Briefly about the treatment method
The use of percutaneous coronary intervention (PCI) as an emergency treatment for myocardial infarction is urgent.
The goal of primary PCI is to open the artery as quickly as possible, preferably within 90 minutes. The treatment method is very effective, often without complications, but, unfortunately, not everywhere patients have the opportunity to seek help on time or get to the hospital on time. Another type of emergency surgery for myocardial infarction is coronary artery bypass grafting (CABG), which is usually performed to simultaneously treat mechanical complications such as papillary muscle rupture or ventricular septal defect accompanied by cardiogenic shock. In uncomplicated MI, mortality can be high when surgery is performed immediately after the infarction.
Rubric “Conversation with a specialist” Acute myocardial infarction - symptoms and first aid
The joint article was prepared by three specialists at once - cardiologist, anesthesiologist-resuscitator of Health Academy LLC Konstantin Nikolaevich Bozhesku, functional diagnostics specialist of Health Academy LLC (formerly an employee of the Nizhny Tagil emergency medical service team), Gennady Andreevich Puzanov and paramedic of the highest category of the team intensive care of the State Budgetary Healthcare Institution SO "City Emergency Medical Care Station of Nizhny Tagil" by Dmitry Vasilievich Subbotin.
Timely pre-medical and emergency medical care during an attack of myocardial infarction in most cases is the key to the patient’s successful recovery. It is the absence of such activities that often becomes the cause of death even for young people who have encountered this acute cardiac pathology. Cardiologists recommend that all patients with coronary artery disease know the first signs of myocardial infarction and the rules for providing first aid. It is also important to know what treatment the patient will be prescribed in the hospital in order to prepare for a conversation with the attending physician and ask him the necessary and important questions.
When is it necessary to start performing first aid? The answer to this question is always clear – immediately. That is, already when the patient began to show the first signs of myocardial infarction. Its onset is signaled by the following typical symptoms:
intense chest pain; irradiation of pain to the left arm, shoulder blade, teeth or neck area; severe weakness; fear of death and severe anxiety; cold clammy sweat; nausea. With atypical forms of heart attack, the patient may experience other symptoms:
stomach ache; digestive disorders; vomit; dyspnea; suffocation, etc. First aid in such situations should begin with calling an ambulance. When talking with the dispatcher of this service, you must:
report the symptoms observed in the patient; express your assumption about the possibility of myocardial infarction; ask to send a team of cardiologists or resuscitators. After this, you can begin to carry out those activities that can be performed outside the medical institution.
First aid The patient must be carefully placed on his back and given the most comfortable position (semi-sitting or a cushion placed under the back of his head).
Ensure a flow of fresh air and the most comfortable temperature conditions. Remove clothing that interferes with free breathing (tie, belt, etc.).
Convince the patient to remain calm (especially if the patient exhibits signs of motor agitation). Talk to the victim in a calm and even tone, do not panic or make sudden movements.
Give the patient a Nitroglycerin tablet under the tongue and a sedative (Corvalol, motherwort tincture or valerian).
Measure blood pressure. If the pressure is not more than 130 mm. rt. Art., then it is advisable to re-take Nitroglycerin every five minutes. Before the doctors arrive, you can give 2-3 tablets of this drug. If the first dose of Nitroglycerin caused a severe throbbing headache, then the dosage should be reduced to ½ tablet. When using this drug in the form of a spray, its single dose should be 0.4 mg. If the patient's first dose of Nitroglycerin caused a sharp decrease in blood pressure, then this drug should not be used further.
Give the patient a crushed Aspirin tablet (to thin the blood).
Count the patient's pulse. If the heart rate is no more than 70 beats/minute and the patient does not suffer from bronchial asthma, then he can be given one of the beta blockers (for example, Atenolol 25-50 mg).
You can put a mustard plaster on the area where the pain is located (remember to keep an eye on it so that there is no burn).
During the provision of first aid, the patient’s condition may be complicated by the following conditions:
fainting; heart failure. If fainting occurs, it is necessary to remain calm and ensure the normal functioning of the respiratory system. The patient must be placed in a horizontal position, a cushion placed under his shoulders and dentures (if any) removed from the mouth. The patient's head should be in a tilted position, and if there are signs of vomiting, it should be turned to the side.
In case of cardiac arrest, artificial respiration and chest compressions must be performed before the medical team arrives. The frequency of compressions on the midline of the chest (heart area) should be 75-80 per minute, and the frequency of blowing air into the airways (mouth or nose) should be about 2 breaths every 30 compressions on the chest.
Emergency medical care and principles of treatment in a hospital Emergency medical care for myocardial infarction begins with the relief of acute pain. For this, various analgesics (Analgin) and narcotic drugs (Promedol, Morphine, Omnopon) in combination with Atropine and antihistamines (Diphenhydramine, Pipolfen, etc.) can be used. For a faster effect, painkillers are administered intravenously. Seduxen or Relanium is also used to eliminate the patient's anxiety.
