharp decrease in indicator - 50-20 x109/l). This may be the result of a minor injury that causes intradermal hemorrhages or prolonged bleeding from wounds;
- Stage three (platelet count is minimal – 20x109/l). Spontaneous internal bleeding is to be expected here.
Below we will talk about thrombocytopenia, which manifests itself moderately, sharply and severely.
Causes of moderate thrombocytopenia
- Excessive alcohol consumption;
- Pregnancy period;
- Liver pathologies;
- Use of a number of medications;
- DIC syndrome;
- Lupus erythematosus and systemic vasculitis;
- Heart failure;
- Consequences of radiation therapy.
Causes of severe thrombocytopenia
- Systemic lupus erythematosus;
- Significant DIC syndrome;
- Acute leukemia;
- Hemolytic disease of the newborn.
Causes of severe thrombocytopenia
- Acute radiation sickness;
- Overdose of cytotoxic drugs;
- Severe course of acute leukemia.
Symptoms
The manifestations of thrombocytopenia depend entirely on the underlying disease, but it is worth talking about the general signs. Among them:
- Bruises appear inexplicably on the skin;
- The blood slowly stops at the cut sites;
- Often the nose bleeds;
- The oral mucosa bleeds;
- Increased risk of internal bleeding;
- There is a risk of cerebral hemorrhage.
As soon as general symptoms appear, you should consult a doctor. Thrombocytopenia is treated in most cases on an outpatient basis.
Stenosis
If the pathology is severe, the patient must be placed in an intensive care unit. The treatment strategy itself is determined by the underlying disease.
Diagnostic measures
Any increased bleeding is a reason to visit a hematologist. The doctor will prescribe the necessary tests. Among which:
- General blood analysis;
- Hemostasiogram;
- Ultrasonography;
- Radiography;
- Enzyme immunoassay blood test.
The latest tests are indicated if necessary, this is already decided by the doctor.
Pathology in cancer
Thrombocytopenia is very common in cancer patients. This is not by chance, of course, chemotherapy and radiation therapy cause its appearance. Some drugs have a detrimental effect on platelets.
On the other hand, the pathology can be caused by some types of cancer, for example, lymphoma.
If a patient develops a pathology in which the platelet level drops, the doctor is obliged to consider all possible causes, even those not related to cancer treatment.
Thrombocytopenia makes the condition of an oncology patient complex, which means that the doctor faces difficulties in treating him. He must keep in mind that:
- If platelet counts are low, chemotherapy and radiation therapy must be carried out very carefully, as the risk of bleeding increases;
- A decrease in the rate of <50x109 per liter leads to an increased risk of heavy bleeding during surgery;
- A decrease <10x109 per liter significantly increases the risk of spontaneous bleeding.
Treatment of thrombocytopenia in cancer patients
There are recognized methods of treating pathology in cancer patients. They boil down to the following:
- It is necessary to adjust the therapeutic program;
- If necessary, transfuse platelet mass to the patient when there is a risk of bleeding or before a course of chemotherapy;
- It is necessary to transfuse platelet mass under the close supervision of a hemotransfusiologist and a nurse.
There are simple recommendations on how to avoid bleeding:
- Using an electric razor instead of a razor;
- Avoiding injury;
- Using a toothbrush with soft bristles;
- Rejection of drugs that reduce blood clotting, etc.
The Onco.Rehab Integrative Oncology Clinic is glad to see its patients who are not burdened by pathologies and their complications. We fight for your health, so that your days are filled with the joy of life.
Methods for diagnosing thrombocytopenia
At the initial stages, it is possible to diagnose thrombocytopenia only based on the results of a general blood test - based on a reduced level of platelets. But to identify possible causes of the pathology and its complications, the patient will have to undergo an extensive examination. Standardly it includes:
- Biochemical blood test – reflects the general condition of the body;
- Genetic blood test - identifies hereditary diseases that can cause thrombocytopenia;
- Duke bleeding time assessment – determines the state of the circulatory system;
- Determination of blood clotting rate;
- Bone marrow puncture - evaluates the composition and structure of red cells;
- Immunological blood test - detects antibodies to platelets IgG;
- Ultrasound of the liver and spleen determines the size of these organs.
Basic functions of platelets
In appearance, platelets are round or oval red plates with a smooth surface. They are formed in the bone marrow. They mature in approximately 8 days. These components constantly circulate in the bloodstream.
The main function of platelets is to ensure blood clotting. In addition, the ability of these blood components to stop bleeding is important. This is ensured by the fact that individual platelets can stick together and stick to sites of vascular damage. The process is automatically started by the human body when there is a risk of bleeding.
