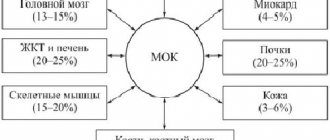
This disease is characterized by an abnormally low concentration of red blood cells. The red blood cells themselves contain hemoglobin, which carries oxygen to various parts of the body. With a reduced content of red blood cells, oxygen deficiency occurs and various parts of the body cease to function normally. Anemia (actually a drop in hemoglobin concentration) is detected in 58.7% of patients. Oncoanemia is calculated by the level of oxygen saturation of the blood, which drops to 12 g/dL and below. This condition is present in some cancer patients who have undergone chemotherapy. Oxygen deficiency in the circulatory system has a detrimental effect on a person’s general condition, worsening the prognosis.
Reasons for appearance
Red blood cells are produced in the bone marrow. A hormone called erythropoietin, produced by the kidneys, tells the body to increase the concentration of red blood cells. Oncology and its treatment can cause a drop in hemoglobin concentration in various ways: • certain chemotherapy drugs can damage the bone marrow, which has a detrimental effect on the production of red blood cells; • certain types of cancers that directly affect the bone marrow, or those types of cancer that metastasize into the bones are able to displace normal cellular components of the bone marrow; • chemotherapy drugs containing platinum compounds (for example, cisplatin) can damage the kidneys, reducing the production of erythropoietin; • radiation treatment of large areas of the body or the pelvic bones, legs, sternum and abdominal area can severely damage the bone marrow; • nausea, accompanying vomiting, loss of appetite can provoke a deficiency of nutritional components necessary for the production of red blood cells (in particular, there is a lack of folic acid and vitamin B12); • the immune response to the progression of cancer cells can also lead to a drop in hemoglobin.
The main goals of changing the diet of cancer patients are:
- ensuring good functioning of the immune system;
- neutralization and removal of decay products of malignant tumors from the body (detoxification);
- stimulation of a surge of vitality and energy for an active fight against cancer;
- ensuring the proper functioning of critical organs, especially the kidneys, liver and intestinal tract;
- in addition to the main treatment with the supply of natural substances that can slow down the growth of the tumor.
In foreign clinics, the patient is given special attention, which includes, among other things, choosing the right diet that would promote good health and increase the body's resistance. At the same time, doctors closely monitor changes in health and, if necessary, adjust food intake.
In Turkey, an integrated approach is used to treat cancer patients, so specialists create a balanced nutrition program for cancer. This helps maintain the patient’s strength and also minimize the side effects of radical therapy.
Diagnosis of the pathology in question
Treatment of anemia begins with a general blood test; Also, a biochemical blood test is done. With normal hemoglobin levels, the absence of the disease is diagnosed. When levels are less than 70 g/l, hospitalization and subsequent red blood cell transfusion are required. If hemoglobin drops too much, even people with stage 3-4 cancer are hospitalized. Sometimes doctors refuse to carry out hospitalization. In such situations, you need to be persistent, because transfusion must be carried out without fail. If the hemoglobin level is above 70 g/l, but below normal, you should look at the MCV indicators in the results of a biochemical blood test. This way it will be possible to determine the type of anemic pathology. Based on the average volume of red blood cells, you can understand whether this is due to iron deficiency. • MCV less than 80ft is a microcytic type of anemia caused by iron deficiency. • MCV is in the range of 80-100ft - it is normocytic (here we can talk about its aplastic, hemolytic or hemoglobinopathic type). • MCV above 100ft is macrocytic, caused by a lack of folic acid, vitamin B12, and nutritional deficiency.
Anemia in malignant neoplasms
The term “cancer anemia” has not found use in the medical literature. Most often, anemia is considered as one of the symptoms of the disease or as a complication of treatment without being classified as an independent nosological unit. Such a mechanistic interpretation of a decrease in hemoglobin concentration in the blood leads to a misunderstanding of the profound further consequences for the physical, social and psychological state of the cancer patient. How specific is anemia in cancer, what are its consequences and the degree of influence on the effectiveness of treatment? These are just some of the questions to which it is important to have answers.
