© Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
Leriche syndrome is a chronic disease in which a narrowing or complete closure of the lumen of the arteries of the legs occurs with impaired circulation. Typically, the pathology is diagnosed in men aged 40-60 years, but in recent years there has been some “rejuvenation” of the group of patients.
The disease is quite dangerous, because it leads to disability in relatively young people, is fraught with fatal complications, and often requires serious surgical treatment. After atherosclerosis of the vessels of the heart and brain, damage to the arteries of the legs takes third place, being detected in almost every fifth patient with atherosclerosis after 50-55 years. In the case of major amputation of a limb, approximately half of the patients are at risk of dying within a year after surgery.
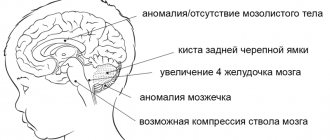
The aorta is the largest vessel in the human body, providing blood to all organs and tissues. In the lower section, it is divided into the right and left iliac arteries, which supply blood to the lower extremities. In Leriche syndrome, the substrate of the disease becomes the lower fragment of the aorta after the renal arteries and iliac vessels depart from it.
Leriche's syndrome. Treatment
Leriche syndrome is a disorder of blood flow in the lower extremities, which occurs when there is severe narrowing or complete blockage of the abdominal aorta at the site of its bifurcation into the iliac arteries. Until recently, the pathology was most often diagnosed in men aged 40-60 years. But doctors warn that she has recently become much younger and her problem is acute even in men aged 30-35 years. Not everyone knows about the existence of such a disease, so doctors often hear the question: “What is Leriche syndrome and what are the chances of getting it?” Answers to questions are in this article.
Causes of the disease
Leriche syndrome (another name is aortic atherosclerosis) can be caused by:
- congenital pathologies of the aorta;
- thrombosis;
- nonspecific aortoarteritis;
- blockage of blood vessels;
- atherosclerotic changes in blood vessels;
- dysplasia of the fibromuscular layers of blood vessels.
The causes of atherosclerosis have long been known, these are:
- unhealthy diet (lots of fatty foods, fast food);
- lack of sleep;
- poor lifestyle in general.
Fatty foods have a detrimental effect on the body of the elderly and older people, since their metabolism is slowed down and fats settle on the walls of blood vessels, which leads to atherosclerosis.
Symptoms and diagnosis of Leriche syndrome
The main signs of the described disease are:
- intermittent lameness;
- problems with potency;
- absence of pulse in the arteries of the lower extremities.
Intermittent claudication is the main symptom of Leriche syndrome. Patients may also experience severe pain in the lower back and buttocks, hips, calf muscles and ankle joints when walking.
Doctors diagnose Leriche syndrome using research methods such as:
- ultrasound examination of the vessels of the lower extremities;
- MRI of the lower extremities;
- contrast angiography.
Main signs of pathology
How serious the general deviations in the functioning of the body's systems will be is determined by the length of the section of the vessel that is subject to obstruction (blockage) and poorly supplies the tissue with the necessary substances.
Symptoms of Leriche syndrome do not appear immediately after the initial vascular lesion. They develop as a larger portion of the artery further obliterates. Until thrombosis begins, the patient feels signs of the disease only after significant physical exertion, and therefore may not pay attention to them for a long time. At rest, symptoms appear gradually and increase slowly.
The pathology begins with a drop in pressure in remotely located vessels, and as a result, blood microcirculation deteriorates. As the syndrome develops, metabolic processes in tissues are disrupted.
The symptoms of the disease are as follows:
1. Pain in the lower extremities, which manifests itself when walking a certain distance. Patients are concerned about discomfort in the lower leg, thigh, buttocks and lower back. This is due to the development of ischemia. The so-called intermittent claudication occurs, and depending on its severity and the distance the patient can cover painlessly, they are classified according to degrees:
- I degree. This stage is the stage of functional compensation, that is, recovery is still underway. There is increased general fatigue, convulsive phenomena, and discomfort in the lower extremities (tingling, numbness). Patients complain that their feet are cold for no reason. Pain that forces a person to stop until it goes away occurs when walking a distance of half a kilometer to a kilometer (at an average pace).
