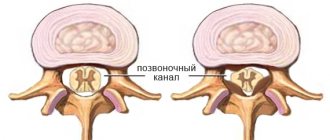
Stenting of the carotid arteries is an effective minimally invasive method for preventing ischemic stroke in atherosclerosis and stenosis. If a patient has a narrowing of the carotid sinus of more than 70% in area, then the risk of stroke is about 10% per year. In cases of previous cerebrovascular accidents, the risk of major stroke increases to 50% per year.
Stenting has a number of advantages over carotid endarterectomy, since it does not require surgical access, is performed under local anesthesia and can be used in weakened patients. The main vessels supplying the brain and neck are the two common carotid arteries. They rise up the neck, where each divides into two branches, the external carotid, which supplies blood to the skin and soft tissues of the head, and the internal carotid (ICA), which supplies blood to the brain. Damage to these vessels by atherosclerosis is the cause of most ischemic strokes.
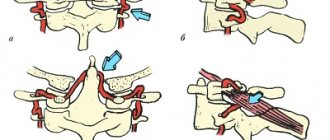
Carotid artery stenting involves an operation to expand the narrowed vessel from the inside with a special balloon and strengthen the wall with a metal mesh (stent). To prevent complications associated with the entry of pieces of plaque into the brain during angioplasty, an intravascular filter is used, located above the site of the atherosclerotic plaque. This operation is performed without incisions, through a puncture in the leg or arm.
Advantages of carotid artery stenting at the Innovative Vascular Center
Our clinic has extensive experience in treating patients with carotid artery pathology. In recent years, stenting has almost replaced open carotid endarterectomy in our practice, as we have become convinced that this method has undeniable advantages and is suitable for most cases.
We perform stenting of the internal carotid artery after assessing the intracerebral vascular bed in order to eliminate the risk of stroke as much as possible. The price for carotid artery stenting in our clinic is affordable, although a disposable instrument is used to perform the operation in our clinic - a recognized world leader in the development of peripheral endovascular products.
During the use of carotid artery stenting in our clinic, we have not noted a single case of serious complications (stroke, bleeding, thrombosis). The clinic’s vascular surgeons have a differentiated approach to the choice of method for restoring arterial patency. We try to perform open endarterectomy in young patients, and ICA stenting in older patients.
What should I change in my diet?
The basic principles of diet therapy for atherosclerosis can be formulated as follows:
DECREASE:
- total fat intake
- consumption of saturated fatty acids (butter, animal fats)
- eating foods rich in cholesterol
- salt consumption (up to 3-5 g per day)
INCREASE:
- consumption of fiber and complex carbohydrates (vegetables and fruits).
- consumption of foods containing polyunsaturated fatty acids (fish, seafood, liquid vegetable oil)
6. HYPOCHOLESTEROL (HYPOLIPIDEMICA) DIET
The principle of the diet is to significantly reduce the consumption of cholesterol and easily digestible carbohydrates, and for overweight patients, a significant reduction in calorie intake
This diet is general in nature; if there are various variants of lipid metabolism disorders, the attending physician makes appropriate adjustments. It is very important to avoid eating after 19:00, and dinner should consist entirely of foods containing a large amount of fiber and absolutely no cholesterol (vegetables, fruits).
I.N E L Z
Consume foods containing large amounts of saturated fat. These include the following:
- Milk and dairy products (condensed milk, cream, sour cream, butter, cheese, cottage cheese, kefir, curdled milk, yogurt, ice cream, milkshake), as well as milk porridge.
- Pork and cooking fat, margarines, coconut and palm oil.
- Pork, lamb (respectively ham, bacon, brisket, ham, carb, neck), lard and, accordingly, those products in which they can be included (smoked and boiled sausages, frankfurters, sausages, cutlets, steaks, meatballs, canned meat, meat in jelly), fatty meat broths.
- Liver (respectively pate) and other offal (kidneys, lungs, brains).
- Red poultry meat, leather.
- Sturgeon, fish spark, fish liver, crayfish, crabs, shrimp, shellfish.
- Eggs (respectively mayonnaise).
- High quality bread and crackers made from it, confectionery products (cakes, cookies, pastries, biscuits), because they contain milk, eggs, sugar.
- Pasta.
- Cocoa, chocolate, coffee beans.
- Sugar, honey
- Cold drinks: sweet carbonated drinks (Fanta, Pepsi, etc.)
- Alcoholic drinks: beer, sweet fortified wines, liqueurs.
II . CAN
Consume the following products in moderation (no more than 2 times a week, or more often, but in limited quantities as prescribed by your doctor):
- White poultry meat without skin, lean beef. The preferred cooking method is boiling, grilling, microwave processing; undesirable cooking method - stewing, frying.
- Secondary broth from lean beef and lean chicken (a portion of meat is boiled in water a second time, the first broth is drained).
- River fish, incl. red.
- Bread made from bran and rye flour, crackers made from it.
- Buckwheat (cook in water without adding oil).
