Disease or symptom?
Urinalysis is one of the main laboratory tests that is carried out at the stage of diagnosis. If the test results indicate hematuria, the doctor will definitely refer the patient for further examination. Why? Hematuria is the presence of blood in the urine. Obviously, normally there should be no blood in the analysis.
Since this is not an independent disease, but a symptom that may indicate serious health problems, the doctor will prescribe an additional examination to establish an accurate diagnosis.
Causes and symptoms
Based on the reasons for its occurrence and the nature of its development, ischemia is divided into:
- Coming due to prolonged compression of the artery leading to the organ. The cause may be a scar, tumor, foreign body, or accumulated fluid.
- Arising as a result of arterial spasm. The cause may be the use of vasoconstrictor drugs, severe emotional or physical shock: panic, pain shock, hypothermia, mechanical irritation.
- Occurring due to partial or complete blocking of the artery by a thrombus or embolus. Also, closure of the lumen is possible due to vascular diseases: atherosclerosis, obliterating endarteritis, periarteritis nodosa.
Ischemia can also develop due to injury - due to mechanical rupture of blood vessels or blood loss, as well as due to blood diseases - an increase in its viscosity.
Any form of the disease is characterized by disruption of the normal functioning of organs - slowing of blood flow and disruption of metabolic processes, sometimes very severe. Symptoms in the affected area include:
- dystrophic changes and decreased tissue elasticity;
- lowering temperature and blood pressure - for the extremities;
- numbness, tingling and pain.
If these symptoms occur, we strongly recommend that you consult a doctor immediately.
But chronic cardiac ischemia may not manifest itself clinically, while remaining very dangerous. The appearance of the first symptoms may indicate an advanced process. They are:
- Pain in the chest, which intensifies with physical activity and may subside as it continues.
- Shortness of breath and a feeling of interruptions in the heart. If these symptoms appear, you must consult a doctor as soon as possible, and if an attack of pain occurs for the first time or its nature is unusual, you must immediately take nitroglycerin and call an ambulance.
Nowadays, it is possible to help a person in any situation and at any stage of the disease. Although, of course, the effectiveness of this help and the prognosis are much better if you consult a doctor in the early stages.
The doctor can identify ischemia or the risks of its manifestation in the initial stages of the disease. For this purpose, a detailed analysis of risk factors and exercise tests are used: treadmill test, bicycle ergometry, stress echocardiography. As well as vascular examination: coronary angiography, multislice computed tomography and ultrasound - the most accessible method, recommended as a screening or first-line study.
Types of hematuria
There are micro- and macrohematuria. Macrohematuria can be seen with the naked eye - the urine turns red or brown. Microscopic hematuria is determined laboratory.
Despite the fact that with the latter the amount of blood in the urine is not large, both conditions can be dangerous.
It is worth noting that patients sometimes see blood in the urine when there is none. Urine changes color when consuming certain foods (beets, black currants and beans, blackberries, rhubarb) or medications (metronidazole, rifampicin, etc.).
Causes
“Kidney hematuria” is a diagnosis made by patients who find blood in their urine. We recommend not to engage in self-diagnosis, but to consult a urologist or nephrologist in time, because this phenomenon has many causes. Let's look at the main ones.
- Infections of the kidneys and urinary tract (cystitis, urethritis), prostate gland, genital organs
- Urolithiasis (sand and stones in the kidneys, bladder, ureter)
- Neoplasms (tumors of the kidneys, bladder, benign prostatic hyperplasia, etc.)
- Glomerulonephritis
- Kidney and urinary tract injuries
- Kidney infarction
- Hereditary pathologies
- Drug therapy (taking certain antibiotics, anticoagulants, drugs used in oncology).
Indications and contraindications
Indications
- benign and malignant tumors within the organ;
- partial kidney damage due to injury or tuberculosis;
- urolithiasis with ineffective conservative therapy;
- kidney infarction;
- having only one kidney;
Contraindications
- diseases of an inflammatory or infectious nature;
- concomitant diseases of the body in the stage of decompensation;
- some blood pathologies;
- terminal stage malignant diseases.
When the kidneys have nothing to do with it
Hematuria and kidney (genitourinary) diseases are not always related. Sometimes the cause of blood in the urine is heavy physical activity. For example, this condition can occur in long-distance runners.
Blood is also detected in the tests of women who neglected the rules for collecting urine for testing during menstruation.
Occasionally, the “culprit” of the problem is sexual intercourse preceding the clinical analysis.
The presence of single erythrocytes (red blood cells, not hemoglobin, as some patients incorrectly believe) in morning urine, which is collected according to all the rules after hygiene measures, is considered the norm.