A characteristic feature is the multifactorial nature of pathogenesis
Anemia is a syndrome, a pathological condition of the body that develops as a result of a disease and often worsens during chemotherapy. In this case, a decrease in blood Hb level below the physiological norm is recorded (
Antitumor treatment also affects the number of red blood cells in the blood. The main pathogenetic factors that reduce hemoglobin levels are myelosuppression and blocking the production of erythropoietin produced by the interstitial cells of the renal cortex.
Thus, anemia of malignant disease (AD) can be defined as a complex symptom complex, syndrome, pathological condition that develops during a malignant process as a result of disease and drug treatment. A decrease in hemoglobin levels below the physiological norm affects the patient’s quality of life, the prognosis of life and the course of the disease, and, probably, the effectiveness of specific treatment.
A characteristic feature of ADN is the multifactorial pathogenesis. The following mechanisms are clearly distinguished: inhibition of erythropoiesis, reduction in the lifespan of erythrocytes, impaired iron metabolism.
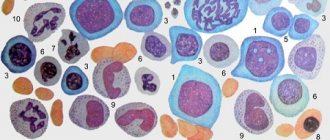
ADN refers to hyporegenerative anemia with a relatively reduced number of reticulocytes that does not correspond to the degree of anemia. There are differences between anemias of various types of ADN in terms of their severity, percentage of micro- and macrocytic forms. In most cases, however, ADN is a hyporegenerative anemia with a low reticulocyte count (reticulocytopenia), with hemoglobin values between 80 g/l and 100 g/l. The average erythrocyte volume and cellular hemoglobin concentration were within normal limits.
Most manifestations are due to anemic hypoxia
The pathophysiology of chronic anemia in MN involves intense interactions between the tumor cell population and the immune system, resulting in macrophage activation and increased expression of various cytokines. All of the characteristic pathophysiological features of ADN (reduced erythrocyte lifespan, decreased bone marrow iron recycling, inadequate erythropoietin (EPO) production, and suppression of erythroid precursors) result from activation of the immune and inflammatory systems by malignant cells.
As a rule, patients with anemia note manifestations caused by the development of anemic hypoxia. In mild forms, this may include weakness, fatigue, general malaise, and decreased concentration. People with more severe anemia may complain of shortness of breath with slight or moderate exertion, palpitations, headache, tinnitus, sleep disturbances, appetite disturbances, and decreased libido. In severe anemia or in the presence of concomitant pathology, heart failure may develop.
A frequently encountered diagnostically important symptom of moderate or severe anemia is pallor (of the skin, visible mucous membranes and nail beds). Symptoms such as increased cardiac impulse and heart sounds, and the appearance of functional systolic murmurs during auscultation of the heart are also valuable.
In addition to general symptoms directly related to the development of hypoxia, anemia may have other manifestations depending on the etiology and pathogenesis. For example, the development of neurological symptoms with concomitant vitamin B12 deficiency, jaundice with a hemolytic component.
Iron deficiency in ADN is characterized by so-called sideropenic symptoms: pronounced changes in the skin, nails, hair, which are not found in other types of anemia, muscle weakness that does not correspond to the depth of anemia, perversion of taste (pathophagy) and smell (pathosmia). Patients often experience dry and cracked skin on the arms and legs, and angular stomatitis.
A complete clinical blood test is required
Attention should be paid to the need to conduct a complete clinical blood test during the initial study, including determining the amount of hemoglobin, counting the number of erythrocytes and reticulocytes, color index and hematocrit index, as well as the number of leukocytes, platelets, leukocyte formula and ESR. The current practice in the clinic of studying only three indicators (hemoglobin, leukocytes, ESR) is not only not informative, but also harmful, as it can lead to erroneous conclusions. Fragmentary blood tests are permissible only with dynamic monitoring of the results of therapy.
When establishing the nature and causes of anemia, a syndromic approach is important, including assessment of the number of leukocytes, platelets, leukocyte formula and ESR value. If, for example, signs typical of myelo- and lymphoproliferative diseases, both acute and chronic, are detected, interpretation of the genesis of anemia will not present any particular difficulties. If during anemia there is a transient leukemoid reaction such as neutrophilic leukocytosis and thrombocytosis, this can help in the diagnosis of acute posthemorrhagic anemia, and the detection of leukopenia and thrombocytopenia along with anemia immediately raises a reasonable suspicion of hematopoietic aplasia or B12-deficiency anemia. The diagnostic value of ESR in anemia is also great.
