- Epidemiology
- Risk factors
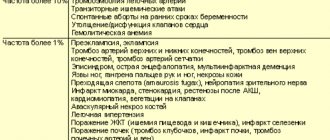
- Clinical manifestations
- Diagnostics
- Prognostic factors
- Treatment
Myelodysplastic syndromes (MDS) comprise a group of malignant tumor diseases of the hematopoietic system.
In these diseases, the maturation of bone marrow cells is disrupted with changes in their structure and functional properties.
A characteristic, but not obligatory, feature of the disease is the outcome of acute leukemia.
The life expectancy of patients varies widely - from several months to 10 or more years.
Epidemiology
The incidence of MDS averages 3-4 cases per 100,000 population per year and increases with age.
The main group of patients with MDS are elderly people (average age - 70 years). In people over 70 years of age, the incidence reaches almost 23, and in the age group over 80 years - almost 40 cases per 100,000 population per year.
The morbidity rate in men slightly exceeds the morbidity rate in women. MDS in childhood is extremely rare.
In 10-15% of cases, MDS is a complication of chemotherapy and radiation for another cancer.
The true incidence of MDS remains unknown. This is due to the asymptomatic course of the disease in many patients, difficulties in diagnosis, and other reasons.
Treatment of myelodysplastic syndromes (MDS)
Therapeutic measures are carried out in accordance with the assessment of the risk of MDS disease. To assess risks, so-called scale systems are used. Currently, the most common scoring system is the International Prognostic Scoring System (IPSS). Low and intermediate level 1 risk groups are considered low-risk MDS, while intermediate level 2 and high-risk groups are classified as high-risk patients.
Low-risk myelodysplastic syndrome (MDS)
- Maintenance therapy (treatment that reduces the complications of the disease, but does not affect the natural history of the disease):
Giving red blood cells or platelets if these blood levels are lowAntibiotics for infections
When patients have low white blood cell counts ( leukopenia, neutropenia, or granulocytopenia ), administration of certain growth factors may increase the number of white blood cells in the blood. These substances are called granulocyte colony-stimulating factors (G-CSF).
Patients requiring transfusions are at risk of developing severe iron overload as the disease progresses. This is due to the fact that red blood cells contain hemoglobin, which binds oxygen and transports it to tissues. Hemoglobin contains iron. With each pack of red blood cells a patient receives, they automatically absorb about 200-250 mg of iron. This is high compared to your natural daily iron intake of about 1 mg per day. Iron excretion is limited to 1 mg, so blood transfer inevitably results in increased iron levels in the body. While a healthy person contains approximately 3-4 g (i.e. 3000-4000 mg) of iron in the body, this amount can easily increase tenfold in the case of patients requiring long-term transfusions. However, in these quantities, iron is harmful because it is distributed into the tissues of the liver, heart and glands and causes disorders there. In order to be able to remove iron, so-called iron chelators are used today, which can reduce the level of iron in the body when taken regularly.
Care should be taken not to administer to patients with low platelet counts any medications that further suppress platelet function, such as so-called nonsteroidal anti-inflammatory drugs (aspirin, diclofenac, ibuprofen, naproxen, and others). This can lead to life-threatening bleeding. In some patients, the platelet count does not increase even though platelets are given to them. These patients are called platelet transfusion refractory. The cause is usually the formation of antibodies after frequent blood transfusions. In these cases, antifibrinolytic agents such as para-aminomethylbenzoic acid may be used to reduce the risk of bleeding.
Several international studies have shown that erythropoietic growth factors (erythropoietins or EPOs, which increase the number of red blood cells) can, under certain conditions, lead to a temporary but sustained increase in hemoglobin levels. A recently published index predicts the likelihood of response to erythropoietin therapy. This index combines the number of completed transfusions with the current erythropoietin level. Patients who require many transfusions and have high EPO levels have a low likelihood of responding to the drug.
- Immunosuppressive measures are based on the understanding that antibodies - cytotoxic T cells - through inhibitory substances (cytokines) contribute to insufficient blood formation. In a phase II study, 61 patients with refractory anemia, transfusion-dependent anemia and thrombocytopenia . Antithymocyte globulin and cyclosporine A were used for treatment. 33% of patients eliminated the need for chronic transfusions, 44% improved peripheral granulocyte counts, and 56% achieved a clinically significant increase in platelets.