Diagnostic methods
In order not to make a mistake in the diagnosis, the attending physician - a nephrologist or urologist - will prescribe a number of clarifying tests, including a general blood test, sediment microscopy according to Nicheporenko, creatinine level, concentration of sodium, calcium and potassium in the blood serum.
Additionally, the patient is sent for studies that visualize the kidneys and urinary tract: urography, CT, cystoscopy. Men may be prescribed an ultrasound of the prostate, and women may be prescribed an ultrasound of the pelvic organs.
An important role is played by collecting anamnesis: clarifying symptoms (where the pain is located and how severe it is), lifestyle and hereditary factors.
Hematuria in children: difficulties in making a diagnosis
Determining the causes of blood in a child’s urine has its own characteristics. In a conversation with the parents, the doctor finds out when hematuria was first noted in the tests. Early appearance of blood indicates a congenital pathology. Suspicions are aggravated if the child has chronic hematuria.
An important diagnostic sign that helps the doctor make a diagnosis is the combination of hematuria and proteinuria (protein in the urine) in the analysis. It confirms that the source of the blood is a kidney disorder.
We are treated correctly
It is important to know: if you have hematuria, medication is not the first thing you should worry about. The priority is to consult a doctor, since blood in the urine is not a disease, but a symptom.
Infectious diseases that cause blood to appear when urinating are treated with medication. Surgery cannot be avoided if advanced urolithiasis, tumors and some types of congenital pathologies are detected.
If the cause of unpleasant symptoms is a kidney infection, the patient must adhere to a special diet for some, possibly a long time.
Hematuria: medications that may be required during treatment
Most cases of blood in the urine are not associated with dire diagnoses, but with common kidney and urinary tract infections. This means that the treatment will be simple and effective. Patients will be prescribed antibiotics, anti-inflammatory drugs, and decongestants.
Severe hematuria requires additional drug treatment: these are drugs that stop the blood - dicynon, transekam. During the recovery period, iron supplements, for example, heferol, are prescribed. Vitamin complexes have also proven themselves well.
Myocardial infarction
Heart attack
To this day, people sometimes hear, mainly from people of the older generation, something like the following popular cardiological phrases: “This way you can get a heart attack, that is, heart rupture” (usually meaning shock from surprise or, say, from good news).
We bow to our indestructible grandfathers and grandmothers, and may all the news only bring joy to their tired hearts. However, given the exceptional importance of the topic, it is still worth making certainty in the terminology.
A heart attack is not a rupture of the heart. Moreover, we are not even necessarily talking specifically about the heart: no sweeter, say, an infarction of the brain or spinal cord, an infarction of the kidney or intestines.
And the definition that one of the largest search engines on the Internet gives to a heart attack with automatic importunity: “... cessation of blood flow due to spasm of the arteries or their blockage” is also incorrect. A heart attack is not a “cessation of blood flow,” but the result of such a cessation; the result is always pathological and, as a rule, severe.
Therefore, we will strive for accuracy of definitions and clarity of formulations. The topic is really too serious.
Any living tissue, as we know, consists of cells. For normal operation and effective performance of their functions, these cells must breathe, eat and get rid of waste products of metabolism (metabolism). All these processes are ensured by blood flow or, more precisely, by perfusion - constant “impregnation”, through the flow of blood through the tissue, for which the system of capillaries, the smallest blood vessels, is responsible. Arterial blood enters the capillary system, bringing nutrients and oxygen bound by red blood cells to the tissue. Then, through the small, large and main veins, the blood is drained to the lungs, liver, kidneys - for a new cycle of filtration, detoxification, enrichment and gas exchange.
The pumping function, that is, pumping blood under pressure through this complex vascular system, is performed by the heart muscle, or myocardium. The contractile activity of the heart begins in the womb, in the first weeks of pregnancy, and continues non-stop until the last minute of a person’s life. The opposite is also true: the last minute occurs due to the fact that the rhythmic alternation of contractions (systole) and relaxations (diastole) stops.
However, the myocardium, as a hollow pumping muscle (which is anatomically and histologically very complex) consists of living tissues that also need nutrition and oxygen. In this sense, the myocardium is no different from other organs: it itself needs tissue perfusion of blood, continuous and quite intense, given its lifelong work 24/7 without weekends or holidays. The blood supply to the heart is carried out through a special arterial-venous circuit. Due to its external resemblance to the attribute of monarchy, the myocardial circulation is called coronary, or coronary.