By determining the color index and dividing anemia into hypo-, normo- and hyperchromic, it is possible to limit the range of diagnostic searches. Thus, when hypochromic anemia is detected, chronic iron deficiency anemia, or sideroblastic, should be assumed, and when hyperchromic anemia is detected, B12 or folate deficiency anemia, etc. are expected. It is necessary, however, to note that with modern instrumental calculation of the number of red blood cells, errors in determining the color index are possible, misleading the doctor: both iron deficiency and B12-deficiency anemia often turn out to be normochromic.
In this regard, it is of great importance to study the morphology of red blood cells by a laboratory assistant and describe it in a blood test. By detecting hypochromia and microcytosis of erythrocytes, iron deficiency can be diagnosed, and by detecting macrocytosis, megalocytosis, hyperchromia of erythrocytes, Cabot rings, basophilic punctuation, vitamin B12 deficiency can be diagnosed.
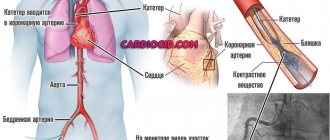
Basic treatment with donor red blood cells
Replacement therapy with donor red blood cells remains the basis for the treatment of severe anemia in chronic diseases. It should be emphasized that there is an extremely negative attitude towards blood transfusions in case of anemia of chronic diseases: each blood transfusion requires a separate justification - a sharp decrease in hemoglobin levels, an increase in hypoxia, vascular reactions, etc. You cannot routinely prescribe red blood cell transfusions “as planned.” In addition to the danger of viral infection, repeated blood transfusions are accompanied by hemosiderosis and inhibit, according to the feedback principle, their own erythropoiesis.
To some extent, blood transfusions are counteracted by recombinant erythropoietin (rh-EPO) therapy. In any case, if the question of blood transfusions arises for this type of anemia, it is necessary to discuss erythropoietin therapy. Erythropoietin was first isolated and reproduced in 1977 by M.I. Yake. The use of its recombinant form as a treatment for anemia in chronic renal failure was approved only in 1987, although the beginning of experimental use in the clinic dates back to 1985 (JW Eschabach). Since 1990, erythropoietin has been used to treat HIV-infected patients, and since 1993 - to treat anemia in patients with cancer.
This is an example of pathogenetic treatment that replenishes the deficiency of endogenous hematohormone. Eprex, Neorecormon, and Erythrostim have been available on the drug market for several years. A new erythropoiesis stimulator, darbopoietin, is being actively studied.
The indication for EPO therapy in a patient with ADN should be a hemoglobin level of less than 100 g/L, and rhEPO treatment is almost always required if the hemoglobin level is less than 80 g/L. First you need to differentiate other possible causes of anemia. In a situation where the number of reticulocytes is increased, one should keep in mind the hemolytic process or acute blood loss as possible causes. If the reticulocyte count is inadequate to the degree of anemia (i.e. less than 3-5%), nutritional deficiency (iron, vitamin B12 or folate) must be taken into account.
If symptoms of anemia are severe and we conclude that the anemia is a consequence of low red blood cell production and is due either to the disease itself, or to myelosuppressive therapy, or to both, then appropriate therapy should be prescribed. In this regard, we must discuss the pros and cons of EPO therapy.
Transfusion provides more rapid palliation of anemic symptoms, but with some inconvenience to the patient and some risk of acute or chronic reaction or transmission of infection. On the other hand, EPO therapy is free of risk factors and is convenient for the patient, who can inject himself at home, although the effect is slower compared to blood transfusion.
A very common misconception
Unfortunately, most doctors are accustomed to considering the development of mild or moderate anemia in cancer patients as inevitable. It is believed that reducing the Hb level to 10 g/dL and even to 8 g/dL does not cause significant harm to the patient.