An important question is how long platelets live. Their viability time lasts approximately 10 days. Depending on the age of the red plates, their size changes: from 2 to 5 microns in diameter.
The process of platelet renewal in the blood occurs constantly. Therefore, an important factor to ensure the maintenance of blood condition is the balance between the formation of red plates and their death. Otherwise, there may be a tendency to blood clots or increased bleeding.
Treatment of thrombocytopenia
Thrombocytopenia is treated by a hematologist. The treatment regimen is developed individually for each patient: the patient’s age, the presence of any diseases, the degree of deficiency, and the amount of bleeding are taken into account. It is necessary to determine the cause of thrombocytopenia so that treatment is as effective as possible. Standard drug therapy consists of:
- Corticosteroids – have anti-inflammatory and analgesic effects;
- Immunoglobulins – correct the functioning of the immune system;
- Immunosuppressants – stop the destructive effect of the immune system on the body;
- Agonists to thrombopoietin receptors – promote more active production of this hormone.
In case of thrombocytopenia caused by bleeding, it is necessary to identify the source of this bleeding and stop it. Only after this the platelet correction is carried out. The patient will have to take medicinal iron and drugs that promote the production of red blood cells.
If drug treatment does not produce any results, splenectomy is indicated - surgical excision of the spleen. For hereditary diseases that prevent the body from producing enough platelets, a bone marrow transplant is necessary. If the platelet level is critically low, a blood transfusion of platelet mass from a donor is performed. If a large volume of blood is lost, a transfusion of fresh frozen plasma and red blood cells is necessary.
Prognosis and prevention
Thrombocytopenia is a dangerous disease that poses a huge threat to the life and health of the patient. Anemia often develops, and vision loss can occur due to hemorrhages in the retina. Advanced forms can provoke hemorrhages in the internal organs and in the brain. In most cases this leads to death.
Thrombocytopenia has no specific prevention. Experts give the following recommendations:
- Take a general blood test every year and undergo a general medical examination;
- Eat properly and nutritiously: eat as much meat and fresh vegetables as possible;
- Play sports and lead an active lifestyle;
- Avoid self-medication: taking aspirin and steroid drugs should be under the strict supervision of a doctor;
- Try to avoid any procedures where there is a risk of cutting (shaving, manicure);
- Treat any infectious processes in a timely manner;
- Take precautions when working with chemicals;
- Give up bad habits: drinking alcohol slows down platelet production.
Thrombocytopenia is a disease that requires constant medical supervision. If you suspect you have it or know about the pathology and want to get rid of it, contact the Medscan medical center. Experienced doctors will perform the necessary diagnostics and develop an individual treatment plan.
Symptoms of thrombocytope
All symptoms of thrombocytopenia are associated with bleeding and manifest themselves as follows:
- Frequent nosebleeds that occur without good reason. This can be a simple runny nose, sneezing, blowing out the nose, or during gentle touching of the nasal mucosa.
- Involuntary bruising. Even at the site of the slightest blow, bruises form that take a long time to disappear.
- Appearance of purpura. Red spots on the skin or mucous membranes. They do not hurt, do not itch, and most often appear at the site of friction with clothing or as a result of microtrauma.
- Bleeding gums. After eating hard food or brushing your teeth, even with the softest brush, your gums begin to bleed.
- Bleeding in the gastrointestinal tract. The mucous membrane of the stomach and intestines is thin and quite delicate, so a decrease in platelets can lead to the appearance of blood in the stool or even vomiting.
- The appearance of blood in the urine. The walls of the ureters, kidneys or bladder may bleed.
- Heavy and prolonged bleeding during menstruation. It can appear both during the first menstruation in a girl and over time in an adult woman.
- Weakness, fatigue, headache, dizziness, decreased physical activity, pale skin, bruises under the eyes, shortness of breath. Blood performs a transport function in the body, and in the case of a decrease in platelets, and as a result of bleeding, which will lead to a decrease in the amount of blood in the body. Thus, the brain, muscles, heart and other organs do not receive enough nutrients and oxygen.
The manifestations and activity of symptoms depend on the severity of thrombocytopenia, which characterizes the number of platelets in the blood.
Severity of thrombocytopenia:
Light degree - from 50 to 150 *109/l. Most often, there are no obvious symptoms, and a low platelet level is diagnosed during preventive examinations or treatment of concomitant diseases.
Average degree - from 30 to 50 *109/l. General symptoms of malaise, irregular and mild bleeding due to injuries, which is difficult to stop
Severe degree - below 30 *109/l. Spontaneous and heavy bleeding into internal organs, inability to stop bleeding without hospital treatment.