Insufficient volume of blood flow through tissue (any tissue, not just the heart) is called hypoperfusion. The widely known term “ischemia” was interpreted differently at different stages of the development of medicine; Today, ischemia is understood as a pathological state of tissue that develops as a result of hypoperfusion, and the obligate (mandatory for the use of the term or diagnosis) signs of ischemia are violations of all the basic processes provided by the tissue blood supply - nutrition, oxygenation (oxygen saturation) and waste removal.
Thus, coronary heart disease (CHD) is chronic starvation and/or “clogging” of myocardial tissue, caused by insufficient functioning of the coronary circulatory circuit. There are many known risk factors and direct causes of the development of ischemic heart disease, as well as its clinical variants, but now something else is more important: this situation inevitably leads to overload, premature wear, degenerative-dystrophic changes in tissues and various malfunctions in the functioning of the heart muscle (for example, attacks angina). In conditions of constant ischemia, the myocardium, brain, kidney and any other organ simply cannot fully perform their functions - just as an athlete who is suffocating and living from hand to mouth will not be able to engage in professional sports.
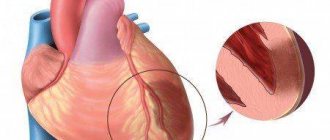
A heart attack is a simultaneous mass death of cells in a local area of tissue. In other words, this is rapid focal necrosis, occurring as a result of a sharp reduction in blood supply (incomplete ischemia) or a complete cessation of perfusion (total ischemia).
Myocardial infarction is the death of one or more areas of the heart muscle, which occurs due to the fact that coronary blood has stopped circulating in these areas.
A wealth of information is now available regarding myocardial infarction. It is not always, as shown above, reliable and accurate, but in any case it is better than a complete misunderstanding of the normal and pathological processes occurring in one’s own body. We will not dwell on the details of epidemiology here, but we will briefly note the four most significant and alarming points.
Firstly, cardiovascular diseases (primarily ischemic heart disease and heart attacks) stubbornly hold the lead in statistical indicators of non-violent mortality: their share in the overall mortality structure, according to WHO estimates, exceeds 30%.
Secondly, the mortality rate in Russia is two and a half times higher than the European average; three times higher than in the USA; nine times higher than in Japan.
Thirdly, heart attacks are constantly “getting younger”: the average age of primary patients with coronary artery disease and heart attacks is steadily decreasing from year to year.
Fourth, 80% of myocardial infarctions were preventable.
List of used literature
- Nikolaev A. Yu., Shcherbin A. A. et al. The mechanism of hematuria in hematuric nephritis // Ter. archive, 1988, No. 6, p. 34–37.
- Burtsev V.I., Turchina L.P. Hematuria // Clinical Medicine, 1997, No. 6, p. 66–69.
- Pediatric nephrology [Text]: practical work. hands / ed. E. Loyman, A. N. Tsygin, A. A. Sarkisyan. - Moscow: Litterra, 2010. - 400 p.
- Urolithiasis disease. Modern methods of diagnosis and treatment [Text] / Yu. G. Alyaev [etc.]; edited by Yu. G. Alyaeva. - Moscow: GEOTAR-Media, 2010. - 224 p. : ill. - (B-specialist doctor).
Modern radiodiagnosis of kidney abscess
Kidney abscess is one of the most dangerous urological pathologies, threatening the patient with severe, sometimes even fatal consequences, if this condition is not diagnosed in time and effective therapy is not carried out. The main difficulty in timely detection of the disease is that the clinical picture of a kidney abscess imitates the clinical picture of acute pyelonephritis [1, 3, 5-7, 10].
A kidney abscess is a limited purulent inflammation in which the tissues of the organ melt and a cavity filled with pus is formed. In most cases, the disease occurs as a result of insufficient or improper treatment of purulent pyelonephritis (Fig. 1). Bacteria enter the organ through the blood or urinary tract, cause inflammation and damage the kidney tissue. In some cases, an abscess develops against the background of diabetes mellitus, urinary tract injury, is a direct consequence of a calculus in the pelvis or ureter, or as a complication after surgery (for example, surgery to remove kidney stones). In some cases, the possibility of local hematogenous infection of the kidney, which causes ischemic infarction and suppuration, cannot be excluded [1, 3, 5-7, 10].
Rice. 1.
Kidney abscess.
A kidney abscess can occur independently and then in its involutive process it goes through 3 phases: the phase of acute inflammation, purulent melting and chronicity. Single and multiple abscesses may occur.
In some cases, when the abscess is located within the upper or lower segment of the kidney, sequestration of a large area of the renal parenchyma may occur. Cases of abscess formation after a stab wound to the kidney have been described.
