Causes of atonic constipation
The causes of atonic constipation include the following factors:
- abnormalities of intestinal development;
- diseases of the endocrine system, changes in hormone levels (during pregnancy, menopause, etc.);
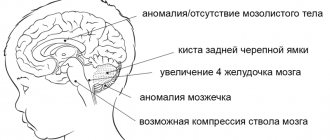
- neurological disorders;
- spinal cord injuries;
- taking medications that affect intestinal motility.
The cause of atonic constipation is a sedentary lifestyle. It is not necessary to have a sedentary job - atonic constipation also occurs after injuries and operations, when it is necessary to adhere to bed rest. Other possible causes include intoxication, exacerbation of inflammatory diseases, depression, bad habits, and infectious diseases.
A number of medications change muscle tone; antispasmodics, analgesics, antidepressants, some hormonal drugs, and medications that affect the transmission of nerve impulses can weaken it.
So-called idiopathic constipation has no known cause. Atonic constipation is often idiopathic in nature.
It is believed that intestinal dyskinesia is characteristic of functional constipation and irritable bowel syndrome with their predominance. But the slow movement of contents through the colon is associated with pathologies of the muscles and nervous system. There are two criteria by which an inert, or lazy, bowel is determined: resistance to laxatives and instrumental confirmation of slowing.
Intestinal hypotension. Colon hypotension Intestinal hypotension symptoms
Medicine uses a multifaceted approach to treatment so that hypotension of the large intestine and small intestine regresses and does not contribute to the further formation and development of more complex diseases. In order for the treatment to be effective, physiotherapeutic procedures are prescribed:
- electrophoresis using antispasmodic drugs;
- diathermy;
- ozokerite, with paraffin, from the belly side.
Early examination and treatment prevents the development of more serious diseases that require surgery or pose a threat to healthy functioning
In this case, the following indications are made and dietary changes that should be observed:
| Daily use of foods rich in fiber, which stimulates peristalsis: |
|
| It is necessary to exclude products that create the effect of strong fermentation and cause flatulence: |
|
Pharmacy medications are prescribed:
| Bisacodyl, Guttalax | Responsible for stool stimulation. |
| Platiphylline, Atropine | Act as anticholinergics. |
| Ephedrine | It is an adrenergic agonist. |
| Phytipreparations: Senade, Tisasen | Treat constipation caused by hypotension and sluggish peristalsis of the large intestine, regulate the frequency of stool. |
The attending physician tells you everything that is recommended to know about the disease. Discusses all indications and contraindications with the patient.
https://www.youtube.com/watch?v=K823hXfijhw
Hypotony and atony of the uterus
may lead to its removal if proper treatment is not carried out.
You can learn from here why low blood pressure is dangerous for teenagers.
You will find a description of kidney hypotension in a newborn here.
Gastric atony
Stomach atony is a rather rare disease, but it is one of the most dangerous diseases due to its rapidly increasing symptoms. It manifests itself in the weakening or absence of tone of the muscles that are located in the wall of the stomach and are responsible for its peristalsis. Therefore, when you notice the first symptoms, you should immediately contact a specialist.
Causes
The disease develops reflexively or as a result of damage to the nerve cells of the organ. Also, predisposing factors may be:
- prolonged and excessive overeating or drinking;
- exhaustion of the body;
- myocardial infarction;
- peritonitis;
- pneumonia;
- some serious illnesses;
- surgical intervention;
- infections;
- damage to the intestines and stomach;
- severe fatigue;
- depressed mental state.
Diagnostics
Atony can only be diagnosed using fluoroscopy. The stomach has a characteristic shape with a wide lower part and a narrow tube in the body, and peristaltic contractions are either noticeably weakened or absent completely.
When it enters the stomach, the contrast agent is not retained and enters the lower section. Analysis is also collected.
The nature and content of vomiting is of great importance for the diagnosis of this disease; with atony, a large amount of hydrochloric acid will be observed in it.
There is a disease called gastric hypotension. Its symptoms are similar to atony and you should be extremely careful when diagnosing it. As with atony, muscle tone in the walls of the stomach decreases, and the motor function of the stomach is also impaired.
The causes of hypotension are divided into two types. One of the causes of the disease lies in the stomach itself, and the second - in other diseases of the body. Hypotension can occur when:
- Stress, nervous tension.
- Mechanical injuries.
- Frequent and active sexual activity. Menstrual dysfunction in women.
- Chronic infections and intoxication of the body.
- Chronic diseases leading to a sedentary lifestyle.
- Potassium deficiency. Metabolic disorders.
- Asthenic body type.
- Prolapse of the stomach (gastroptosis).
- Fast fatiguability.
- Weakness.
- Sleep disturbance.
- Absent-mindedness.
- Quick satiety when eating food.
- Chronic constipation.
- Flatulence.
- Sometimes - increased appetite.
Symptoms
There are mild and severe forms of the disease. The mild form is characterized by heaviness and fullness in the epigastric region after eating. After eating, the contours of the stomach may be clearly visible through the flabby muscles of the abdominal wall. The patient’s health deteriorates especially clearly after excessive consumption of food or drink. Also possible:
- belching food or air;
- decreased appetite;
- Blunt pain;
- hiccups;
- bad breath;
- nausea or vomiting (distinguished by a greenish tint).
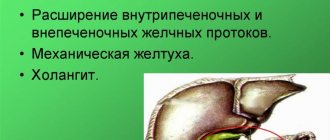
The disease is recurrent and long-lasting. Due to frequent stagnation of food in the stomach, complications arise, leading to inflammatory processes in the organs of the gastrointestinal tract, pancreas and biliary tract. Very often, atony is accompanied by diseases such as gastroptosis and gastritis. nervous dyspepsia.
The severe form is marked by acute or chronic gastric obstruction.
Treatment
First of all, it is strengthening the general condition of the body and nervous system. Organization and regulation of mental work and the working day. And also a mandatory diet. For patients with atony it is recommended:
- limit drinking;
- frequent meals in crushed form and in small quantities;
- separate solid and liquid meals;
Also, the diet contains sufficient amounts of vitamins and the food should be particularly nutritious. Patients with atony, and especially if gastroptosis is associated with it, in addition to diet, should wear a bandage to strengthen the abdominal walls.