- Immunomodulatory substances . In addition to TNF-alpha inhibition, their mode of action also involves activation of T and NK cells, as well as direct pro-apoptotic mechanisms. The substance thalidomide has a cytokine inhibitory effect and has been successfully used in myelodysplastic syndromes. Treatment for newly diagnosed MDS is more effective than for advanced MDS. However, 30% of patients discontinue treatment due to side effects (fatigue, nerve damage, constipation). Thalidomide analogues have been developed and are recommended for use in early forms of MDS. 4-amino-glutarimide-lenalidomide has a completely different side effect profile and does not cause polyneuropathy (nerve damage) or fatigue. In patients with defects of chromosome 5 (so-called 5q-MDS), the drug is particularly effective: an evaluation of an international phase II study showed a longer-term freedom from the need for blood transfusions in almost 70% of treated patients. About 50% of patients did not require transfusion even after 2 years of continuous use. 70% of patients achieved a cytogenetic response (decrease in the number of del (5q) in the bone marrow by 50%), 44% achieved a complete cytogenetic response, i.e. the typical del(5q) chromosome was no longer detected in the analysis. In 2013, the European Medicines Agency approved the use of the drug for patients with an isolated 5q chromosomal abnormality.
High risk MDS
- 5-azacytidine and 5-aza-2′-deoxycytidine (decitabine) are pyrimidine analogs that, at noncytotoxic concentrations, inhibit DNA methyltransferase (demethylating agents) and experimentally induce the maturation of certain bone marrow cells. 5-azacytidine was approved for the treatment of MDS in the United States after a phase III trial demonstrated improved patient survival compared with patients in the control group. At the latest assessment, the rate of complete remissions and partial responses in the treatment group was 15.7%, while the duration of transition to leukemia was statistically significantly increased with therapy. An evaluation of an international phase III trial comparing 5-azacytidine with other treatments demonstrated an increase in life expectancy. In the azacitidine treatment group, patients survived for an average of 24 months, while in the control group, survival was 15 months. Based on these data, the substance was approved on December 23, 2008 for the treatment of progressive myelodysplastic syndromes in Europe.
- Intensive chemotherapy with protocols used for AML (acute myeloid leukemia) can be used to induce remission in patients under 70 years of age. In recent studies that included at least 30 patients, overall remission rates were 45-79%. Early mortality was similar to that in patients with acute myeloid leukemia. A favorable prognosis with long-term treatment is mainly documented in patients with refractory anemia with an excess of RAEB-T blasts with a normal karyotype. Allogeneic blood stem cell transplantation is the preferred treatment for patients with high-risk MDS under 50 years of age from a matched donor. Disease-free survival in this case is 40% six years after transplantation. The patient's age at transplantation is one of the biggest risk factors.
Share
0
Risk factors
It is known that the risk factors for the development of MDS and acute myeloid leukemia are similar.
In childhood, the main predisposing factors for the development of MDS are genetic diseases (Down syndrome, Fanconi syndrome, neurofibromatosis, dyskeratosis congenita, etc.).
A genetic predisposition has also been noted in adults whose parents suffered from MDS.
Another risk factor is ionizing radiation , which is confirmed by the results of long-term observation of the population living near nuclear power plants and survivors of atomic bomb explosions.
Chemical risk factors include organic compounds (gasoline and its derivatives, pesticides, solvents), as well as inorganic (asbestos, quartz, arsenic) substances .
MDS develops more often in smokers compared to non-smokers.
A higher risk of MDS was observed among workers in agriculture, the textile industry, medical institutions, machine operators, and people living near factories.
The most studied risk factor is the effect of chemotherapy and radiation treatment . Most often, MDS is diagnosed in patients treated for breast cancer, multiple myeloma, Hodgkin's lymphoma (lymphogranulomatosis), non-Hodgkin's lymphoma (lymphosarcoma), and small cell lung cancer.
MDS has been best studied in patients with Hodgkin lymphoma. The incidence of MDS in this category of patients ranges from 1.5 to 10% and depends on age, previous treatment and duration of observation.
The average period from the start of treatment for Hodgkin's disease to the diagnosis of MDS is about 4-6 years. There is no convincing evidence of an increased risk of MDS with the combination of chemotherapy and radiation compared with chemotherapy alone.
MYELODYSPLASTIC SYNDROMES:
development mechanisms, symptoms, treatment
What is MDS?
Myelodysplastic syndromes (MDS) are a group of diseases that primarily affect the bone marrow and occur when the bone marrow does not produce enough healthy blood cells.
Myelodysplastic syndromes mainly affect older people (most patients are between 60 and 85 years old), but younger people (over 30 years old) can also get sick with them. By type, MDS differs into primary (idiopathic) - 80-90% of cases, secondary (due to previous chemotherapy and other factors) - 10-20%. Sporadic, familial - rare, but in this case it is necessary to exclude Fanconi anemia or other variants of the phenotype with mutator genes. The 5-year survival rate for MDS does not exceed 60%.
With few exceptions, the causes of MDS are unknown. Congenital MDS has been described in some people. If such an external factor cannot be identified, then the disease is called “primary MDS.”