There are also so-called metastatic kidney abscesses, which occur when infection is introduced from extrarenal foci of inflammation. The source of infection is often in the lungs (destructive pneumonia) or the heart (septic endocarditis) [1, 3, 5-7, 10].
Solitary abscesses most often occur on one side, metastatic ones are often multiple and bilateral.
An abscess of the renal cortex can open:
- through the kidney capsule into the perinephric tissue with the formation of a perinephric abscess;
- into the collecting system and emptying through the urinary tract system;
- into the abdominal cavity.
It can also become chronic and simulate a kidney tumor.
There are the following types of kidney damage in this pathology [11]:
- pyelonephritis and perinephric abscess;
- pyelonephritis and perinephric abscess and calculus;
- pyelonephritis and parenchymal abscess;
- pyelonephritis and parenchymal and perinephric abscesses;
- pyelonephritis and pelvicaliceal and perinephric abscesses;
- pyelonephritis and pelvicaliceal abscess spreading into the cortex;
- pyelonephritis and pelvicaliceal abscess;
- pelvicaliceal abscess (without pyelonephritis).
The general symptoms of a kidney abscess do not differ from those of any severe septic disease:
high body temperature with tremendous chills, frequent, weak pulse, shortness of breath, thirst, general weakness, headache, scleral icterus, adynamia, euphoria. Body temperature is set at high levels (39-41 ° C). Among the local symptoms in the diagnosis of the disease, intense pain in the kidney area is important, resulting from a disorder of blood and lymph circulation in the kidney and compression of the edematous kidney tissue in a dense, low-extensibility fibrous capsule. The pain is especially intensified by palpation of an enlarged and tense kidney or by tapping the lumbar region. The protective tension of the lumbar muscles and the anterior abdominal wall is always sharply expressed. Often, patients with a kidney abscess take a forced position with the leg adducted to the stomach, the extension of which causes sharp pain in the lumbar region on the side of the disease (a sign of reactive psoitis). Bacteriuria and leukocyturia usually appear late in the disease, when the abscess breaks into the urinary tract. If the fibrous capsule of the kidney melts and the contents of the abscess are emptied into the perinephric tissue, then purulent paranephritis occurs [1, 3, 5-7, 10].
On the overview urogram
you can detect a curvature of the spine in the direction of the lesion and the absence of a shadow of the psoas muscle on this side, an enlargement of the kidney. Sometimes in the area where the abscess is localized, a bulging of its outer contour is noted.
On excretory urograms
a decrease in the excretory function of the kidney, compression of the renal pelvis or cups, and their amputation are determined. The mobility of the kidney is limited at the height of inspiration and after exhalation. When pus breaks through into the pyelocaliceal system, a cavity filled with radiopaque liquid is visible on the urogram.
Radioisotope nephrography
indicates a normal functional state of the kidneys, which allows us to indirectly assume the presence of a kidney abscess with clinical symptoms of purulent damage. Dynamic scintigrams in the area of the abscess reveal an avascular space-occupying formation.
Ultrasound examination (ultrasound)
Valuable information can be obtained from ultrasonography - a cavity containing fluid (pus) is detected (Fig. 2, 3).
Rice. 2.
Ultrasound image of the right kidney of patient V. Conclusion: urolithiasis on the right. Expansion of the abdominal system on the right. Right ureteral calculus. Abscess of the right kidney.
A)
On the right, the abdominal system is significantly expanded (calyces up to 18 mm, pelvis up to 21 mm, ureter up to 11 mm).
b)
Two stones measuring 5 and 9 mm are visualized in the right ureter (white arrow).
V)
On the right, in the lower group of cups there are stones up to 5 mm in size (white arrow) and a liquid formation (red arrow).
G)
In the middle third on the right, a liquid formation measuring 40 x 42 mm with a thick capsule, with septations inside and a hyperechoic suspension (white arrows) is visualized.
Rice. 3.
Ultrasound image of the left kidney of patient S. Diagnosis: pyonephrosis on the left. Serous-purulent paranephritis on the left. Coral stone of the left kidney. Postoperative histology: purulent calculous pyelonephritis, pyonephrosis, hydronephrosis, chronic urethritis, serous-purulent paranephritis, mixed immune response in the lymph nodes.
A)
The left kidney is significantly increased in size due to severe hydronephrosis, the calyces are clearly dilated, the contents of which are thick liquid.
b)
In the projection of the pelvis, a staghorn calculus is visualized (white arrow).
V)
The parenchyma of the left kidney is practically absent, the calyces are filled with a hyperechoic suspension (blue arrows) and a staghorn calculus is visualized (white arrow).