Among the medications for gastric atony, Passazhix is an antiemetic dopamine receptor blocker and Metoclopramide, a centrally acting dopamine receptor antagonist. The second remedy is also an antiemetic.
To regulate bowel function, it is recommended to eat foods such as:
In the fight against the disease, it will be important to strengthen the abdominal muscles, for this you should pay attention to physical therapy. Together, this will raise the overall tone of the body.
Water therapy is very good for treatment. If possible, the patient should be sent to the mountains, village or to the seashore.
Prevention
To prevent gastric atony, light sports and a normal diet are recommended. An example of a set of exercises is given below.
What is intestinal atony?
A fairly common disease is intestinal atony.
, the symptoms and treatment of which are familiar to gastroenterologists in large cities.
According to medical statistics, it is in megacities that the majority of patients with this diagnosis live.
They lead a sedentary lifestyle, consume refined foods and fast food, are constantly overtired, do not get enough sleep, and experience stress. These are just some of the factors that can cause disruption of intestinal motility.
Intestinal atony: what is it and how does it occur?
This is a decrease in the tone of the intestinal muscles, in which their ability to contract decreases or completely disappears.
As a result, the functionality of the intestines decreases: food is still digested and useful components are absorbed, but the movement of food through the intestines is difficult. As a result, fecal stagnation and constipation occur. This leads to the accumulation of waste and fecal stones.
Stagnation of undigested food is a rather serious problem.
Firstly, fermentation begins in the intestines, which is accompanied by the release of a large amount of gases and irritation of the mucous membrane.
Secondly, irritation of the mucous membrane by toxins and bacterial activity cause inflammation (slight inflammation occurs already on the 2-3rd day of irregular bowel movements), which becomes chronic over time.
Thirdly, the components formed as a result of fermentation and rotting of food are partially absorbed into the blood, causing general intoxication of the body.
https://www..com/watch?v=xIOXj0hJhyQ
Normally, the intestinal muscles contract approximately 18 times per minute. With atony, the number of contractions decreases to several units per minute, in the worst case, disappears altogether.
Symptoms of atonic constipation
Symptoms include bloating, flatulence, abdominal pain, intestinal colic, and absence of intermediate urges between bowel movements. Researchers Shulpekova and Ivashkin in their scientific work indicate that “hypotonic or atonic functional constipation is associated with loss of tone of the colon. In this case, the delay in defecation can reach 5–7 days, the feces can be large in volume and loose in consistency” (Shulpekova, Ivashkin, 2004, p. 49).
However, this does not mean that dry and dense, fragmented feces cannot be observed. Stagnation of feces leads to the absorption of water from them, as a result of which the consistency of the stool changes. Often the act of defecation is accompanied by severe pain.
The characteristic symptoms of atonic constipation include the following:
- Bloating, flatulence. They develop against the background of stagnation of feces and excessive absorption of water from them.
- Pain in different parts of the abdomen. Often associated with gas formation, they can resemble intestinal colic - they appear periodically, without clear localization.
- Absence of intermediate urges between acts of defecation.
- Pain in the rectum. From time to time, due to overstretching of the rectal ampulla, cramping pain may occur.
There is a high probability of developing proctological complications, so blood and mucus are often present in the stool. If such symptoms occur, you should consult a doctor immediately.
Other symptoms are associated with general intoxication of the body with feces. Increased absorption of toxins in the colon leads to fatigue, pale skin, sweating, dizziness, decreased appetite, and nausea. These are nonspecific manifestations of poisoning, so they can persist for many years, and the person simply has no idea what is causing this feeling.
Intestinal hypotension: causes, symptoms and treatment
The intestinal tract most often suffers from various ailments. The thing is that all food products that a person ingests pass through the digestive system. One of the unpleasant ailments is intestinal hypotension. What is this disease and can it be cured? We'll tell you.
The concept of hypotension and the reasons for its development
Intestinal hypotension refers to one of the processes in which there is a decrease in digestive motility and impaired fecal output. During normal functioning of the organ, defecation should occur 1-2 times in two days.
With hypotension, this period increases to 3-5 days. Then doctors talk about the manifestation of chronic constipation.
Colon hypotension can develop for several reasons due to:
- leading an unhealthy lifestyle;
- presence of harmful habits such as smoking and drinking alcohol;
- poor nutrition, where fatty, fried, spicy, refined foods predominate;
- the presence of congenital anomalies in the digestive system;
- formation of adhesions in the abdominal area;
- stenosis of various areas in the large intestine, which manifests itself against the background of the appearance of a tumor-like formation;
- long fasting. This process is observed during weight loss;
- sedentary lifestyle;
- lack of physical activity;
- constant stressful situations and nervous overstrain;
- unusual place and conditions for the act of bowel movement;
- diseases that are associated with the endocrine system. These include hypothyroidism, hyperthyroidism, diabetes mellitus, acromegaly;
- acquired diseases of the digestive system. These include gastritis, colitis, pancreatitis, enterocolitis;
- diseases in the rectum. These include diseases in the form of fissures in the anal area, hemorrhoids, proctitis, paraproctitis;
- diseases of the urinary and reproductive system in the form of kidney hypotension, menstrual irregularities in the female half of the population;
- prostate adenoma and prostatitis in men;
- toxic effects of certain drugs and chemicals;
- muscle weakening of the press and muscle structures in the pelvic area;
- disturbance of blood flow in the mesentery of the colon;
- damage to areas of the nervous system in the brain and spinal cord that are responsible for regulating the activity of the intestinal tract;
- long-term course of dysbacteriosis.
The main cause of this disease is considered to be poor nutrition. Therefore, in order to regulate the functionality of the organ, doctors advise starting with nutrition. You should follow a strict diet for some time. Daily stressful situations also have a negative impact on the organ. This factor can lead not only to hypotension, but also to other, more serious complications.
Symptoms of intestinal hypotension
Hypotension of the colon can occur regularly or with a certain periodicity. It all depends on the characteristics of the organism, the course of the disease and the decisive factor.
The most important symptom of the disease is considered to be infrequent bowel movements. At the same time, a change in the shape of feces is also observed. They become dense and resemble the shape of balls. White veins may be present.
Also, if intestinal hypotension is diagnosed, the symptoms will be accompanied by:
- bleeding after bowel movement;
- lack of appetite;
- insomnia;
- painful sensations in the head;
- bloating and colic;
- tachycardia;
- sweating at night;
- weakening of the body;
- chronic fatigue;
- irritation.