- Potatoes soaked in water, peeled, for an hour. The preferred method of preparation is boiling. Light frying in vegetable oil is allowed.
- Mushrooms.
- Ketchup (not sweet), mustard, soy sauce, tkemali sauce, adjika, vinegar, spices, herbs.
- Tea, instant coffee without sugar.
- Chewing gum without sugar.
- Walnuts, almonds, hazelnuts.
- Alcoholic drinks: vodka, cognac, whiskey, tequila, dry wine.
III . NEED TO
Eat the following foods daily in large quantities:
- Vegetable oil (sunflower, corn, salad, olive, soybean, rapeseed, cottonseed).
- All vegetables (fresh, frozen, canned without sugar, dried fruits) with peel: carrots, beets, cabbage, turnips, radishes, radishes, zucchini, squash, eggplant, tomatoes, cucumbers, cauliflower, peas, beans, soybeans, corn. When preparing a vinaigrette, the vegetable oil should not be excessive (i.e., remain at the bottom of the dish). Cold vegetarian borscht is healthy.
- All fruits and berries with peel.
- Onions, garlic, herbs (parsley, celery, cilantro, basil, lettuce, spinach, wild garlic, sorrel, etc.).
- Sea fish (cod, hake, navaga, ice fish, haddock, sprat), incl. fatty (halibut, herring, tuna, sardine). Method of preparation: boiling, baking, frying in vegetable oil, under marinade.
- Sea kale.
- Oatmeal (from unrefined oatmeal or “Hercules”), boiled in water.
- Cold drinks: mineral water, fruit water, fruit juice and fruit drink without sugar.
Preparing for the intervention
- Before the operation of carotid artery stenting, the patient must undergo a number of mandatory examinations:
- Clinical blood and urine tests
- Biochemical blood test (urea, creatinine, electrolytes)
- X-ray of the lungs
- ECG
- Echocardiography
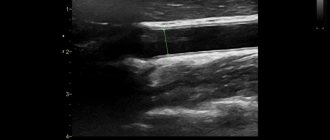
- Ultrasound of the carotid arteries and transcranial Dopplerography
- Multislice computed tomography of the vessels of the neck and brain
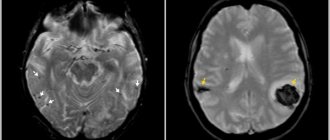
- MRI of the brain
- Consultation with a neurologist
- One day before stenting, all patients receive combination antiplatelet therapy with 300 mg of Plavix. Immediately before the intervention on the vessel, heparin is administered intravenously.
Risk factors
Factors that affect arteries and increase the risk of damage, plaque formation, and disease include:
- High blood pressure.
High blood pressure is the most important factor in the development of atherosclerotic lesions of the carotid arteries. Exposing the artery wall to high pressure weakens it and makes it more susceptible to damage. - Smoking.
Nicotine irritates the inner lining of blood vessels, and also increases heart rate and increases blood pressure. - Age.
With age, the arterial wall loses elasticity and becomes more susceptible to damage. - Violation of the blood lipid ratio.
Elevated levels of low-density lipoprotein cholesterol ("bad cholesterol") and high levels of triglycerides contribute to the formation of atherosclerotic plaques. - Diabetes.
Diabetes not only affects the ability to control blood sugar levels, but also lipid metabolism, increasing the risk of hypertension and the development of atherosclerosis. - Obesity.
Excess body weight increases the risk of arterial hypertension, atherosclerosis and diabetes. - Heredity.
The presence of atherosclerosis or coronary heart disease in relatives significantly increases the risk of developing atherosclerotic lesions. - Sedentary lifestyle.
Lack of physical activity contributes to the development of hypertension, obesity and diabetes.
Often, the listed risk factors are present in combination, thereby increasing the degree of risk.
Pain relief during stenting
The intervention is performed under local anesthesia using light sedatives, since it is necessary to assess the patient’s neurological status during stenting. When the balloon is inflated, the patient may experience a slow heart rate (bradycardia) and a decrease in blood pressure (hypotension), so continuous monitoring of cardiac activity during surgery is necessary.
The patient lies on his back, with his arm abducted, on which a blood pressure cuff is attached. The electrodes of the device for taking a cardiogram are glued to the chest. The surgical field is processed and the patient is covered with a sterile sheet.
Answers to your questions
- Question: How can I check that my prosthesis is working correctly?
Answer: After implantation of the prosthesis, the symptoms and signs that preceded surgical treatment will become significantly less and, in many cases, completely disappear. If symptoms and signs do not return or worsen, it is safe to say that the prosthesis is working normally.
- Question: What will happen to my vascular system if the prosthesis stops working properly?
Answer: The organ or tissue supplied by this prosthesis will gradually or suddenly receive less blood. In this case, typical symptoms and signs (depending on the area where the prosthesis is located) will develop. For example, increased pain when walking or decreased walking distance without pain, or cold feet.
- Question: How often does my vascular graft need to be replaced?