Ultrasound of the kidneys reveals the following signs of an abscess:
- hypoechoic foci in the parenchyma with sizes from 10 to 15 mm or more;
- unevenness and bulging of the outer contour of the kidney at the site of the abscess;
- significant reduction in kidney excursion;
- decreased echogenicity of the parenchyma.
On Dopplerograms, there is no vascular pattern in the abscess area.
In the acute phase, it is a round, focal formation of different sizes, of lower echogenicity than the surrounding parenchyma. The parenchyma zone in this phase does not undergo structural changes.
Depending on the location, the abscess may bulge somewhat above the contour of the kidney or compress the pelvis. With small abscesses, the kidney remains normal in size; with large and multiple abscesses, the kidney is enlarged, the capsule is thickened, and a low-echoic zone of perinephric tissue infiltration is located around it (a sign of secondary paranephritis). In the phase of purulent melting, a cavity is formed with unclear intermittent contours, the contents of which are low-echoic, with point or linear echogenic inclusions.
In the chronic phase, a thick, unevenly echogenic capsule is formed around the abscess; the contents combine floating signals of low and high echogenicity; sometimes two levels of different echogenicity are observed (dense and liquid layers of pus). In rare cases, the abscess cavity shrinks and calcifies.
Computed tomography (CT)
More informative is CT, which reveals a kidney abscess in the form of a zone of reduced accumulation of contrast material in the kidney parenchyma in the form of single or multiple decay cavities, which, merging, turn into large abscesses. The abscess has the appearance of a rounded formation of increased transparency with an attenuation coefficient from 0 to 30 HU. During the control study, a clear demarcation of the focus of destruction from the kidney parenchyma is noted.
CT makes it possible to detect not only intrarenal or perinephric fluid accumulations, but also the presence of gas in the abscess cavity. Using this method, it is also possible to establish the ways of infection spreading into surrounding tissues. These data can be useful in choosing a surgical approach and determining the extent of surgical intervention (Fig. 4).
Rice. 4.
CT scans of patient B. The CT scan was performed without intravenous contrast agent (the patient has high waste products). Conclusion: multiple kidney abscesses.
A)
The right kidney is rotated along the horizontal axis, its dimensions are 13 x 7 x 7 cm, the parenchyma is not thinned. In the calyx of the lower group there is a calculus measuring 8 x 3 mm (white arrow).
b)
The renal cavity system is expanded, the pelvis measures 44 x 27 mm, the right ureter is expanded to 15 mm. In the upper third of the right ureter there are 2 stones measuring 8 and 5 mm (white arrow).
V)
In the parenchyma, in the middle third, with access to the anterior contour, with close adherence to the liver, a rounded formation up to 40 mm in size is determined, a heterogeneous structure, closer to liquid in density, its wall is fragmentary up to 5 mm (blue arrow). In addition, in the kidney parenchyma there are several similar formations up to 20 mm in size (white arrow). The perinephric tissue is somewhat infiltrated.
G)
In the parenchyma, in the middle third, with access to the anterior contour, with close adherence to the liver, a rounded formation is determined, up to 40 mm in size, of a heterogeneous structure, closer in density to liquid, its wall is fragmentary up to 5 mm. In addition, in the kidney parenchyma there are several similar formations up to 20 mm in size (white arrow). The perinephric tissue is somewhat infiltrated.
Treatment for kidney abscess
consists of decapsulating the kidney, opening and draining the abscess and paranephrium using rubber gauze swabs and drainage tubes. In case of extensive purulent-destructive damage to the kidney and satisfactory function of the opposite kidney, nephrectomy is performed [4, 8, 9, 11-13].
Differential diagnosis of a kidney abscess should be carried out with a simple kidney cyst, polycystic kidney disease, or subcapsular hematoma of the kidney.
A simple kidney cyst on ultrasound (Fig. 5) has a round shape and clear, even contours. The wall is not visible, internal structures and partitions are absent; the cyst has echo-negative content and a clear mirror artifact (dorsal enhancement effect).
Rice. 5.
Ultrasound picture of a simple kidney cyst: a liquid formation of regular shape is determined, with a thin capsule, anechoic, giving an enhancing effect.
In case of kidney injury, echography allows one to assess the nature and extent of damage, as well as the surrounding organs, and the condition of the second kidney. Trauma with a violation of the integrity of the renal parenchyma and intra- or perinephric hematoma (Fig. 6) is accompanied by a change in the structure and density of tissue, which is reflected in ultrasound scanograms. Here the clinical picture and anamnesis data (trauma) are of great importance.
Rice. 6.
Subcapsularly in the left kidney, a liquid formation measuring 104 x 62 cm is visualized, with septations inside and a hyperechoic suspension.