Risk factors for primary MDS are considered to be contact with toxins (gasoline, organic solvents, pesticides), ionizing radiation, smoking, congenital and hereditary diseases (Fanconi anemia, severe congenital neutropenia, Shwachman-Diamond syndrome, Diamond-Blackfan anemia), and old age. Secondary MDS can develop after previous chemotherapy for cancer (Hodgkin's lymphoma, breast cancer, etc.) or after blood cell transplantation as a result of the mutagenic effect of a number of drugs (mechlorethamine, procarbazine, chlorambucil, etc.).
There is no convincing evidence that MDS can be caused by any viruses, so MDS cannot be transmitted to others. Since family members are not at increased risk, they do not need to undergo additional testing.
MDS develops as a result of a disruption in the normal functioning of the bone marrow.
The main function of the bone marrow is to produce blood cells, which include red blood cells, platelets and white blood cells. Each of these cells, after leaving the bone marrow, performs important life-saving functions. Providing tissues and organs with oxygen (red blood cells), stopping bleeding (platelets) and protecting against infections (leukocytes) depends on them. Healthy bone marrow contains immature blood cells called stem cells or progenitor cells that, as needed, turn into mature red blood cells, white blood cells and platelets to perform their functions.
In MDS, these stem cells may not reach maturity and/or have a shortened life cycle, dying in the bone marrow before being released into the blood, which leads to a decrease in the number of mature circulating blood cells (so-called cytopenia) and, accordingly, a decrease in their function. In addition, mature blood cells circulating in the peripheral blood may not function properly due to so-called dysplasia - abnormalities in the shape or morphology of blood cells found in the bone marrow and/or peripheral blood.
The failure of the bone marrow to produce healthy mature cells occurs gradually, and patients may suffer long-term effects of the disease, such as anemia, bleeding and decreased resistance to infections. In addition, up to 30% of MDS patients may develop acute myeloid leukemia (AML).
Clinical manifestations of MDS
Many patients in the early stages of the disease do not experience any symptoms because... There is a sufficient number of mature cells in the blood. One of the most characteristic symptoms at the onset of the disease is anemia (low red blood cells, hemoglobin and hematocrit).
Patients suffering from anemia usually experience a constant feeling of fatigue, weakness, decreased performance, and inability to concentrate. Women tolerate anemia better than men. As anemia increases, increased heart rate, difficulty breathing, drowsiness, and dizziness occur. Fainting may develop. Anemia is especially difficult for elderly patients and people with heart and lung diseases: they may develop angina (pain in the heart area), myocardial infarction, increase shortness of breath, decrease exercise tolerance, and develop heart rhythm disturbances.
When the vessels of the lower extremities are damaged, the manifestations of the so-called intermittent claudication (the appearance of pain in the legs when walking short distances) intensify. Therefore, changes in blood tests are often learned during an examination for therapeutic pathology.
.
Often, patients are treated for anemia under the supervision of a therapist who uses iron supplements, vitamin B12, and folic acid for this purpose, but does not achieve success, i.e. anemia is “refractory” (resistant) to these standardly used drugs, which may be a reason to consult a hematologist.
Anemia may be accompanied by a decrease in the number of neutrophils (neutropenia) and platelets (thrombocytopenia). A low number of leukocytes in the blood (the norm is from 4,000 to 10,000 leukocytes in 1 microliter of blood) reduces the body's resistance, primarily to bacterial infection. Patients often suffer from recurrent skin infections, ear, nose and throat infections, bronchopulmonary infections (bronchitis, pneumonia) and infections of the urinary tract, mouth (stomatitis) and teeth, accompanied by fever.
With thrombocytopenia (normal blood levels from 130,000 to 450,000 platelets in 1 microliter of blood), patients experience increased bleeding with a tendency to bruise and bleeding even as a result of minor blows and scratches. Even small cuts may take longer than usual to stop bleeding. Severe thrombocytopenia, which is observed in rare cases, occurs when the number of platelets decreases below the level of 20,000 in 1 μl or 20x109/l and is accompanied by bleeding.
Bruising can be significant, some as large as the palm of your hand. Nosebleeds are common, and patients complain of bleeding gums, for example, during dental procedures, and women may experience heavier menstrual bleeding.
It is recommended that a patient with MDS consult a hematologist before seeking dental care, given the risk of bleeding and infection. Moreover, according to indications, medications can be prescribed (prophylactic antibiotics, etc.).
Diagnosis of MDS
1. The first step in diagnosing MDS is to perform a clinical blood test by taking a blood sample from a vein. The blood sample determines the number of blood cells (erythrocytes, leukocytes and their subtypes, as well as platelets), the shape and size of erythrocytes and leukocytes.