Symptoms and treatment of hypotension should be determined as soon as possible. If the first signs appear, do not delay visiting the doctor. If you start treatment on time, you can prevent the development of serious complications.
Diagnosis of hypotension
Few people know what hypotension of the large intestine is. At first glance, it seems that the problem can be solved with the help of laxatives. But the organ quickly gets used to this state and becomes lazy.
When the first symptoms occur, you should immediately visit a doctor. He will listen to the patient’s complaints and prescribe an examination.
It includes:
- examination and palpation of the abdominal area;
- radiography using a contrast agent. This will allow you to see the condition of the intestinal tract in appearance. Perhaps the cause of hypotension was a tumor or other pathology;
- performing colonoscopy and sigmoidoscopy. Such research techniques help to examine the organ from the inside and assess the condition of the mucous membrane;
- taking material for histology to determine cancer cells;
- a study to assess the motor functionality of the digestive tract.
Once the diagnosis is confirmed, the patient is prescribed treatment.
Treatment of intestinal hypotension
How to cure hypotension of the stomach and intestines? All therapeutic measures are prescribed only by the attending physician after a detailed examination. To eliminate the disease, it is necessary to identify the cause, then all measures will lead to recovery.
For intestinal hypotension, treatment is based on the following:
- following a strict diet. You need to include a lot of plant fiber in your diet. It is included in vegetables and fruits, wholemeal bread, herbs, fresh juices, buckwheat and dairy products. Don't forget about vegetable fats. Before consuming food, you should drink a spoonful of olive, sunflower, or flaxseed oil;
- exclusion from the menu of fatty, fried, spicy foods. It is also worth giving up foods that cause gas formation in the form of beans, peas, apples, grapes, radishes, garlic, onions, bread made from premium flour, fatty meat and fish;
- Drinking cool water after waking up before eating. Instead of water, you can take juice from vegetables and fruits. You should also add half a teaspoon of salt to these drinks;
- performing physical exercises. They strengthen muscle structures and activate the intestinal tract. Gymnastics that imitates cycling will bring benefits;
- swimming lesson. You need to visit the pool at least twice a week;
- taking daily walks after work for at least thirty to forty minutes;
- carrying out drug therapy. Hypotension should be treated with drugs that stimulate bowel movements. This includes laxatives in the form of Guttalax. Anticholinergics and adrenergic agonists are also prescribed. Their effect is aimed at stimulating the functioning of the intestinal tract directly from the brain. In stressful situations, sedatives are prescribed. For pain, antispasmodics are prescribed;
- performing physical procedures. The patient may be prescribed electrophoresis with the use of antispasmodics, diathermy, paraffin therapy, and a cool shower;
- use of traditional methods. The patient can take herbal decoctions of chamomile, calendula, and sage instead of tea. They have a pronounced anti-inflammatory and calming effect.
To normalize the intestinal flora, bifidobacteria and lactobacilli are used.
Pathology must be treated under the supervision of a doctor. If you do nothing for a long time, various complications may occur.
Tips and tricks
Source: https://zivot.ru/kishechnik/gipotoniya.html
Complications of constipation
Atonic constipation, like other types of bowel movement disorders, can lead to serious complications. In the long term, they affect the health of the cardiovascular system, increase the risk of strokes and heart attacks, malignant intestinal tumors, reduce resistance to infections, and stimulate the exacerbation of allergic diseases.
Complications such as hemorrhoids, anal fissures, proctitis and paraproctitis can occur even against the background of one episode of constipation if there is a predisposition.
Quite quickly, against the background of prolonged constipation, dysbiosis develops - a change in the balance of intestinal microflora can further aggravate the problem, lead to a deficiency of vitamins and minerals, and a general weakening of the body. Therefore, it is important to consult a doctor in a timely manner to correct the problem.
Why is inflammation of the intestinal walls dangerous?
Recently, the number of Russians diagnosed with IBD has increased annually by an average of 10–12%. Most often, residents of modern megacities suffer from ulcerative colitis and Crohn's disease. In the first case, the mucous membrane of the colon is affected, and in the second, the end of the small intestine and the beginning of the large intestine. Inflammation leads to the formation of bleeding ulcers and progresses rapidly, leading to irreversible tissue damage if undiagnosed and treated.
- Patients with Crohn's disease have a significantly increased risk of intestinal obstruction and, as a result, fistula formation.
- Massive bleeding in ulcerative colitis can cause intestinal perforation and life-threatening peritonitis.
- Finally, IBD is recognized as one of the factors that significantly increases the likelihood of tumor formation in the intestine.
Even at the initial stage, intestinal diseases manifest themselves with unpleasant symptoms that significantly reduce the quality of life.
Features of treatment
Treatment of atonic constipation is complex. There are several approaches to drug therapy:
- motility regulators, enterokinetics, and other agents. They allow you to regulate intestinal motility by correcting the tone of the intestinal muscles.
- Drugs that indirectly affect the digestive system. This approach is used when atony is caused by other diseases. Medication support and correction can improve bowel function.
- Symptomatic therapy: laxatives for immediate relief, medications to eliminate symptoms of intoxication, painkillers. Such remedies complement the main course of treatment or other measures to normalize intestinal function.
It should be understood that basic and symptomatic treatment should be prescribed by a specialist. One of the main mistakes many people make is trying to help themselves with symptomatic treatment, laxatives or cleansing enemas, without undergoing examinations. Why is this an error? The choice of laxative should take into account the option of chronic constipation.
Doctors try not to prescribe laxatives that chemically stimulate peristalsis. Parfenov V.I. in his article explains why “the main disadvantage of the listed laxatives is the rather rapid addiction to them, the need to gradually increase the dose, significantly exceeding the permissible, and, as a consequence, degeneration of the mechanoreceptors of the colon” (Parfenov, 2013, p. 100 ).
But not only chemical laxatives can be addictive when taken over a long period of time. You should be especially careful with any senna-based laxatives, as prolonged use leads to addiction and the need to constantly increase the dosage to achieve a positive effect.
Regular use of cleansing enemas will also lead to the appearance of an inert colon - a lack of urge to defecate and worsening the problem.
Laxatives, which increase the volume of intestinal contents and osmotic pressure, are not addictive and can be used for constipation. But many patients require discontinuation of treatment due to bloating, painful cramps and other possible side effects.