- II degree. The stage of subcompensation, in which patients already regard symptoms as a problem and often already seek medical help. The distance covered before painful sensations appear is about two hundred meters. Hair falls out on the affected leg and its growth is impaired. The skin becomes dry and peeling is observed. Nails become brittle and their growth rate is significantly reduced. Subcutaneous fatty tissue and foot muscles become depleted and cease to perform their functions.
- III degree. Decompensation manifests itself in constant pain: even at rest, the patient is bothered by the lower leg and thigh. The distance a person can walk is reduced to thirty meters. The skin becomes thin and easily vulnerable, minor scratches lead to the appearance of ulcers and cracks. The color of the skin on the affected limb changes depending on its position above the level of the body: when lowered, the leg turns red, when raised, it turns pale. The muscles of the foot and leg atrophy.
- IV degree. Destructive changes are expressed in unbearable, constant pain in the ankle and toes. The distal parts of the lower extremities are covered with non-healing ulcers, around which there is redness and a gray coating inside. The lower leg and foot swell. Without timely medical care, gangrene occurs.
2. Weakening (presence of only systolic murmur) or complete absence of pulsation of the femoral arteries.
3. Erectile dysfunction in male patients that cannot be cured is associated with ischemia: spinal and pelvic organs. In addition to sexual impotence itself, for the same reasons, pain in the lower abdomen may occur when walking.
Treatment of Leriche syndrome
Treatment of this disease is carried out therapeutically and surgically. In case of severe damage to the aorta, surgery is inevitable, since gangrene quickly develops with the disease in question, and therefore doctors are forced to amputate the lower limb. It is possible to perform endarterectomy (removal of the substrate that causes the blockage), prosthetics (replacing the affected area of the vessel with a healthy one), bypass surgery (creating a path to resume blood flow bypassing the diseased area), stenting (placement of a special device that does not allow the artery to collapse).
Does surgery guarantee a complete cure for Leriche syndrome? Treatment is also carried out after surgery - the patient must take medications that prevent the formation of blood clots. This therapy can be continued for life.
Surgical treatment of Leriche syndrome does not always lead to complete recovery. So, after amputation the patient becomes disabled. If the patient does not follow the doctors’ recommendations (for example, continues to smoke), the disease may recur with death.
You can be examined for the presence of atherosclerosis of the vessels of the lower extremities and determine the risk of developing Leriche syndrome only at an appointment with a specialist. You can sign up for a consultation on our website https://www.dobrobut.com/.
Treatment
Treatment of Leriche syndrome aims to improve blood flow in the arteries of the legs, prevent the progression of the disease and the development of complications, the most dangerous of which are gangrene, myocardial infarction, and stroke.
Depending on the stage of the disease and the nature of the manifestations, conservative therapy or surgery is prescribed. Conservative treatment includes the prescription of drugs that improve blood circulation in the microvasculature, tissue trophism, and vasodilators.
The patient should know that only treatment prescribed by a doctor will not bring the desired result without excluding risk factors for the disease and lifestyle changes, therefore the main principles of therapy are:
- Elimination of risk factors (control of blood pressure, lipid levels, blood glucose);
- Complete elimination of smoking;
- Regular walks;
- Taking medications to improve blood flow.
Conservative therapy
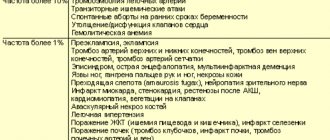
For stages I and IIA, only conservative treatment is permissible; for more advanced forms, surgery cannot be avoided. Among the drugs prescribed:
- Pentoxifylline, which reduces platelet aggregation and improves the rheological properties of blood. It has been proven that the drug can reduce the symptoms of the disease, but it is effective only in 30-40% of patients;
- Reopoliglucin, reomacrodex, which reduce blood viscosity;
- Acetylsalicylic acid, which prevents thrombosis;
- Cilostazol, which improves blood rheological parameters;
- Ticlopidine, clopidogrel, which have pronounced antiplatelet properties;
- Sulodexide, which reduces viscosity by reducing the content of fats and fibrinogen in the blood;
- Nicotinic acid and its derivatives, which cause dilation of peripheral vessels and promote the breakdown of fibrinogen;
- Antispasmodics (papaverine, drotaverine);
- For severe pain, analgesics are indicated.