2. To exclude the most common anemias, a blood serum test is performed to determine the level of iron and ferritin (assessment of iron reserves in the body), vitamin B12 and folic acid, erythropoietin (a protein that is produced in the kidneys in response to low oxygen levels in the tissues body, stimulates the formation of red blood cells in the bone marrow).
3. If the cause of bone marrow damage is considered probable, a bone marrow examination is indicated. Bone marrow examination includes examination of a bone marrow aspirate (myelogram analysis, cytological examination), obtained by taking a sample of liquid bone marrow, and a bone marrow trephine biopsy (sample of the bone component of the bone marrow).
During the bone marrow examination, the following is determined:
1) percentage of blasts and cells with signs of dysplasia;
2) iron content in cells of the erythroid series;
3) chromosomal abnormalities, such as missing or extra chromosomes in bone marrow cells. Any abnormalities are described in the hematology report, and chromosomal abnormalities (absence or deletion of chromosomes, and the presence of altered or additional chromosomes or parts of chromosomes) are included in the cytogenetic report. Subsequently, repeated bone marrow studies are performed in patients with MDS in order to determine the clinical status of MDS over time (remission, stabilization, progression) and evaluate the effect of the therapy.
Determining the severity of MDS in humans.
Based on the information received, not only the diagnosis of MDS is established, but also the subtype of the disease and the prognosis for a particular patient are determined. Various classification systems have been developed for this purpose. According to the latest proposed classification, known as the World Health Organization (WHO) Classification, there are six different subtypes of MDS, the division of which is based on analysis of large international databases and a better understanding of disease processes.
In the past, the French-American-British classification system (FAB classification) was widely used. Some hematologists continue to use this system today.
FAB classification
was developed in the early 80s of the last century by a group of doctors from France, the United States of America and Great Britain who specialized in the diagnosis of MDS. The main criterion in this classification was the percentage of blast cells in the bone marrow, with a percentage of these cells less than 2% considered normal for healthy bone marrow. According to the FAB classification, the following five subtypes of MDS are distinguished:
· refractory anemia (RA);
· refractory anemia with ring sideroblasts (RACS);
· refractory anemia with excess blasts (RAEB);
· refractory anemia with excess blasts in transformation (RAIB-T);
· chronic myelomonocytic leukemia (CMML).
The WHO classification system for MDS in adults retains some elements of the FAB classification system and expands the categories of MDS subtypes. The main characteristics of the six subtypes of MDS, as distinguished by the WHO classification system, are highlighted in the table below.
Noteworthy changes in the WHO classification system, compared to the FAB classification system, are as follows:
· division of the RAEB subtype into two subtypes;
· exclusion of CMML as an independent subtype;
· inclusion of MDS with chromosomal abnormality “syndrome 5q-” as a separate subtype;
· exclusion of the subtype refractory anemia with excess blasts in transformation (RAEB-T), which is currently considered to be included in AML;
· introduction of the category “MDS unclassified”.
Refractory anemia (RA).
Patients in this category suffer from anemia that does not respond to treatment with iron supplements or vitamins, that is, it is refractory to such treatment. Anemia may be accompanied by thrombocytopenia and mild to moderate neutropenia.
Refractory anemia with ringed sideroblasts (RACS).
In patients with this type of anemia, dysplasia is observed only in the erythroid series. Sideroblasts are erythroid cells containing iron granules; ring sideroblasts are abnormal. Refractory anemia with or without ringed sideroblasts (RAS) is considered the most benign subtype in the WHO classification system.
Refractory cytopenia with multilineage dysplasia (RCMD).
This category includes patients who have refractory cytopenia (persistently low numbers of some type of blood cell, such as refractory neutropenia or refractory thrombocytopenia) and have minimal dysplasia in at least two types of blood cells, as well as a blast count of 5% and less, or the number of ring sideroblasts is less than 15%. If the number of ring sideroblasts in a patient with RCMD exceeds 15%, a diagnosis of RCMD-CS is made.
| WHO classification of MDS | |
| MDS subtype | Characteristic |
| RA | Minimal dysplasia in one blood cell type (red blood cells or red blood cells) and <5% blasts in the bone marrow |
| RAX | Dysplasia of erythroid lineage only and > 15% ring sideroblasts |
| RCMD | Dysplasia (>10%) in two or three blood cell types, <5% blasts and <15% ring sideroblasts in the bone marrow (ring sideroblasts >15% is called RCMD-CS) |
| RAEB | |
| RAEB 1 | The number of blasts in the bone marrow is from 5% to 9% |
| RAEB 2 | The number of blasts in the bone marrow is from 10% to 19% |
| MDS/MPZ | Dysplasia in the presence of characteristics usually associated with a myeloproliferative disorder; includes HMML |
| Syndrome 5q - | Patients who do not have chromosomal abnormalities, with the exception of a deletion in the long arm of chromosome 5 |
| MDS unclassifiable | Includes patients with cytopenia in one blood cell type other than anemia (ie, neutropenia or thrombopenia) and any unusual characteristics (eg, bone marrow fibrosis) |
Refractory anemia with excess blasts (RAEB).