Principles of effective treatment:
- competent selection of laxatives in accordance with the type of constipation;
- refusal of self-medication;
- following doctor's orders.
One of the non-addictive laxatives is Fitomucil Norm. It contains soluble and insoluble dietary fiber - the shell of psyllium seeds and the pulp of homemade plum fruits. The English drug acts gently and predictably, helping to restore normal stool. "Fitomucil Norm" does not cause side effects in the form of spasms, pain, false and repeated urges to defecate. Psyllium absorbs water, turning into a gel, which allows you to gently remove feces. Insoluble fiber stimulates intestinal motility. Long-term use of the drug is allowed in consultation with a doctor.
Symptoms and treatment of atonic constipation are always strictly individual: it is important to determine the cause of the disorder and correct it. To do this, the doctor will prescribe a comprehensive diagnosis. You may need to consult other specialists: endocrinologist, neurologist.
Motility disorders of the digestive organs and general principles of their correction
Almost any disease of the digestive organs is accompanied by a violation of their motor function. In some cases they determine the nature of clinical manifestations, in others they hide in the background, but are almost always present. And this is natural, since the nature of motor activity is under control and in close connection with the state of the digestive organs, as well as under the control of nervous and humoral mechanisms of a higher level.
All conditions associated with impaired motility of the digestive organs can be divided into two large groups. In the first case, the disorders in question are associated with a pathological process in one or another part of the digestive system, for example, with duodenal ulcer or colitis. Motility can change when the intestine is compressed from the outside, there is an obstacle in its lumen, or the volume of its contents increases, as, for example, observed with osmotic diarrhea. In other cases, motor skills change due to a violation of its regulation by the nervous or endocrine systems. This group of diseases is called functional, which emphasizes the secondary nature and reversibility of developing changes. At the same time, long-term functional disorders of the motility of the digestive organs sooner or later lead to their “organic” damage. Thus, functional gastroesophageal reflux can cause reflux esophagitis, that is, lead to the formation of gastroesophageal reflux disease, and irritable bowel syndrome can lead to the development of chronic colitis. Thus, the favorable course of functional disorders, which is emphasized by the Rome criteria, is such only over a certain time period. It should also be emphasized that functional diseases are especially relevant for pediatric practice, since they make up the vast majority of all diseases of the digestive system in children. The prevalence of functional disorders in the structure of gastrointestinal tract diseases in children is not only high, but continues to grow every year. Thus, functional dyspepsia syndrome is observed in 30–40% of cases, chronic duodenal obstruction in 3–17% [1].
All motor disorders of the digestive tube can be grouped as follows:
- Change in propulsive activity:
- – decrease – increase.
- Changes in sphincter tone:
- – decrease – increase.
- The appearance of retrograde motility.
- The emergence of a pressure gradient in adjacent parts of the digestive tract.
The clinical symptoms of motility disorders of the digestive organs are diverse and depend on the localization of the process, its nature and the root cause. They can manifest as diarrhea or constipation, vomiting, regurgitation, abdominal pain or discomfort and many other complaints.
The patient’s somatic symptoms (complaints) are essentially the interpretation by the human mental sphere of information from receptors located in the internal organs. Its formation is influenced not only by the pathological process as such, but also by the characteristics of the nervous system and mental organization of the patient. The actual complaint presented to the doctor in this way is determined by the nature of the pathology, the sensitivity of the receptors, the characteristics of the conduction system and, finally, the interpretation of information from the organs at the level of the cerebral cortex. At the same time, the last link often has a decisive influence on the nature of complaints, leveling them in some cases and aggravating them in others, as well as giving them an individual emotional coloring.
The flow of impulses from peripheral receptors is determined by the level of their sensitivity or hypersensitivity to the action of damaging stimuli, manifested by a decrease in the threshold of their activation, an increase in the frequency and duration of impulses in nerve fibers with an increase in the afferent nociceptive flow. In this case, stimuli that are insignificant in strength (for example, stretching of the intestinal wall) can provoke an intense flow of impulses into the central parts of the nervous system, creating an image of a severe lesion with a corresponding autonomic response.
Thus, we can distinguish three levels of formation of a somatic symptom (complaint), for example pain: organ, nervous, mental. The symptom generator can be located at any level, but the formation of an emotionally charged complaint occurs only at the level of mental activity. In this case, a pain complaint generated without damage to the organ may not differ in any way from one that arose as a result of true damage.
As in the case of pain, complaints associated with impaired motility of the gastrointestinal tract can be formed at the level of the affected organ (stomach, intestines, etc.), associated with a violation of the regulation of these organs by the nervous system, but can also be generated regardless of the state of the organ, due to the peculiarities of the patient’s psycho-emotional organization. Compared to the mechanism of pain, the difference is associated only with the direction of nerve impulses: in the case of pain, there is an “ascending” direction, and the overlying level can become the generator of the complaint without the participation of the underlying one, while in the case of impaired motility of the gastrointestinal tract, the opposite situation is observed: “descending” impulse with the possibility of generating a symptom by the underlying organ without the participation of the overlying one. Finally, it is possible to generate a descending stimulus at the segmental level in response to a pathological ascending impulse, for example, with receptor hyperreactivity. Mechanisms associated with a decrease in the sensitivity threshold of intestinal receptors in combination with its stimulation by upper regulatory centers, activated against the background of psychosocial influences, are observed, in particular, with irritable bowel syndrome.
Thus, any symptom (complaint) becomes such only when scattered nerve impulses are processed by higher departments. A true somatic complaint is determined by damage to one or another internal organ, and various parts of the nervous system perform the functions of a connecting link and primary data processing, transmitting the latter to the mental level or in the opposite direction. At the same time, the generator of somatic-like complaints can be the nervous system itself and its higher parts. At the same time, the mental level is absolutely self-sufficient and here complaints can “emerge” that do not have their prototype at the somatic level, but are indistinguishable from true somatic symptoms. It is these mechanisms that underlie functional motor disorders. Differentiation of the primary level of the symptom (complaint) is of fundamental importance for the correct diagnosis and selection of the optimal treatment plan.
Disturbances in the motility of the digestive organs of any origin inevitably cause secondary changes, the main ones of which are disturbances in the processes of digestion and absorption, as well as disturbances in the intestinal microbiocenosis. The listed disorders aggravate motor disorders, closing the pathogenetic “vicious circle” [2].