For long-term non-healing trophic ulcers, dressings of the affected areas are performed using local agents that improve trophism and regeneration (solcoseryl, methyluracil).
Operation
Surgical treatment is necessary starting from stage IIB of the disease. Before prescribing an operation, the surgeon evaluates the condition of the aorta, vessels of the lower extremities, coronary arteries and cerebral arteries for atherosclerotic lesions and surgical risks associated with it.
For Leriche syndrome, reconstructive operations are performed, the main of which are:
- Endarterectomy – removal of an atherosclerotic plaque with suturing of the vessel or replacement of the defect with synthetic material, native vessels.
- Prosthetics – the altered fragment of the artery is removed, and in its place a synthetic prosthesis or a section of the patient’s vessel taken from another area (autovenous) is installed.
- Aortofemoral bypass surgery - if the lesion is significant, an anastomosis is performed to bypass the damaged area of the vessel (between the aorta and the femoral artery). If the bifurcation of the aorta and both iliac arteries are affected, then a prosthesis is used that completely replaces the site of the bifurcation (in the form of “pants”).
- Stenting – a stent (hollow tube) is installed in a vessel through which blood flows; the method is indicated for patients with damage to the vessels of the heart, brain, or high operational risk when undergoing prosthetics or bypass surgery.
operations for Leriche syndrome – bypass surgery (1) and angioplasty with stenting (2)
If the severity of atherosclerosis is such that it is no longer possible to restore blood flow, or gangrene of the limb has developed, then the only type of operation may be amputation of the leg to a level where blood flow is still present.
It is worth noting that patients who have undergone surgery, as well as those undergoing conservative treatment, must take antiplatelet drugs (aspirin, clopidogrel). In the case of widespread atherosclerosis, such treatment is considered basic and can even be prescribed for life. Vascular drugs are used in courses, and antiplatelet agents are used long-term, throughout life.
Non-drug methods of treating Leriche syndrome consist of ultraviolet and laser irradiation of the blood to reduce its viscosity and reduce platelet aggregation, hyperbaric oxygenation, and physiotherapeutic procedures (UHF, electrophoresis).
Leriche syndrome is a dangerous disease with a serious prognosis. Approximately every third patient who died from cardiovascular pathology has one or another of its manifestations. Prevention of the progression of vascular changes largely depends not only on the timeliness of treatment, but also on the patient’s desire to save the limb and life. Surgeons know of cases where, even after losing a leg, patients did not give up smoking and did not follow the prescribed recommendations. If there are even the slightest signs of impaired arterial blood flow in the vessels of the legs, you should urgently consult a doctor and begin treatment immediately.
Forecasts
Timely reconstructive vascular operations for Leriche syndrome in 90% of cases lead to successful results in restoring blood flow. Long-term results in such cases are also usually favorable.
Without treatment, the prognosis for the outcome of Leriche syndrome is always unfavorable. Approximately 8 years after the first signs of pathology appear, about 1/3 of patients die, 1/3 undergo limb amputation, and in the remaining 1/3 the symptoms of ischemia constantly progress. Experts note that this pathology develops faster in young patients.
Leriche syndrome is a dangerous pathology and requires timely treatment from a vascular surgeon when the first signs of ischemia of the lower extremities appear. To restore normal blood flow in the initial stages of the disease, conservative therapy may be recommended. In the future, surgical treatment is necessary to restore the patency of the affected arteries.