Ultrasound allows you to diagnose polycystic kidney disease (Fig. 7) by the number of echo-negative zones. In the early stages of polycystic kidney disease, ultrasonography reveals their enlargement. Sometimes, to clarify the diagnosis, renal angiography is necessary (saturation defects are detected, renal vessels are narrowed, the number of small arteries is reduced, and fields without vessels corresponding to cysts are also determined).
Rice. 7.
Ultrasound picture of polycystic kidney disease. The presence of multiple anechoic formations of various diameters.
Also, a kidney abscess must be differentiated from cystic kidney cancer (Fig. 8). Here, much attention is paid to the clinical picture, as well as CT data.
Rice. 8.
Computer tomograms: doubling of the cavity system of the left kidney is determined, the kidney is rotated anteriorly. Conclusion: histous kidney cancer.
A)
At the border of the upper and middle third of the kidney (the level of the upper cavitary system) in the parenchyma/calyces, a tumor-like formation of an irregular shape of a cystic-solid nature is determined with an exit to the posterior contour and prolapse into the perirenal fat, dimensions in axial sections are 38 x 39 mm, vertical dimension is 45 mm .
b)
After intravenous contrast enhancement, the accumulation of contrast agent is determined by the solid part of the formation (multiple septa of different thicknesses), which is intimately adjacent to the muscles at the level of interest. Kidney function is preserved.
V)
After intravenous contrast enhancement, the accumulation of contrast agent is determined by the solid part of the formation (multiple septa of different thicknesses), which is intimately adjacent to the muscles at the level of interest. Kidney function is preserved.
G)
After intravenous contrast enhancement, the accumulation of contrast agent is determined by the solid part of the formation (multiple septa of different thicknesses), which is intimately adjacent to the muscles at the level of interest. Kidney function is preserved.
Clinical example
Patient V., 35 years old. He has been suffering from chronic glomerulonephritis for 20 years.
The real deterioration after hypothermia since September 2014, when there was a rise in body temperature to 39 ° C, chills, and a dry cough, did not go to the doctor. He continued to work, noted an increase in body temperature in the evening with chills, sweating, and stopped the attacks with paracetamol with a short-term positive effect. Since November, the increase in body temperature began to be constant, with periodic rises to 40 °C. I went to the doctor.
On ultrasound, the kidneys are located in a typical manner. The right kidney is of normal size, mobility is preserved. The left kidney is significantly increased in size, 170 x 90 mm, parenchyma 19 mm. Almost the entire kidney is represented by liquid formations with a diameter of 15 to 37 mm, containing a hyperechoic suspension and multiple septa. The abdominal system is not expanded, no stones were identified. Conclusion: multiple abscesses of the left kidney (Fig. 9).
Rice. 9.
Ultrasound examination of patient V.
A)
Multiple fluid formations of the left kidney of various diameters with septations and a hyperechoic suspension inside.
b)
Multiple fluid formations of the left kidney of various diameters with septations and a hyperechoic suspension inside.
V)
Multiple fluid formations of the left kidney of various diameters with septations and a hyperechoic suspension inside.
G)
Ultrasound examination with color circulation. Formation without signs of blood flow.
A CT scan reveals a volumetric formation in the left kidney of an irregular shape, slightly beyond the contours of the kidney, of a heterogeneous, soft tissue-liquid nature, with multiple delimited fluid accumulations. When contrasted, the soft tissue component is slightly enhanced in the parenchymal and delayed phases; the liquid component is not enhanced. In the adjacent sections, swelling of the fatty tissue and a small amount of free and encysted fluid along the renal fascia were noted. At the level of the kidney, multiple lymph nodes up to 18 mm in size are identified on the left para-aortic (Fig. 10). Conclusion: abscess of the left kidney.
Rice. 10.
Computer tomograms of the kidneys of patient V.
A)
In the left kidney, a volumetric formation of irregular shape is determined, slightly beyond the contours of the kidney, of a heterogeneous, soft tissue-liquid nature, with multiple delimited fluid accumulations.
b)
When contrasted, the soft tissue component is slightly enhanced in the parenchymal and delayed phases, the liquid component is not enhanced.
V)
When contrasted, the soft tissue component is slightly enhanced in the parenchymal and delayed phases, the liquid component is not enhanced.
G)
When contrasted, the soft tissue component is slightly enhanced in the parenchymal and delayed phases, the liquid component is not enhanced.
The diagnosis was confirmed by left-sided nephrectomy.