Then, to assess the severity of the heart attack, the patient is given an electrocardiogram. If hospitalization is possible within half an hour, the patient is immediately transported to a medical facility. If it is impossible to transport the patient to the hospital within 30 minutes, thrombolytics (Alteplase, Purolase, Tenecteplase) are administered to restore coronary blood flow.
A stretcher is used to transfer the patient to the ambulance, and during transportation to the intensive care unit, humidified oxygen is inhaled. All these measures are aimed at reducing the load on the heart muscle and preventing complications.
After arrival at the intensive care unit, to eliminate pain and agitation, the patient is given neuroleptanalgesia with Talamonal or a mixture of Fentanyl and Droperidol. In case of a prolonged angioedema attack, the patient can be given inhalation anesthesia using a gaseous mixture of nitrous oxide and oxygen.
Next, the patient is prescribed the following medications:
Nitroglycerin, Isosorbide dinitrate, Isoket - in the acute period of a heart attack, these drugs are used to reduce the myocardial oxygen demand, first they are administered intravenously, and after stabilizing the patient's condition - orally and sublingually.
Beta blockers (Anaprilin, Inderal, Obzidan, Propranolol) - help slow the heart rate and reduce the load on the heart.
Antiplatelet agents (Aspirin) thin the blood and prevent the development of a new heart attack.
Anticoagulants (Heparin) - used to prevent recurrent heart attacks and reduce blood clotting.
ACE inhibitors (Ramipril, Captopril, Enalapril, etc.) are used to lower blood pressure and reduce the load on the heart.
Sedative and hypnotic drugs (Diazepam, Oxazepam, Triazolam, Temazepam, etc.) are used when it is necessary to limit the patient’s activity and for sleep disorders.
Antiarrhythmic drugs (Novocainamide, Rytmilen, Lidocaine, Difenin, Amiodarone, etc.) are used for cardiac arrhythmias to stabilize cardiac activity and reduce the load on the myocardium.
Other pharmacological drugs can be used to treat myocardial infarction, since the tactics of drug treatment of the patient depends on the general condition of the patient and the presence of other pathologies (diseases of the kidneys, blood vessels, liver, etc.).
Also, for the treatment of myocardial infarction, modern medicine uses various instrumental, highly effective techniques to restore coronary blood flow:
balloon angioplasty; coronary artery bypass grafting. Such surgical techniques allow patients with severe forms of myocardial infarction to avoid serious complications and prevent the high risk of mortality from this cardiac pathology.
Motor activity of a patient with myocardial infarction All patients with myocardial infarction are advised to limit their physical activity, since this regime contributes to a more rapid replacement of the infarction area with scar tissue. In the first days, the patient must observe strict bed rest, and from 2-3 days, in the absence of complications and signs of heart failure, his motor regimen begins to gradually expand. Initially, he is allowed to sit on a bedside chair 1-2 times a day and sit on it for about 15-30 minutes (the frequency and duration of these actions is determined by the doctor).
These days the patient can eat on his own. He also needs to be washed and cleaned, and he must use a bedpan to defecate (the use of a bedside toilet seat is permissible only with the permission of a doctor and only for patients with a stable heart rhythm).
Starting from 3-4 days, the patient is allowed to sit on a chair for about 30-60 minutes twice a day. In case of an uncomplicated heart attack, the patient is allowed to start walking between 3-5 days (this time is determined by the doctor). The time of such walking and the distances over which the patient moves increase gradually.
In an uncomplicated form of myocardial infarction, the patient is discharged from the hospital on days 7-12, and in complicated cases it can take place only after 3 weeks or more. In the future, the patient must undergo a course of rehabilitation, which can be performed in specialized institutions or at home. During this period, the intensity and duration of physical activity gradually increases depending on health indicators.
Nutrition of the patient during myocardial infarction In the first week after myocardial infarction, the patient is recommended to have a low-calorie diet with limited salt, animal fats, liquids, foods with nitrogenous substances, excessively coarse fiber and cholesterol. The diet should include foods that are rich in lipotropic substances, vitamin C and potassium salts.
In the first 7-8 days, all dishes should be pureed. Food is taken in small portions 6-7 times a day.
The diet may include the following foods and dishes:
wheat bread crackers; semolina, oatmeal, buckwheat and rice cereals; lean veal; low-fat varieties of fish; chicken meat; protein steam omelette; low-fat cheese; fermented milk drinks; butter; salad of fresh grated carrots and apples; vegetable soups; boiled beets and cauliflower; pureed fruit; compotes and fruit drinks; rosehip decoction; weak tea; honey. During this period, the following foods and dishes are prohibited:
dough products (pancakes, donuts, cakes, pies); smoked and marinated dishes; pickles; fried foods; sausages; fatty dairy products; salty and spicy cheeses; caviar; fat meat; boiled and fried eggs; fish and mushroom broths; pasta; cooking fat; mushrooms; legumes; sorrel; turnip; grape; tomato juice; spices; chocolate; natural coffe. 2-3 weeks after a heart attack, the patient is recommended the same set of products and list of restrictions, but the food may no longer be pureed, prepared without adding salt and taken about 5 times a day. Subsequently, the patient's diet expands.