The digestive organs have electrical activity that determines the rhythm and intensity of muscle contractions and motor skills in general. The question of the localization of the electrical pacemaker of the gastrointestinal tract remains open. Studies have shown that the pacemaker of the stomach is located in the proximal part of the greater curvature, and for the small intestine this role is played by the proximal duodenum (some authors localize it in the area of the confluence of the common bile duct), which generates slow electrical waves that are the highest for the entire small intestine frequencies. In addition, it has been proven that any zone of the gastrointestinal tract is a source of rhythm for caudally located segments or becomes so under certain conditions. The speed of propagation of the basic electrical rhythm in different parts of the gastrointestinal tract is not the same and depends on its functional state and the pacemaker. For the stomach, it ranges from 0.3–0.5 cm/sec (in the fundus) to 1.4–4.0 cm/sec (in the antrum). It should be noted that there is always a gradient of both the basic electrical rhythm and the rhythmic contractions of the smooth muscles of the gastrointestinal tract in terms of the frequency and speed of excitation in the caudal direction [3, 4, 5, 6].
To assess the nature of the motility of the digestive organs, X-ray (contrast) and electrophysiological research methods (electrogastroenteromyography) can be used. The latter have now received a new impetus for development and implementation on the basis of a new technical base and computer technologies, which have made it possible to carry out complex mathematical analysis of the obtained data in real time. The method is based on recording the electrical activity of the digestive organs.
Correction of motility disorders of the digestive organs comes down to solving three problems:
- treating the underlying cause;
- correction of actual motor disorders;
- correction of secondary changes that arose against the background of dyskinesia of the gastrointestinal tract.
Since the root cause of functional disorders is most often a violation of the nervous regulation of the digestive organs, the first task in this case should be solved by gastroenterologists in close contact with neurologists, psychoneurologists and psychologists after a thorough examination of the patient [7]. In the case of primary pathology of the digestive organs, for example with a peptic ulcer, treatment of the underlying disease comes first.
The second problem is solved by prescribing postural therapy, nutritional correction and medications. Postural therapy is most important in the correction of gastroesophageal reflux. It is recommended to ensure an elevated position of the head end of the patient's bed, avoid tight clothing and tight belts, physical exercises associated with overstraining the abdominal muscles, deep bends, prolonged stay in a bent position, lifting weights of more than 8-10 kg with both hands. Infants should be placed in an upright position during feeding and immediately after feeding. In the diet, you should limit or reduce the content of animal fats, increase the protein content, avoid irritating foods, carbonated drinks, reduce the single volume (you can increase the frequency) of food intake. In addition, you should not eat before bed. Obese patients are advised to lose weight. These and some other problems in infants are solved by prescribing special antireflux mixtures. If possible, you should avoid taking drugs that reduce the tone of the lower esophageal sphincter, including sedatives, hypnotics, tranquilizers, theophylline, anticholinergics, beta-agonists. If you smoke, you must stop.
In case of intestinal pathology, poorly tolerated foods (causing pain, dyspepsia) and promoting gas formation are excluded: fatty foods, chocolate, legumes (peas, beans, lentils), cabbage, milk, brown bread, potatoes, carbonated drinks, kvass, grapes, raisins. Fresh vegetables and fruits are limited. Other foods and dishes are prescribed depending on the predominance of diarrhea or constipation in the clinical picture.
In general, the diet is determined by the underlying disease.
For the purpose of drug correction of the motility of the digestive organs, prokinetics and antispasmodics are used. The list of prokinetics used by domestic gastroenterologists is relatively small. These include metoclopramide, domperidone and trimebutine.
The action of domperidone (Motilium), as well as metoclopramide (Cerucal, Reglan), is associated with their antagonism towards dopamine receptors of the gastrointestinal tract and, as a result, increased cholinergic stimulation, leading to increased sphincter tone and accelerated motility. Unlike domperidone, metoclopramide penetrates well through the blood-brain barrier and can cause serious side effects (extrapyramidal disorders, drowsiness, fatigue, anxiety, as well as galactorrhea associated with an increase in prolactin levels in the blood), which makes it necessary to avoid its use in pediatric practice. The only situation when metoclopramide is indispensable is emergency relief of vomiting, since other prokinetics are not available in injectable forms. Motilium is prescribed at a dose of 2.5 mg per 10 kg of body weight 3 times a day for 1–2 months. Side effects of Motilium (headache, general fatigue) are rare (in 0.5–1.8% of patients).
The effect on motor skills and the possibility of using somatostatin analogs (octreotide) for functional disorders in both adults and children are also being studied. Somatostatin has been shown to reduce gastrointestinal motility and can be used successfully in a number of functional disorders, but specific indications and route of administration have not yet been developed [8, 9].
Loperamide (Imodium) occupies a special place among drugs that affect motility. The point of pharmacological application of this drug is the opiate receptors of the colon, the effect on which leads to a significant, dose-dependent, more pronounced slowdown of motility compared to trimebutine. Loperamide is a highly effective symptomatic antidiarrheal agent and can be used in combination with other drugs. Its use should be quite careful, because against the background of slowing motility, intestinal absorption increases, which can lead to severe intoxication, especially in patients with infectious diarrhea or severe intestinal dysbiosis.
In many cases, in addition to disturbances in propulsive activity, sphincter spasm occurs. In these cases, antispasmodics become the key drugs, not only normalizing muscle tone, but also eliminating pain. Several groups of drugs have antispasmodic effects on the digestive organs. These include M-anticholinergics (starting with atropine, which has gone out of clinical practice), myotropic antispasmodics acting through the suppression of phosphodiesterase (for example, drotaverine (No-shpa)), a selective blocker of calcium channels of intestinal cells (pinaverium bromide (Dicetel)) and a highly effective modulator Na+- and K+-channels (mebeverine (Duspatalin)).
Drotaverine, by inhibiting phosphodiesterase IV, increases cAMP concentrations in myocytes, which leads to inactivation of myosin kinase, inhibits the connection of myosin with actin, reducing the contractile activity of smooth muscles, and promotes relaxation of sphincters and a decrease in the force of muscle contractions.