Conclusion
Ultrasound is the main method for diagnosing a kidney abscess and a monitoring method in the postoperative period, allowing to monitor the course of the disease, record the degree of regression of the purulent cavity, and promptly detect the formation of new foci of destruction in the kidney and/or retroperitoneal space. CT makes it possible to detect not only intrarenal or perinephric fluid accumulations, but also the presence of gas in the abscess cavity. Using this method, it is also possible to establish the ways of infection spreading into surrounding tissues. These data can be useful in choosing a surgical approach and determining the extent of surgical intervention.
Literature
- Antonov A.V. Fluid formations of the retroperitoneal space: diagnosis and treatment // Urological Gazette. 2012; 2 (4): 32-41.
- Gadzhiev A.N. Percutaneous puncture drainage for purulent-inflammatory diseases of the kidneys and retroperitoneum: Diss. ...cand. honey. Sci. M., 2021.
- Derevyanko I.M., Derevyanko T.I. Paranephritis. Stavropol, 2000. 61 p.
- Kvyatkovsky E.A. Ultrasonography and Dopplerography in the diagnosis of kidney diseases. Dnepropetrovsk: New ideology, 2005. 318 p.
- Mikhin I.V., Bublikov A.E. Pyelonephritis: clinical picture, diagnosis, surgical treatment. Volgograd, 2012. 84 p.
- Sinyakova L.A. Purulent pyelonephritis. Diagnosis and clinical features // Urology and nephrology. 2001; 5: 68-73.
- Sinyakova L.A. Purulent pyelonephritis. Modern diagnostics and treatment: Author's abstract. diss. ...Dr. med. Sci. M., 2002.
- Teodorovich O.V., Gadzhiev A.N. Percutaneous puncture drainage of the kidneys: 10th Plenum of the All-Russian Society of Urologists. M., 2002: 792.
- Teodorovich O.V., Sinyakova L.A. The role of percutaneous drainage methods in the treatment of purulent pyelonephritis: 10th Plenum of the All-Russian Society of Urologists. M., 2002: 793.
- Chaly M.E., Amosov A.V., Gazimiev M.A. Diagnosis of acute pyelonephritis in the postoperative period using color echo Dopplerography: Russian Society of Urologists. Governing body. Plenum: Materials. Kirov, 2000: 105-106.
- Gakiya M. Spontaneous rupture of infected renal cyst: a case report // Hinyokika-Kiyo. 2000; 46 (4): 265-267.
- Kaim AH, Burger C., Canter CC, Goerres GW PET-CT guided percutaneous puncture of an infected cyst in autosomal dominant polycystic kidney disease: case report // Radiology. 2001; 221(3):818-821.
- Ueno Y., Hosaka K., Takesaki T. A case of infected renal cyst extending to leg abscess // Hinyokika-Kiyo. 2000; 46 (2): 105-107.
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
FAQ
How is hematuria diagnosed?
Blood in the urine is detected during a general urine test. Since it does not represent a ready-made diagnosis, the causes of hematuria need to be further clarified.
Is hematuria dangerous?
Blood in the urine may be a sign of life-threatening diseases, such as acute glomerulonephritis or kidney cancer. Therefore, the doctor will definitely prescribe additional tests that will help in making a diagnosis.
How does pediatric hematuria differ from adult hematuria?
It is not the phenomenon itself that is different, but its possible causes. Chronic hematuria that occurs in a young child leads the doctor to believe that the cause may be a congenital pathology. However, its risk is minimal: in most cases, blood in the urine in both children and adults is associated with infectious diseases of the kidneys, bladder and urethra.
Kidney failure
Pyelonephritis
Diabetes
6584 07 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Kidney failure: causes, symptoms, diagnosis and treatment methods.
Definition
Kidney failure is a condition in which one or both kidneys cannot fully perform their functions. This occurs as a result of some disease when the kidneys stop fully filtering the blood. Substances that should be eliminated from the body end up back into the bloodstream. Impaired kidney function may be associated with a decrease in blood flow through them and a sharp decrease in oxygen supply.
The main function of the kidneys is excretory, that is, cleansing the body of waste and toxins, while the kidneys are responsible for maximum preservation of nutrients.
The kidneys take part in phosphorus-calcium metabolism and the formation of bone tissue by producing calcitriol (the active form of vitamin D), so in children, kidney failure negatively affects bone growth and abnormal development, and in adults it can cause fragility.
The kidneys regulate blood pressure, so kidney failure causes it to rise.
The kidneys are involved in the formation of red blood cells - erythrocytes. With kidney failure, the number of red blood cells decreases and anemia develops.
The kidneys regulate the amount of water and salts - maintaining the water-salt balance.