Answer: Your prosthesis was designed to last indefinitely. But as mentioned above, in some cases the operation of the prosthesis may be disrupted. If this happens, you will need to replace the prosthesis, but the decision is made individually in each specific case. There is a small risk that the prosthesis may become infected. We guarantee that when the prosthesis is implanted, it is absolutely sterile. The operation is also carried out under conditions of the greatest possible and strictest sterility. In very rare cases, infection can still spread to the prosthesis from your skin or from the air in the operating room. This may have no effect, but if the prosthesis becomes infected, it should be removed.
- Question: Can the prosthesis be affected by external energy influences, such as running engines, microwave ovens, airport security checks, sunbathing, etc.?
Answer: No
- Question: Should I reduce my activity level?
Answer: Only your attending physician can decide the level of individual restrictions. He knows your health condition and the location of the prosthesis. After implantation of a vascular prosthesis, as a rule, the patient can return to a completely normal and active life. However, when implanting a prosthesis, your doctor may restrict you from certain activities, such as sports, lifting weights, or gardening, until the prosthesis is fully integrated into the vascular system.
- Question: Should I limit my walking?
Answer: Dosed walking is not harmful, but even beneficial. Physical activity on the legs will prevent atrophy (reduction in volume) of the muscles through which small arteries pass. The greater the muscle mass, the more blood vessels will form. Set a walking rhythm for yourself (for example, 60 steps per minute) and try to walk a certain distance every day. Walk until pain appears in your leg muscles. There is no need to walk while overcoming the pain - the pain causes a spasm of the arteries. Record in the table the number of steps that you managed to walk without pain, and you will see that it gradually increases.
- Question: Can I smoke?
Answer: You should not smoke. It has been irrefutably proven that smoking has a negative impact on the long-term results of the vascular prosthesis, as well as on the condition of your own arteries in general.
- Question: Can I stop taking my medications for a while?
Answer: Some drugs used in the treatment of atherosclerosis are taken in courses of 2-3 months, others - continuously. Only your attending physician can decide in what dosage and according to what scheme they should be used. In some cases (for example, during an upcoming surgery), it is advisable to stop taking certain medications for a while or replace them with others. In any case, inform your attending physician about your illness and the medications you are taking.
- Question: How about reducing my sexual activity?
Answer: Only if the doctor recommends that you reduce sexual activity. In all other cases there is no need for any restrictions.
- Question: Can I continue to drive my car?
Answer: In most cases, yes. But you should always consult your doctor.
- Question: If I develop an infection or have surgery, do I need to take special precautions?
Answer: It has been proven that even with such ordinary manipulations as dental treatment, a temporary release of microbes into the blood can occur. If these agents come into contact with the prosthesis, it may become infected. Therefore, if you have an infectious disease, if you are undergoing a minor operation, for example, treatment or tooth extraction, cystoscopy, fibrogastroscopy or intestinal examination, you should definitely consult your doctor about taking antibiotics.
Complications during stenting
- Transient cerebrovascular accidents
Transient ischemic attacks occur in 0.5% of patients during or immediately after carotid artery stenting. May be associated with tiny pieces of plaque entering the brain as the conductor passes through the narrowed area. These may be transient visual or speech disturbances, weakness in an arm or leg, which disappear within the next 3 hours after the intervention.
- Ischemic stroke
The development of stroke, according to the literature, occurred in 1% of patients after stenting, but in recent years, due to the advent of new technologies for protecting the brain, this complication is much less common.
- Reflex bradycardia and hypotension
These phenomena are associated with the effect of the balloon on the vagus nerve passing next to the carotid artery. They manifest themselves as a decrease in heart rate and a drop in blood pressure. With a timely response from the anesthesiologist, this complication is quickly relieved with medications.
- Bleeding from the puncture site
A rare complication, accompanied by the formation of a tense hematoma in the area of access to the vessel. Sometimes open surgery may be necessary to stop bleeding.
Causes of the disease
The exact causes of primary arteritis have not yet been identified. Scientists were able to find out that certain groups of bacteria and viruses . a hereditary factor cannot be ruled out , since several cases of morbidity are often detected in one family.
Other causes of inflammation of the arteries include taking certain medications, as well as the immune reactivity of the human body.
The process of disease development begins with immune inflammation of the arterial wall. The inflammatory process occurs due to the formation of autoantibodies and immune complexes in the blood, deposited on the walls of blood vessels. Affected cells release inflammatory mediators, which leads to the formation of inflammatory foci.
Postoperative period
The patient is discharged on the 2nd day after surgery with a mandatory follow-up ultrasound scan.
After carotid artery stenting, combination antiplatelet therapy with clopidogrel 75 mg/day and aspirin 100 mg/day is prescribed for up to 12 months. Subsequently, aspirin and anti-cholesterol drugs - statins remain.
A control ultrasound scan is performed one month after stenting surgery. The patency of stented segments should be assessed at intervals of 6 months. If signs of restenosis are detected, the patient is prescribed a multislice computed tomography scan with contrast.