Pinaveria bromide (Dicetel) blocks voltage-dependent calcium channels of intestinal myocytes, sharply reducing the entry of extracellular calcium ions into the cell and thereby preventing muscle contraction. Features of the drug are its selectivity for the digestive organs, including the biliary tract, as well as the ability to reduce visceral sensitivity without affecting other organs and systems, including the cardiovascular system.
A special feature of mebeverine (Duspatalin) is its dual action. On the one hand, it blocks fast Na+ channels, preventing depolarization of the muscle cell membrane and the development of spasm, while disrupting the transmission of impulses from cholinergic receptors. On the other hand, mebeverine blocks the filling of Ca++ depots, depleting them and thereby limiting the release of K+ from the cell, which prevents the development of hypotension. Thus, mebeverine has a modulating effect on the sphincters of the digestive organs, which not only relieves spasms, but also prevents excessive relaxation. A special feature of Duspatalin is its release form: 200 mg of mebeverine are enclosed in microgranules coated with a pH-sensitive shell, and the microgranules themselves are enclosed in a capsule. In this way, not only the greatest effectiveness of the drug is achieved, but also prolongation of its action over time and throughout the entire gastrointestinal tract. The drug, gradually released from the granules, ensures a uniform effect for 12–13 hours. Duspatalin is prescribed orally 20 minutes before meals, 1 capsule 2 times a day (morning and evening).
Mebeverine has been produced since 1965, and many years of experience in its use have shown not only the effectiveness of the drug, but also its safety. An important feature of the drug is the absence of anticholinergic effects, which significantly expands the scope of its application.
For flatulence, medications are prescribed that reduce gas formation in the intestines by weakening the surface tension of gas bubbles, leading to their rupture and thereby preventing stretching of the intestinal wall (and, accordingly, the development of pain). Simethicone (Espumizan) and combination drugs can be used: Pankreoflat (pancreatic enzymes + simethicone), Unienzyme with MPS (plant enzymes + sorbent + simethicone).
For constipation, the prescription of laxatives and/or prokinetics is indicated, however, in the latter group of drugs there are no effective drugs approved for use in pediatric practice, and of the laxatives, the most effective and safe drug in all age groups is lactulose (Duphalac).
The main feature of lactulose is its prebiotic effect. Prebiotics are partially or completely indigestible food components that selectively stimulate the growth and/or metabolism of one or more groups of microorganisms living in the large intestine, ensuring the normal composition of the intestinal microbiocenosis. From a biochemical point of view, this group of nutrients includes polysaccharides and some oligo- and disaccharides.
As a result of microbial metabolism of prebiotics in the colon, lactic acid, short-chain fatty acids, carbon dioxide, hydrogen, and water are formed. Carbon dioxide is largely converted into acetate, hydrogen is absorbed and excreted through the lungs, and organic acids are utilized by the macroorganism, and their importance for humans can hardly be overestimated.
Lactulose is a disaccharide consisting of galactose and fructose. Its prebiotic effect has been proven in numerous studies. Thus, in a randomized, double-blind, controlled study on 16 healthy volunteers (10 g/day of lactulose for 6 weeks), a significant increase in the number of bifidobacteria in the colon was shown [10].
The laxative effect of lactulose is directly related to its prebiotic effect and is due to a significant increase in the volume of colon contents (by approximately 30%) due to an increase in the bacterial population. An increase in the production of short-chain fatty acids by intestinal bacteria normalizes the trophism of the colon epithelium, improves its microcirculation, ensuring effective motility, absorption of water, magnesium and calcium. The incidence of side effects of lactulose is significantly lower compared to other laxatives and does not exceed 5%, and in most cases they can be considered minor. The safety of lactulose determines the possibility of its use even in premature infants, proven in clinical trials [11, 12].
The dose of lactulose (Duphalac) is selected individually, starting with 5 ml once a day. If there is no effect, the dose is gradually increased (by 5 ml every 3-4 days) until the desired effect is obtained. Conventionally, the maximum dose can be considered in children under 5 years old 30 ml per day, in children 6–12 years old - 40–50 ml per day, in children over 12 years old and adults - 60 ml per day. The frequency of administration can be 1-2 (less often - 3) times a day. A course of lactulose is prescribed for 1–2 months, and, if necessary, for a longer period. The drug is discontinued gradually under control of stool frequency and consistency.
Adsorbents, among which Smecta occupies the first place, also regulate motility to a certain extent. It is important that smectite (the active principle of the drug Smecta), in addition to the direct adsorbing effect, has mucocytoprotective properties and helps slow motility and has a beneficial effect on the composition of the intestinal microflora, being a synergist of probiotics.
The third task in the correction of motility disorders is to influence the disorders that arise against the background of dyskinesia of the digestive tract. Motility disorders (both slowing and accelerating) lead to disruption of the normal processes of digestion and absorption and changes in the composition of the internal environment of the intestine. A change in the composition of the internal environment in the intestine affects the composition of the microflora with the development of dysbacteriosis, and also aggravates existing disorders of the digestive processes, in particular, due to changes in the pH of the intestinal contents. In the future, damage to the epithelium and the development of an inflammatory process are possible, marking the transition from functional disorders to a disease with a well-defined morphological substrate. Thus, on the one hand, to correct impaired motility, it is advisable to use drugs with prebiotic activity (including lactulose), and, on the other hand, in the complex treatment of functional disorders of the digestive tract, if necessary, drugs of pancreatic enzymes should be included ( preferably highly effective microspherical, for example, Creon), adsorbents (Smecta), probiotics (Bifidum-bacterin forte and similar).
In general, the determination of the composition of therapy should be strictly individual, taking into account the pathogenetic features of the process in a particular patient with mandatory correction of the root cause of digestive motility disorders.
Literature
- Handbook of pediatric gastroenterology. Ed. A. M. Zaprudnova, A. I. Volkova. M.: Medicine, 1995.
- Belmer S.V., Khavkin A.I., Gasilina T.V. Functional disorders of the digestive organs in children. Educational and methodological manual. M., 2006. 42 p.
- Ponomareva A.P., Belmer S.V., Karpina L.M. Electromyographic assessment of intestinal motor function in children // Issues of modern pediatrics. 2006. T. 5. No. 6. P. 32–35.
- Klimov P.K., Barashkova G.M. Physiology of the stomach: mechanisms of regulation. L.: Nauka, 1991. pp. 57–69.