Causes of kidney failure
There are many reasons for the development of kidney failure. Some lead to a rapid deterioration of kidney function, most often of ischemic or toxic origin (acute kidney injury, or acute renal failure). Others lead to a gradual deterioration of kidney function (chronic kidney disease, or chronic renal failure). In addition to the inability of the kidney tissue to filter the body's metabolic waste products (particularly creatinine and urea nitrogen) from the blood, the kidneys' ability to control the amount and distribution of water in the body (fluid balance) and the level of electrolytes in the blood is reduced. Acute kidney injury is a sudden decline in kidney function over several days or weeks, causing a buildup of nitrogenous compounds in the blood (azotemia). Causes of renal failure in the acute form of the disease:
- acute disturbances of renal hemodynamics (collapse, shock);
- intoxications of various origins (medicinal, insect and snake bites, household poisons);
- acute infectious kidney damage;
- acute inflammatory kidney diseases (pyelonephritis, acute glomerulonephritis);
- injury to the kidney or other organ with large blood loss;
- urinary tract obstruction;
- kidney removal.
Among all the causes of chronic renal failure, a special place is occupied by diseases that affect the renal glomeruli:
- renal diseases - chronic pyelonephritis and glomerulonephritis;
- metabolic diseases: amyloidosis, gout, diabetes;
- congenital renal diseases: narrowing of the renal arteries, underdevelopment of the kidneys, polycystic disease;
- rheumatic diseases: hemorrhagic vasculitis, scleroderma, systemic lupus erythematosus;
- serious disorders of the cardiovascular system: arterial hypertension and diseases leading to significant changes in renal blood flow (heart failure, arrhythmia);
- diseases that cause problems with the outflow of urine.
Acute renal failure is always a consequence of other pathological processes in the body.
If you immediately pay attention to its symptoms and take action, it is possible to completely restore the function of the affected kidney. In chronic renal failure, the kidneys are damaged irreversibly. In some cases, kidney failure in women can develop during pregnancy.
Although decline in kidney function is possible at any age, chronic kidney failure and acute kidney injury are more common in older adults. Many diseases that cause deterioration of kidney function can be treated to restore kidney function. Thanks to the availability of dialysis and kidney transplantation, kidney failure has become a manageable disease rather than a fatal one.
Classification of the disease
The International Classification of Diseases (ICD) 10 has been amended to replace the outdated term “chronic renal failure” with the term “chronic kidney disease” (code N18).
Modern classification is based on two indicators - glomerular filtration rate and signs of renal damage (proteinuria, albuminuria). Depending on their combination, there are five stages of chronic kidney disease.
The immediate causes of acute renal failure (code N17) are low blood flow velocity, acute destruction of the glomerulus with loss of afferent and efferent arteries and glomerular capillaries, damage to nephron tubules, or impaired outflow of urine from the kidney due to obstruction. Depending on this, there are three forms of acute renal failure:
- prerenal (70%),
- parenchymal (25%),
- obstructive (5%).
Symptoms of kidney failure
Kidney failure has the following main symptoms:
- decreased amount of urine excreted, urination disorder (oliguria, dysuria);
- swelling;
- general lethargy, drowsiness;
- nausea, vomiting, loss of appetite;
- tachycardia, increased blood pressure;
- bloating, loose stools.
Since in renal failure the kidneys do not perform their main - excretory - function, metabolism is disrupted.
Often the dominant symptoms of acute renal failure are manifestations of the underlying disease or symptoms caused by surgical complications of an operation that led to impaired renal function.
Chronic renal failure is characterized by an asymptomatic onset of the disease. At this stage, patients often do not complain; in extreme cases, they report increased fatigue with moderate physical activity, as well as dry mouth and weakness, which manifests itself in the late afternoon. Further attention is drawn to pale skin and flabby muscles that lose tone. Based on the results of a biochemical blood test, patients are often informed about the presence of protein in the urine and minor changes in the electrolyte composition of the blood.
The severity of symptoms depends on the stage of chronic kidney disease. The disease has an undulating course: the patient’s condition either improves or worsens again.
The terminal stage of chronic kidney disease is extremely dangerous, when the patient’s emotional reactions are disrupted (apathy sharply turns into excitement, night sleep is disturbed, and signs of lethargy appear). There is an ammonia odor from the mouth, swelling, the face becomes puffy, yellowish in color, traces of scratching are visible on the skin, the hair becomes dull, brittle, and dystrophy increases. Symptoms of uremic intoxication increase: ascites, pleurisy, pericarditis, uremic coma. Severe arterial hypertension often occurs.
Diagnosis of kidney failure
To diagnose renal failure, the following examinations are prescribed:
- general (clinical) blood test;