This category is divided into two subcategories that differ in the number of blasts in the bone marrow. In patients with RAEB-1, the number of blasts ranges from 5% to 9%, and in patients with RAEB-2 – from 10% to 19%.
Myelodysplastic syndrome/myeloproliferative disease (MDS/MPD).
Patients with MDS/MPD include those with chronic myelomonocytic leukemia (CMML), which is a separate category in the FAB classification system.
5 q - (5 q
minus) syndrome.
5q- syndrome, currently classified as a separate subtype of MDS, was first described more than 30 years ago. The name of this syndrome is associated with chromosome number 5, namely a chromosomal abnormality (deletion) in the long arm (q) of chromosome 5. A deletion within the long arm of chromosome No 5 is the only chromosomal abnormality in MDS patients diagnosed with 5q- syndrome.
The syndrome typically occurs in middle-aged women, usually age 65, and is accompanied by mild to moderate anemia, a low white blood cell count (leukopenia), and often a normal or elevated platelet count. Syndrome 5q- is characterized by a favorable prognosis, with a life expectancy of more than five years from the time of diagnosis (a criterion accepted in medicine to assess the severity of the disease).
Unclassifiable MDS.
This category includes patients with cytopenia in one blood cell type (eg, thrombopenia or neutropenia) and any unusual characteristics (eg, bone marrow fibrosis), accounting for no more than 1% to 2% of all MDS cases.
Another system used to characterize MDS activity and provide a patient's prognosis is the International Prognostic Scoring System ( IPSS ).
To assess the severity of MDS, the International Prognostic Scoring System (IPSS) is used; the disease is scored based on the danger it poses to the patient, that is, the time at which the disease is likely to progress or transform into AML. The prognostic score is determined based on the percentage of blasts present in the bone marrow, the results of a cytogenetic study, as well as blood cell counts and other blood test results.
The prognostic score is determined by adding individual scores based on the percentage of blasts, cytogenetic studies and blood tests and is used to assess the outcome of the disease for a patient with MDS. The prognostic score shows which risk group the patient belongs to.
| Determination of prognostic score Predictive score: the sum of individual scores for blasts, cytogenetic study results and blood test results | |
| Percentage of blasts in bone marrow | Point |
| 5% or less | 0,0 |
| 5-10% | 0,5 |
| 11-20% | 1,5 |
| 21-30%* | 2,0 |
| Cytogenetic study results** | |
| good | 0,0 |
| intermediate | 0,5 |
| bad | 1,0 |
| Level of cytopenias based on blood test results*** | |
| 0 or 1 cytopenia | 0,0 |
| 2 or 3 cytopenias | 0,5 |
| *Patients whose bone marrow contains more than 20% blasts are diagnosed with acute myeloid leukemia (AML). ** Prognostically good results mean a normal set of 23 pairs of chromosomes or a set in which there is only partial loss of the long arm of chromosome No. 5. Intermediate results include all results that do not fall under the definition of “good” or “bad”. Poor prognostic outcomes include the loss of one of the two chromosomes No. 7 (monosomy 7), the addition of a third chromosome No. 8 (trisomy 8), or three or more abnormalities. *** The level of cytopenias based on the results of a blood test is determined as follows: neutrophils < 1,800 per 1 microliter of blood; hematocrit < 36% of red blood cells in the total blood volume in the body; platelets < 100,000 per microliter of blood. | |
Treatment of MDS
The goals of treatment are to restore peripheral blood parameters, reduce the clinical manifestations of MDS, reduce dependence on transfusions of blood components, delay the transformation to AML, increase life expectancy, and improve the quality of life of patients.
Treatment options for patients with MDS depend on the type of disease, prognostic factors, age of the patient, and comorbidities and can be divided into potentially curative therapies and supportive care.
Supportive and symptomatic therapy
The basis of treatment for MDS is maintenance therapy, which includes the use of growth factors, treatment of intercurrent infections and replacement therapy with blood components.