How erroneous this point of view is was shown by studies of the relationship between quality of life and anemia, while timely and adequate correction of anemia significantly improved the well-being of patients. A significant effect of anemia correction on the effectiveness of chemotherapy, including in combination with radiation treatment, has been shown. The results of prospective and retrospective studies conducted over the last decade convincingly indicate that the problem of anemia and its importance for the patient are clearly underestimated. The introduction into clinical practice of a number of new cytostatics, the active use of aggressive treatment regimens, including simultaneous chemotherapy and radiation therapy (for example, for localized small cell lung cancer), and the use of high doses of interferons and interleukins can increase the effectiveness of treatment of a malignant disease. But intensification of treatment worsens the quality of life of patients and requires active maintenance therapy, one of the components of which is the timely correction of anemia with the use of modern drugs - erythropoiesis stimulants.
The first symptoms of oncoanemia
The primary indicators of the defect in question are sudden paleness of the skin and impaired functionality of the digestive system. Most patients lose their appetite; they suffer from constant nausea. The development of cancer is accompanied by a gradual deterioration of the condition. There is systematic malaise, muscle weakness, accelerated fatigue, and loss of former ability to work. Quantitative examination of the circulatory system must be carried out a certain number of times during the treatment of anemia. Thus, the dynamics of cancer progression is assessed.
Treatment of anemia in cancer patients
The main advantage of the intravenous administration of erythrocyte drugs is the rapid restoration of the optimal hemoglobin concentration. However, this approach provides a short-term effect. If the pathology in question begins to show symptoms, a blood transfusion containing a sufficient number of red blood cells may be required. Some people with low hemoglobin caused by chemotherapy can be treated with epoetin alfa or darbepoetin alfa. These medications are forms of erythropoietin produced in the laboratory. They send a signal to the bone marrow to increase the production of red blood cells. In order to eliminate iron deficiency, these medications must be combined with intravenous injections of products containing iron. According to statistics, in 45% of cases a good result is achieved through a combination of erythropoietin and iron. Sometimes you can even get by with just the use of iron supplements.
Nutrition for cancer is prepared using the following useful products:
- Yellow, orange, and reddish-orange fruits and vegetables are believed to contain carotenoids that have beneficial effects against cancer. First of all, these are: apricots, citruses, carrots, tomatoes, zucchini. Beta-carotene, lutein, lycopene improve immunity and protect cellular structure from radiation.
- If the liver is damaged, meals should be fractional, without fatty and heavy foods, and include a sufficient amount of vitamins, proteins that are easily digestible, microelements and fiber.
- Broccoli, radishes, cauliflower and Brussels sprouts, turnips, and mustard are classified as cruciferous vegetables that contain indole, an active element that helps cleanse the liver and neutralize harmful chemical factors.
- Some varieties of green plants are rich in chlorophyll, so including them in the diet for cancer helps against abnormal elements and microbes. Such representatives include blue-blue and unicellular green algae, green peas and mustard, dandelion shoots, cabbage, and nettle leaves.
- Green tea is famous for its various strengthening properties.
- Pineapple, broccoli and garlic have an antitumor effect and stimulate detoxification. They reduce the likelihood of developing nitroso-induced oncology.
- For breast cancer, it is recommended to increase the intake of vitamin D, bran, whole grain cereals and their sprouts, beans, and bran.
- Ellagic acid, which prevents oxidation in cell membranes and is considered a good antioxidant, is contained in: raspberries, grapes, strawberries, strawberries, pomegranate, and blueberries.
- Fruits and vegetables of blue, red or lilac colors include anthocyanidins - antioxidants that activate the body's defenses, reduce the effects of free radicals, viral agents and carcinogens, and remove substances including chemical breakdown products and harmful elements. Representatives of this group include: blue cabbage, cherries, beets, various types of grapes, blackberries, blueberries.
- If you have pancreatic cancer, you cannot eat some healthy foods. For example, dates, bananas and grapes. Low-fat dairy products will have an effective effect.
Scientists have found that a cancer treatment diet that contains brown seaweed (also known as Japanese kelp) and blue-green algae helps reduce tumor size.
Various freshly squeezed juices and fruit drinks have a good effect.