Channel One, program “Live Healthy!” with Elena Malysheva, in the “About Medicine” section, a conversation about Leriche syndrome:
Angioplasty and stenting
The chronic form of NVC syndrome is more difficult to treat. When the venous outflow is decompensated, it becomes necessary to restore the patency of the vessel. Open operations involving the isolation of the IVC and its replacement with a vascular prosthesis are feasible, but very traumatic and ineffective. The artificial vena cava prosthesis often thromboses again and the complex operation becomes completely useless. With the advent of new composite materials for large-diameter stents, our clinic began to perform endovascular methods for restoring the patency of the vena cava. Angioplasty and IVC stenting are performed by experienced endovascular surgeons at the Innovative Vascular Center. The point of the intervention is to restore the patency of the closed segment of the inferior vena cava with a special conductor, a high-pressure balloon and the installation of a metal frame - a stent.
Diagnosis of pityriasis
If you find suspicious spots on the skin, you should promptly contact a dermatologist. During a visual examination, the doctor assesses the nature of the rashes, their shape, size, location on the body and is able to make the correct diagnosis. After dermatoscopy, the following studies are additionally carried out: biochemical tests of blood and urine, RMP (microprecipitation reactions with antigens), skin scrapings from injured areas.
A more complex diagnosis is carried out if the skin disease lasts more than six weeks. In these cases, discharge from the affected lesions is sent for bacterial culture. A biopsy and subsequent histological studies will help make the correct diagnosis. In order to distinguish Zhiber's disease from other types of lichen, toxicerma, psoriasis, complicated syphilis and other pathologies, fluorescent diagnostics are carried out, scrapings are checked for the presence of pathogenic fungi, RPR tests are done for syphilis, etc.
Prevention
To prevent Raynaud's disease, medical experts recommend using contrast baths to train blood vessels. It is also necessary to eat properly and nutritiously, and not to overuse coffee, as it constricts blood vessels.
Avoid overheating; in cold weather, always wear gloves and dress appropriately for the weather.
Raynaud's disease should only be treated under the supervision of a qualified physician. You can get quality medical care in.
Pityriasis rosea in pregnant women
Pityriasis occurs more often in women than in men. It is especially dangerous when the skin disease occurs in pregnant women. If you notice any rashes, it is important to immediately visit a dermatologist and undergo treatment. It is unacceptable to risk the baby’s health and expect the plaques to disappear on their own. If the disease is not treated, then bacterial infections appear, which are much more difficult to deal with.
If a pregnant woman has not been diagnosed with pityriasis rosea, it is nevertheless important to adhere to the following recommendations:
- clothing made from cotton and linen is preferable to synthetic and woolen fabrics
- limiting heavy physical activity
- For hygienic purposes, use only warm water
- timely moisturizing of damaged skin areas
Symptoms
Clinical features of Raynaud's syndrome:
- most often, color changes are observed on the fingers;
- changes begin on one finger, then spread to other fingers and become symmetrical on both hands;
- the II-IV fingers of the hands are most often involved, the thumb usually remains unchanged;
- changes in skin color may also be observed in other areas: ears, tip of the nose, face, above the knees;
- during Raynaud's attacks, livedo reticularis may appear on the extremities, which disappears after the completion of vasospasm;
- in rare cases, damage to the tongue is observed, which is manifested by numbness and transient speech impediments.
Clinically, an attack of Raynaud's disease consists of three phases:
- The first phase is expressed in spasm of the arteries, pallor of the skin, a decrease in its temperature, numbness, and pain.
- The second phase is characterized by the development of cyanosis of the skin and increased pain.
- The third phase is swelling and redness of the skin, decreased pain.
However, classic three-phase Raynaud's attacks are observed only in 15% of patients; in most cases, two-phase color changes are observed Source: Alekperov R.T. Raynaud's syndrome in the practice of a rheumatologist / R.T. Alekperov // Modern rheumatology. - 2014. - No. 2. - P. 37-46. .
The duration of the attack is usually 15-20 minutes, but sometimes it can last even several hours.
At the last stage of the disease, persistent skin lesions develop, and deformation of the fingers is possible.
In most cases, Raynaud's disease is symmetrical in nature: if the pathology affects one hand, then after some time the pathology develops on the second.