One aspect of maintenance therapy for patients with MDS is the use of hematopoietic growth factors, which act on the bone marrow to enhance the production of one or more hematopoietic lineages. In recent years, several human recombinant growth factors have appeared, including erythropoietins (EPO: epoetins α and β, darbepoetin), garnulocytic and granulocyte-macrophage colony-stimulating factors (G-CSF and GM-CSF: filgrastim, molgramostim), thrombopoietin receptor agonists (romiplostim, eltrombopag), which stimulate the production of red blood cells, granulocytes and platelets, respectively. Only 20-30% of patients with MDS respond to growth factor treatment, which reduces the need for replacement therapy. Prognostic factors for response to therapy are the initial level of EPO, the severity of transfusion requirements, duration of the disease, type of disease according to the FAB or WHO classification, and rice group according to the IPSS scale.
Despite the fact that the cost of hematopoietic growth factor therapy is 3-4 times higher than the cost of transfusion therapy, the former remains the preferred type of treatment. Successful treatment with hematopoietic growth factors can avoid or, in some cases, reduce the need for multiple transfusions of blood components and the attendant risk of iron overload.
The basis of maintenance therapy for patients with MDS is replacement therapy with blood components. In patients at low risk of developing AML, anemia may be the main clinically significant problem. Replacement therapy relieves the symptoms of anemia and is therefore an important treatment option. The frequency of transfusions depends on the patient's condition, the severity of anemia, as well as concomitant pathology. Some patients may need red blood cell transfusions every one to two weeks, while others may need just one transfusion every six to 12 weeks. The result of replacement therapy is an increase in hemoglobin levels, which, as studies show, has a positive correlation with quality of life. Platelet transfusions are rarely given and only in cases where the platelet count is extremely low and/or there is life-threatening bleeding. However, the benefits of transfusion therapy must be weighed against the risk of infectious complications, immunological side effects, and iron overload.
The accumulation of excess iron in the body is a serious clinical problem that, if left unaddressed, can lead to organ damage. Repeated transfusions of red blood cells containing iron as part of hemoglobin lead to the deposition of excess iron in the cells of the reticuloendothelial system, primarily in the liver, spleen, endocrine glands and heart, as well as in small amounts in brain tissue or skeletal muscles. Therefore, the main complications of iron overload are heart disease, liver disease and endocrine disorders. In order to prevent iron overload in the body, laboratory monitoring of iron reserves (serum ferritin) is used, as well as drugs that chelate or bind iron and promote its removal from the body.
There are currently two drugs available to combat iron overload in transfusion-dependent patients—deferoxamine and deferasirox.
The drug deferoxamine (Desferal) delays the toxic effect of the accumulation of excess iron in the body. It is given in addition to blood transfusions and is given by injection, usually 3-7 times a week. Some patients receive subcutaneous injections of the drug 2 times a day. The drug deferasirox (Exjade), a chelator, is taken orally. Treatment with these drugs should be initiated in patients who have received 20-30 units of donor red blood cells, who will undergo chronic transfusion therapy, and in patients with serum ferritin levels persistently exceeding 1000 mcg/L.
Potentially curative therapies
To control the symptoms of the disease or cure MDS in young patients with high-risk MDS, intensive chemotherapy is used to eliminate as much as possible the clone of abnormal cells and achieve long-term remission.
Patients younger than 55 years with IPSS high- or intermediate-2 risk MDS who are not eligible for stem cell transplantation may benefit from chemotherapy similar to that used to treat AML. This treatment method has significant side effects, such as hair loss, oral stomatitis, nausea, vomiting, and loose stools. In addition to these side effects, chemotherapy has an adverse effect on healthy cells along with cells that have undergone dysplastic effects, which requires a long stay in the hematology department. At this time, the patient is given transfusions of red blood cells and platelets, and antibacterial drugs are prescribed to fight the infection. If induction chemotherapy provides adequate control of the abnormal cells (a state of remission), then the restoration of normal blood cells should begin within a few weeks. Unfortunately, the chance of controlling MDS with induction chemotherapy is about 30%. Even in cases of successful treatment, the disease can return - recur.
1. The only known treatment that can cure MDS is allogeneic (donor) hematopoietic stem cell transplantation. It should be kept in mind that this is a complex procedure associated with the risk of early and late complications. The outcome of treatment depends on the degree of compatibility (HLA compatibility) of the donor and the patient (recipient), as well as on the availability of suitable donor cells (presence of compatible blood brothers and/or sisters, availability of a donor bank). Thus, there are strict indications and contraindications for this type of treatment: it is suitable for those cases where patients are able to undergo a stem cell transplant and have a suitable donor. Recently proposed transplantation techniques with reduced-intensity conditioning regimens have had some success in patients with MDS over 55 years of age. Research in this area is ongoing.