- Klimov P.K., Ustinov V.N. Bioelectric activity of smooth muscles of the digestive tract and its connection with contractile activity // Advances in physiological sciences. 1973. T. 4. No. 4. P. 3–33.
- Ustinov V.N. Biopotentials of smooth muscles and contractile activity of the stomach // Physiological Journal of the USSR named after. I. M. Sechenov. 1975. T. 61. No. 4. P. 620–627.
- Clouse RE, Lustman PJ, Geisman RA, Alpers DH Antidepressant therapy in 138 patients with irritable bowel syndrome: a five-year clinical experience // Aliment. Pharmacol. Ther. 1994. Vol. 8. No. 4. P. 409–416.
- Di Lorenzo C., Lucanto C., Flores AF, Idries S., Hyman PE Effect of octreotide on gastrointestinal motility in children with functional gastrointestinal symptoms // J. Pediatr. Gastroenterol. Nutr. 1998. Vol. 27. No. 5: P. 508–512.
- Haruma K., Wiste JA, Camilleri M. Effect of octreotide on gastrointestinal pressure profiles in health and in functional and organic gastrointestinal disorders // Gut. 1994. Vol. 35. No. 8. P. 1064–1069.
- Bouhnik Y., Attar A., Joly FA, Riottot M., Dyard F., Flourie B. Lactulose ingestion increases faecal bifidobacterial counts: a randomized double-blind study in healthy humans // Eur J Clin Nutr. 2004. Vol. 58. No. 3. P. 462–426.
- Gleason W., Figueroa-Colon R., Robinson LH et al. A double-blind, parallel-group, placebo-controlled study of lactulose in the treatment of encopresis in children with chronic constipation // Gastroenterol. 1995. Vol. 108. Suppl. 4. P. A606.
- Belmer S.V. Treatment of constipation in children of the first years of life with lactulose preparations // Children's Doctor. 2001. No. 1. P. 46–48.
S. V. Belmer , Doctor of Medical Sciences, Professor T. V. Gasilina , Candidate of Medical Sciences
RGMU, Moscow
Contact information about the author for correspondence
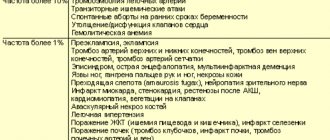
Treatment of medicinal constipation
Atonic constipation may be associated with medications. This effect occurs not only with an overdose, but also as a side effect. We are talking about narcotic analgesics, anticholinergics, hormonal drugs, drugs for normalizing blood pressure, iron supplements, antidepressants, etc.
In some cases, it is advisable to choose an alternative and adjust the treatment regimen for the underlying disease in order to prevent the development of complications from the digestive system. But this should only be done by a doctor.
Therefore, contact a specialist and tell them about the medications you are constantly taking and the associated atonic constipation: he will definitely provide qualified assistance and give recommendations.
Get rid of intestinal problems
The natural British drug is not addictive and works immediately
Find Fitomucil with benefits
IBD in children: growth and development of the body is at risk
Ulcerative colitis in children can appear even before the age of one year and very quickly lead to total damage to the colon. If left untreated, the disease can result in a serious disruption of the physiological process of development of the child’s body: growth retardation or retardation in physical development. If endocrine pathology is not detected, a good pediatrician will definitely prescribe a gastrointestinal tract diagnosis for the child. In addition, this pathology causes serious psychological problems in both children and schoolchildren.
Lifestyle correction
The treatment strategy for atonic constipation is as follows:
- regulation of stool with the help of dietary fiber and water regime (at least 1.5 liters of clean water per day);
- restoration of the lost morning defecation reflex, that is, the habit of emptying the intestines after breakfast;
- maintaining physical activity.
Doctors pay great attention to the psychological state and mood. For example, researchers Marinchuk A. T., Bogatyrev V. G. and others in their work focus on “the need to live with daily morning stool” (Marinchuk, Bogatyrev, Babieva, Koumbatiadis, 2012, p. 53).
You should adjust your daily routine so that going to the toilet in the morning does not become a problem. It is advisable to get up earlier, provide conditions without haste, so that you do not have to restrain the urge.
Symptoms of intestinal diseases: when should you see a doctor?
The disease often manifests itself with intimate symptoms, which the majority of patients try to fight on their own, without rushing to a paid appointment with a proctologist or gastroenterologist. In addition, intestinal inflammation is often accompanied by “masking” symptoms: for example, only stomatitis, as in Crohn's disease, or only inflammation around the anus - perianal dermatitis, or lesions of the eyes or joints. Therefore, the patient often comes to the doctor with a severe form, when the path to recovery turns out to be both longer and more financially expensive.
The following signs should alert anyone:
- frequent diarrhea - up to 15–20 times a day;
- pain and/or cramping in the abdominal area;
- weakness, increased fatigue;
- loss of appetite and noticeable weight loss;
- temperature increase;
- the appearance of traces of blood in the stool.
The likelihood of damage to the large and small intestines is increased in people who regularly and in large quantities consume dark varieties of meat and processed products (sausages, sausage, ham, bacon, etc.). But you should know that adherence to a diet with a predominance of vegetables, fruits, and foods made from whole grains is not a panacea.
A genetic factor plays a certain role: the tendency to intestinal inflammation can be inherited. Among the sick people, people who abuse smoking predominate. Also important are the lack of vitamin D in the body and frequent and uncontrolled self-administration of antipyretic medications.
An appointment with a proctologist in Moscow is recommended not only for people with unstable stools. In order not to fill the army of colorectal cancer patients, even a generally healthy person after 45 years of age should visit a doctor at least once every five years for preventive purposes. The absence of visible signs of inflammation does not exclude the possibility of a hidden disease. Symptoms of intestinal cancer detected at an early stage allow doctors to save the patient and achieve stable remission.
Exercise and physical activity
It is important to increase physical activity: make it a habit to take morning and evening walks, jogging, play sports to the extent physically possible, and swim. If atonic constipation is the result of an injury or a disease of the musculoskeletal system that requires long-term immobilization, then it is important to consult a doctor.
The specialist will develop an exercise program individually, taking into account capabilities and general health. Constant bed rest and complete abstinence from exercise are not indicated in almost any case, except for the most severe ones, so movement is a necessary component of improving the functioning of the gastrointestinal tract.
Exercises such as “bicycle”, leg lifts, and walking are useful. If it is impossible to perform the exercises, you should resort to a kind of passive activity - do a light abdominal massage. Movements should be soft, careful, clockwise.