The diet of cancer patients must include foods that contain omega-3 fatty acids. The best examples are fish oil and fatty sea fish. Also important acids are contained in flaxseed oil and seeds.
It is imperative to maintain favorable microflora in the intestinal tract. To ensure this, doctors recommend including the optimal amount of asparagus, garlic, tomatoes, onions, and sprouted wheat in your daily diet. If you need to induce a laxative effect, you can use prunes. Blueberries help reduce putrefactive processes and fermentation, as well as the accumulation of gases.
If you have cancer, doctors also recommend including the following foods in your diet:
- potatoes, peppers and beans;
- gooseberries, rose hips, hawthorn fruits;
- apples, peaches;
- parsley dill;
- buckwheat, brown rice, oats, barley;
- basil, celery, spinach;
- parsnips, lentils, peas, coriander;
- horseradish, melon, turnip, eggplant, radish;
- corn, basmati rice, pumpkin;
- wheat and its live sprouts;
- sea buckthorn, lingonberry, red and black currant, chokeberry, cranberry;
- honey (has anti-inflammatory, antioxidant and anti-carcinogenic effects).
The material was prepared in agreement with the doctors of the Anadolu Clinic.
Erythropoietin in palliative care
In the first stages of anemia treatment, the full dosage of the medication is prescribed. If during a month of such treatment the hemoglobin concentration increases by 10 g/l, the dosage is reduced by a quarter. If over the same period of time the hemoglobin concentration increases by 20 g/l (or more), the dosage is reduced by half. If the hemoglobin concentration exceeds 130 g/l, the course of taking erythropoietin is temporarily stopped (until the level drops to 120 g/l). After this, the course is resumed, but the initial dosage is already reduced by a quarter.
If monthly use of such a remedy is unsuccessful, the dosage is increased (however, it must be within the maximum permissible limits). If a drop in hemoglobin is caused by a lack of nutritional components, iron tablets may be prescribed. Vitamin B12 and folic acid tablets may also be prescribed. Eating foods containing a substantial dose of iron (red meat, certain fruits, almonds) can be of great help in treating anemia.
Low hemoglobin symptoms
Hemoglobin levels can be easily measured using a laboratory blood test, which can be prescribed by the local physician observing the patient. If you suspect a decrease in hemoglobin, and there is no time to wait for an appointment at a city clinic, you can contact any private laboratory. Such institutions often offer discounts on comprehensive examinations. You can donate blood to such an institution any day. The laboratory will not require you to buy your own syringe and container.
Symptoms to suspect low hemoglobin levels:
- daily weakness that does not disappear even on rest days;
- pale skin;
- there is a decrease in memory;
- tremor of the limbs appeared;
- hair lost its shine and began to fall out;
- shortness of breath appeared;
- Heart rate increased even at rest.
At the first signs of a decrease in hemoglobin, you should consult a doctor or donate blood yourself to check the iron level in your blood. However, detecting a decrease in hemoglobin is not enough. It is important to determine the reason why the body lacks it.
Danger and consequences
Doctors believe that a drop in hemoglobin concentration accompanies all cancer pathologies. A deficiency of red blood cells is dangerous because oxygen starvation of all tissue components can develop. In addition, the presence of such a defect complicates the course of chemo-radiation therapy.
The consequences of the pathology depend on the stage of initial diagnosis of the oncological process. Red blood cell deficiency detected in the early stages usually has a positive prognosis. The favorable outcome is due to the high chances of 100% cure of anemia. Oncoanemia with poor prognosis is usually present in people with stage 3-4 cancer, which causes intoxication, metastasis and death.
Diet for cancer patients
Diet and nutrition during cancer treatment are incredibly important. A balanced and rational diet is necessary regardless of the stage of development of the disease in the patient.
A diet for cancer helps improve overall well-being, maintain normal body weight, regenerate healthy cellular structures after chemotherapy and radiation, maintain the balance of nutrients and their proper metabolism, and also prevent the appearance of foci of infection and inflammation, and exhaustion.
Find out the price
Find out the price
Error! Please fill in all required fields
Thank you! We will contact you shortly
✕