2. The participation of immune mechanisms in the development of bone marrow pathology in MDS has led to the development of treatment methods using immunosuppressants. From this group of drugs, antithymocyte globulin (ATG) and antilymphocyte globulin (ALG) and cyclosporine A are used in the treatment of MDS. ALG/ATG treatment is more effective in young patients with the presence of the HLA-DR15 antigen who have received red blood cell transfusions for a short time. This treatment achieves independence from red blood cell transfusions in 33% of patients; 56% of patients with severe thrombocytopenia had a significant increase in platelet levels, and 44% of patients with neutropenia had an increase in neutrophil levels greater than 1x109/L. Cyclosporine A was most effective in patients with less than 5% blast cells in the bone marrow, a normal karyotype, hypocellular bone marrow and accumulations of lymphoid cells in the trephine biopsy specimen.
3. The study of the mechanisms of development of MDS, undertaken in recent years, has shown that this pathology is characterized by hypermethylation of the promoter region of some tumor suppressor genes, which leads to the “silence” of these genes and the proliferation of tumor cells and transformation into AML. Based on this knowledge, so-called hypomethylating agents have been developed, which promote DNA hypomethylation by inducing the expression of previously “switched off” genes.
In May 2004, the US Food and Drug Administration (FDA) approved the injectable drug azacitidine (Vydaza) for the treatment of all types of MDS. In the Russian Federation, the drug was approved for use in 2010 for the treatment of MDS, AML and CMML. The results of the study showed that azacitidine significantly prolongs life in patients with intermediate and high-risk myelodysplastic syndrome (MDS), as well as with acute myeloid leukemia 20-30% blasts (previously classified as high-risk MDS), for whom stem cell transplantation/intensive chemotherapy is not indicated .
According to Russian protocols, patients with intermediate-2/high-risk MDS and AML who are not suitable for intensive chemotherapy are treated with low doses of cytarabine and/or with maintenance therapy. This treatment alleviates the symptoms of the disease and improves the quality of life of patients, but does not have other significant advantages compared to the natural course of the disease. At the same time, the life expectancy of patients with high-risk MDS receiving azacitidine increases 3 times compared to the current treatment. Moreover, the differences between the azacitidine group and the maintenance therapy and low-dose cytarabine groups are statistically significant (p = 0.045), regardless of age or karyotype (analysis of data from the phase III AZA-001 study) [1]
Azacitidine increases the number of MDS patients who do not require blood transfusions by 4 times. In addition, azacitidine is indicated as temporary therapy in patients awaiting a donor for transplantation (MDS treatment guidelines, NCCN, 2010).
Grade 3-4 adverse events occurring during azacitidine treatment include hematologic (71.4%), including thrombocytopenia (85%), neutropenia (91%), and anemia (57%). Febrile neutropenia occurred in 8.0% of patients, and extremely rarely (<2%) neutropenic sepsis, pneumonia, thrombocytopenia, and hemorrhagic adverse events were recorded.
Azacitidine is administered subcutaneously 75 mg/m2 once a day for 7 days every 21 days (cycle), at least 6 cycles. It has a favorable safety profile and can be used on an outpatient basis.
In May 2006, the FDA approved the use of another hypomethylating drug, decitabine (Dacogen), for the treatment of all subtypes of MDS. The drug was approved for use in the treatment of MDS in the Russian Federation in 2006.
In an open-label, randomized phase III trial[2] of 170 patients comparing decitabine with maintenance therapy, the remission rate was 17%, with hematologic improvement observed in an additional 13% of patients. Decitabine reduces the risk of transformation to leukemia and, in patients who achieve a response, increases survival. The odds of transformation to acute myeloid leukemia or death were 1.68 times higher in the maintenance group compared with the decitabine group.
During decitabine therapy, the most common side effects were: neutropenia -90%, thrombocytopenia -89%, anemia -82%, fever -53%, nausea -42%.
Decitabine is administered intravenously (15 mg/m2 by 3-hour IV infusion every 8 hours for 3 consecutive days every 6 weeks for 10 cycles).
Therapy with both azacitidine and decitabine should be supervised by a hematologist with experience in treating patients with MDS and AML.
4. In December 2005, the US FDA approved the immunomodulatory drug lenalidomide for the treatment of low- or intermediate -1-risk patients with MDS, including del(5q). The drug is administered orally in capsules and has immunomodulatory, antiangiogenic and antitumor effects. At the same time, it does not have the neurotoxicity characteristic of other drugs from this chemical group. The remission rate with lenalidomide was 83% in patients with clonal interstitial deletion of chromosome 5q31.1, while the remission rate was 57% in patients with a normal karyotype and 12% in patients with other karyotype abnormalities. In a phase II study of 146 patients with low- or intermediate-1 risk MDS with del(5q31) requiring chronic transfusion therapy, 64% of patients became transfusion-free. The rate of achieving transfusion independence was higher among patients with isolated del(5q) (69%) than among other patients (49%; P = 0.003).