Colonoscopy of the intestine: are patients’ fears justified?
An illness diagnosed at an early stage creates the least amount of problems for the patient. Therefore, highly informative screening colonoscopy is included in government programs to combat colon cancer in the USA, Israel and European countries. Citizens of developed countries are constantly informed about the need for regular examinations for the prevention and early diagnosis of colorectal cancer.
The specifics of such an intimate procedure do not evoke the most positive emotions among Russians. Pain is a major deterrent even for those people who are fully aware of the need for testing. But is it possible to compare the sensations that arise during a colonoscopy with the torment experienced by patients suffering from already developed oncology!
It should be understood that gentle diagnostic technology, which can be performed under anesthesia, will allow you to avoid dangerous symptoms, frightening diagnoses and a solid set of diagnostic procedures in the future.
Nutrition/diet
Meals should include foods rich in plant fiber and contain fermented milk products. There should be more plant foods than animal products. This will help improve the functioning of the digestive tract, increase the volume and facilitate the excretion of feces. Bran is useful - separately or as part of special bread. These are natural laxatives, just like vegetable oils.
But you should remember: bran is a source of insoluble dietary fiber, the consumption of which in large quantities can provoke increased constipation and increased gas formation. If you are prone to constipation, it is better to pay attention to products containing predominantly soluble dietary fiber.
From the diet you need to exclude foods that thicken the stool and cause increased gas formation:
- potato;
- legumes;
- white bread, pastries;
- spicy dishes;
- smoked meats;
- canned food and marinades;
- chocolate;
- crackers;
- peeled rice, etc.
The daily menu can be based on lean meats, poultry, fish, cereals (except rice and semolina), vegetables, and it is better to steam them. Can be used boiled. Dried fruits have proven themselves to be excellent, especially dried apricots, prunes, and raisins. You can use them on their own or make compotes from them.
Try to limit yourself to six grams of salt per day, otherwise the likelihood of developing fluid retention increases, and swelling is often accompanied by constipation.
It is important to consult a doctor first, especially for people with chronic diseases. The specialist will give precise recommendations regarding the diet.
Foods that cause flatulence
Scientists have proven and repeatedly confirmed the role of nutrition in the occurrence of flatulence2,3.
Products that increase gas formation2,3:
- legumes,
- cabbage,
- spinach,
- sorrel,
- onion and garlic,
- radishes and turnips,
- carrot,
- celery,
- dates,
- bananas,
- apples,
- gooseberry,
- raspberries,
- kvass and beer,
- black bread,
- raisin,
- prunes,
- whole milk,
- carbonated drinks,
- caffeinated drinks,
- alcohol1,3.
Products containing carbohydrates are recognized as dangerous from the point of view of increased gas formation: oligosaccharides, disaccharides, monosaccharides and polyols7. All these carbohydrates are united by the term “FODMAP”, meaning Fermentable Oligo-, Di-, Mono- and Polyol. They are poorly absorbed in the intestine; remaining in it, they become food for bacteria and provoke the development of flatulence with all its inherent symptoms3,7.
FODMAP - foods containing “dangerous” carbohydrates
| Oligosaccharides (fructans and galactans) | vegetables: beets, white cabbage and Brussels sprouts, broccoli and garlic, onions, leeks and shallots, artichokes and asparagus, dill and okra (okra) |
| beans (including green beans), chickpeas, lentils and peas | |
| fruits: apples, watermelons, white peaches, persimmons, rambutan | |
| all cereals made from rye and wheat, as well as products made from them | |
| Disaccharides (lactose) | regular and low-fat cow's milk, goat's milk |
| ice cream made from whole milk and cream | |
| regular and low-fat yogurts | |
| soft cheeses: mozzarella, suluguni, Adyghe, fat cream cheeses | |
| Monosaccharides (fructose) | apples, pears, peaches, watermelon and mangoes, especially in large quantities |
| juices and concentrated sauces from the listed fruits | |
| dried fruits and canned fruits | |
| honey and products containing it | |
| Polyols (sugar alcohols) | fruits: watermelons, apples, pears, plums, prunes, apricots, peaches, nectarines, cherries, avocados, lychees |
| vegetables: all types of cabbage and green peas | |
| mushrooms | |
| sweeteners: isomaltitol, maltitol, mannitol, sorbitol, xylitol, as well as sweeteners ending in “-ol”, such as erythritol |
Up to contents
Types of exercises
Lying on your back
1. Place your hands on your stomach and inhale deeply, pushing it out. As you exhale, draw in your stomach and lightly press on it with your hands.
2. As you inhale, move your hands behind your head and stretch, while simultaneously drawing in your stomach. As you exhale, lower your arms along your body.
3. Alternately bend your knees without lifting your heels from the surface (sliding your feet along the surface).
4. As you exhale, bend your left leg and stretch your knee towards your stomach. Don't help yourself with your hands! Lower your leg and inhale.
5. Repeat the same for the right leg.
6. Repeat the same for both legs at the same time.
7. Bend your knees without lifting your heels off the surface. Then swing your legs left and right.
8. The same, but lifting the heels off the surface.
9. Bend your legs. As you exhale, lift your pelvis off the surface, resting on your shoulder blades and feet. With a sigh, lower your pelvis.
10. Inhale. As you exhale, perform 3-5 circular “bicycle” movements.
11. Inhale. As you exhale, perform 3-4 scissor movements, crossing your straight legs.
12. Inhale. Extend your arms to the sides. As you exhale, rotate your upper body, touching your right hand to your left hand and vice versa. Try to keep only the upper torso off the floor and keep your pelvis in place.
Lying on your right side
13. Right hand under the head, left hand on the stomach, legs bent at the knees. As you inhale, push your stomach out, and as you exhale, pull it in, helping with your hand.
14. As you inhale, straighten your left leg and stretch your arm forward, above your head. As you exhale, pull your knee toward your chest, helping with your hand.
Lying on your left side
15. Repeat exercises 13 and 14, changing the supporting hand.
Lying on your stomach
16. Hands under shoulders. Without lifting your hands from the floor, first get on all fours and then roll onto your feet. Return to starting position.
17. Perform alternating leg swings: while inhaling, lift the leg, while exhaling, lower it.
18. As you inhale, push your stomach out, and as you exhale, pull it in.