Remember! Myocardial infarction is a serious and dangerous pathology that can cause many serious complications and even death of the patient. Be sure to follow all the rules for providing first aid during an attack of this acute condition, call an ambulance in a timely manner and follow all the doctor’s recommendations during treatment in a hospital.
You can make an appointment with a cardiologist, as well as undergo an electrocardiogram at our Medical Center. Make an appointment by phone 8(3435) 230-500
We care about you!
Always yours, Medical
Indications and contraindications for the treatment method
Indications for stenting are:
- Myocardial infarction with ST segment elevation.
- Unstable angina and myocardial infarction without ST segment elevation.
- Stable ischemic heart disease.
There are no absolute contraindications to stenting of coronary arteries. The main contraindication is the impossibility of prescribing antiplatelet therapy.
Relative contraindications: acute renal failure, chronic renal failure, ongoing gastrointestinal bleeding, fever of unknown origin, possibly infectious, untreated active infectious process, acute stroke, severe anemia, malignant uncontrolled arterial hypertension, severe electrolyte disturbances, lack of contact with the patient due to with a psychological condition or serious illness, severe concomitant pathology in which coronary angiography can complicate the course of the disease, patient refusal of necessary further treatment (coronary angioplasty, coronary artery bypass grafting, valve replacement), digitalis intoxication, documented anaphylactic reaction to a contrast agent, severe illness peripheral vessels, impeding access to the vascular bed, decompensated congestive heart failure or pulmonary edema, severe coagulopathy, aortic valve endocarditis.
2.Angioplasty and surgical treatment of heart attack
Angioplasty is often done immediately after a heart attack.
. For unstable angina, especially if the risk of a heart attack is quite high, it also makes sense to have angioplasty.
Angioplasty opens a coronary artery that was narrowed or blocked during a heart attack, allowing blood to flow freely to the heart. Before angioplasty, cardiac catheterization
, during which the doctor will check the condition of the coronary arteries and determine the need and advisability of angioplasty. It is worth knowing that not all medical institutions can perform this operation, and the ambulance will not always take the patient to the exact clinic where this opportunity is available. Therefore, in the case of a heart attack or stroke, it makes sense to turn to paid hospitalization to be sure that medical care will be provided at the highest level.
Visit our Cardiology page
How the treatment method works
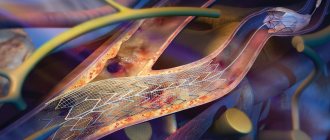
Coronary artery stenting for myocardial infarction includes the following steps:
- A stent is inserted into the narrowing of the coronary artery using a special balloon catheter. A stent is a stainless metal tube with many cells of various configurations.
- When the balloon is inflated, the stent expands in diameter and is pressed tightly into the artery wall, increasing the lumen of the narrowed vessel, which allows blood to flow freely to the heart.
- The balloon is deflated and removed, while the stent remains permanently in place at the site of narrowing or blockage.
Coronary artery bypass grafting is performed on an open heart. The idea is to create a bypass (shunt) from the aorta to the coronary artery, bypassing the site of blockage or narrowing. Usually the material for the shunt is the person’s own vein; sometimes it is necessary to use artificial material. Your attending physician will tell you in more detail about the stages of coronary artery bypass surgery itself.
Observation program after treatment method
Cardiac rehabilitation aims to optimize function and quality of life in those suffering from heart failure. Exercise is an important part of rehabilitation after a myocardial infarction, which has beneficial effects on cholesterol levels, blood pressure, weight, stress and mood. Some patients are afraid of exercise because it can cause another heart attack. But you need to understand that the doctor, upon discharge, indicates the required dosed physical activity. The risk of another heart attack is reduced with strict blood pressure control and lifestyle changes, mainly smoking cessation, regular exercise, a sensible diet for heart disease patients, and limiting alcohol consumption. Drugs are typically prescribed after a myocardial infarction to prevent secondary cardiovascular events, such as further myocardial infarctions, congestive heart failure, or cerebrovascular disease.
Causes
As a rule, the cause of a heart attack is the following diseases:
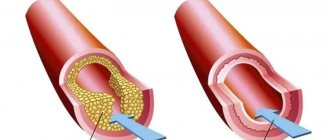
- atherosclerosis - cholesterol plaques that narrow the lumen of the coronary artery, limit the flow of blood to the heart muscle;
- increased blood clotting, which can lead to blockage of a heart vessel - the coronary artery,
- angina - before a heart attack, approximately half of people experience angina attacks during physical activity, which quickly go away when the activity stops. Therefore, a patient with angina pectoris should be under the supervision of a cardiologist to prevent the development of myocardial infarction.
The development of the disease is promoted by: diabetes mellitus, hypertension, obesity, psycho-emotional stress, alcohol consumption, smoking.