In February 2012, a file on lenalidomide was accepted by the European Medicines Agency for registration of this indication - “for the treatment of patients with low/intermediate-1 risk MDS, variant of transfusion-dependent anemia with del(5q) with/without other cytogenetic abnormalities”[3].
In summary, myelodysplastic syndromes (MDS) are a heterogeneous group of bone marrow diseases characterized by ineffective hematopoiesis and varying degrees of risk of transformation into acute leukemia. Diagnosing MDS can be difficult because it shares features with other hematologic diseases, including AML, aplastic anemia, and hereditary sideroblastic anemia. Research aimed at uncovering the disease mechanisms that lead to MDS helps us better understand MDS. Equally important is that a better understanding of the mechanisms of the disease leads to the development of new drugs for the treatment of various subtypes of MDS in patients belonging to different risk groups.
Only recently has treatment for MDS expanded beyond supportive care to relieve symptoms. The only potentially curative treatment for MDS is allogeneic hematopoietic cell transplantation, which, however, is not possible in all cases.
In recent years, based on the study of the pathogenesis of this pathology, a large number of drugs have been developed, some of which will find their place in the treatment of MDS. Examples include the angiogenesis inhibitor bevacizumab (Avastin), the cytokine inhibitor infliximab (Remicade), deacetylase inhibitors, histone-valproic acid and vorinostat, among many others. Scientific evidence suggests that combination therapy with drugs with different mechanisms of action will lead to the desired treatment effectiveness.
But whatever therapeutic strategy is ultimately chosen, it must take into account the patient's decision.
Clinical manifestations
Signs and symptoms in patients with MDS are nonspecific. In many patients, MDS remains asymptomatic for a number of years and is detected only during examination for other diseases.
Anemia (anemia) is the most common symptom of MDS and is found in 85-90% of cases. Most complaints are due to the severity of anemia. Leukopenia (decrease in the number of white blood cells), observed in 50% of patients, may cause a tendency to infectious complications. In some cases, fever may be a symptom of MDS. Sometimes patients consult a doctor due to a tendency to bleeding due to a decrease in the number of platelets.
In 20% of patients with one of the variants of MDS - chronic myelomonocytic leukemia - there is an increase in the size of the liver and (or) spleen .
Somewhat less frequently, there is enlargement of the lymph nodes . Enlargement of the liver and lymph nodes is rare in other types of MDS.
Diagnostics
Detection of MDS is based on the detection of signs of dysplasia (disturbances in tissue formation) in one or more hematopoietic lineages.
At the same time, the identified changes can be extremely diverse. The ratio of normal and altered cells varies significantly in different patients.
Cell lines (hematopoietic germs) are considered to be altered if the number of cells with signs of dysplasia is more than 10%.
If the number of altered cells in the bone marrow is small (less than 10%), a cytogenetic study must be performed to reliably diagnose MDS.
Prognostic factors
The prognosis (outcome) of MDS depends on many factors.
Life expectancy and the likelihood of transformation (transition) to acute leukemia in MDS vary significantly.
The shortest life expectancy (5-7 months) is observed in patients with MDS caused by chemotherapy and radiation. In addition, the prognosis is less favorable in patients over 60 years of age, male gender and in the presence of symptoms of intoxication.
Among blood parameters, unfavorable prognostic signs include:
- hemoglobin level below 10 g/dl
- platelet count less than 100,000 per cubic ml
- more than 5% blast (tumor) cells
- elevated levels of LDH (lactate dehydrogenase), etc.
The degree of tumor infiltration (damage) of the bone marrow has the greatest prognostic significance. The prognosis is less favorable if the number of tumor cells in the bone marrow exceeds 10%. Some identified chromosomal changes also negatively affect the outcome of the disease.
Myelodysplastic syndrome (MDS). Course of the disease
Patients gradually lose more and more strength. The value of hemoglobin and hematocrit, that is, a value that mainly depends on the concentration of red blood cells and on the distribution of solid and liquid components, decreases sharply. Doctors try to stop this trend with weekly blood transfusions or by injecting erythropoietin once a week (a hormone made in the kidneys that stimulates the formation of red blood cells in the bone marrow). At the same time, the number of platelets, responsible for blood coagulation, and the number of leukocytes, responsible for immune defense, are significantly reduced. As a result, patients with MDS are increasingly suffering from sudden bleeding in the gums, nose and, most dangerously, in the stomach and intestines. During the course of the disease, hematomas develop throughout the body. In addition, patients are extremely vulnerable to all types of infections and should avoid crowds. Most patients with MDS die from internal bleeding or pneumonia because they no longer respond to even strong antibiotics. In approximately 30% of all cases of MDS, it suddenly progresses to a state of acute leukemia, during which many patients do not survive even if chemotherapy is started immediately (due to their weakened condition).