Adrenergic stimulants (adrenergic agonists) are medications that stimulate different types of adrenergic receptors in organs and tissues, thereby imitating the effects of natural biologically active substances - the mediator norepinephrine and the adrenal hormone adrenaline.
Norepinephrine is a transmitter of impulses in the peripheral nervous system, regulating the functioning of many internal organs and systems (in particular, the heart, blood vessels, bronchi, uterus, pancreas, urinary system, etc.). Adrenaline is similar in structure and function to norepinephrine and is a hormone of the inner (brain) layer of the adrenal cortex.
Norepinephrine and adrenaline realize their effects through interaction with special structural components of cells - receptors, namely adrenergic receptors. Depending on their location and functions, adrenergic receptors are classified into alpha (α)- and beta (β)-adrenergic receptors.
α-Adrenergic receptors are located mainly in blood vessels, the iris of the eye, and the urinary tract. The effects of α-adrenergic receptor stimulation include constriction of blood vessels (and consequently increased blood pressure), pupil dilation, and urinary retention.
β-Adrenergic receptors are localized primarily in the heart (β1-adrenergic receptors), as well as in the bronchi and uterus (β2-adrenergic receptors). When they are stimulated, an increase in the strength and frequency of heart contractions, dilation of the bronchi and relaxation of the uterus are observed.
There is a separate class of drugs that can stimulate adrenergic receptors (adrenergic agonists, adrenergic stimulants), and a group of drugs that can block adrenergic receptors (adrenergic blockers, adrenergic steroids).
Depending on the degree of selectivity, adrenergic stimulants are divided into α-adrenergic agonists, β-adrenergic agonists, as well as α- and β-adrenergic agonists. Let us consider in detail drugs that stimulate β-adrenergic receptors.
Indications for use
β1-adrenergic agonists are used for acute heart failure associated with low cardiac output - against the background of myocardial infarction, cardiomyopathies, cardiogenic shock, and during heart surgery.
β2-adrenergic agonists are used for diseases associated with bronchospasm - bronchial asthma, chronic obstructive pulmonary disease.
Also, β2-adrenergic agonists are prescribed when there is a threat of premature birth.
β3-adrenergic agonists are used for diseases associated with increased bladder tone - overactive bladder syndrome: urinary incontinence, frequent urination.
pharmachologic effect
β1-Adrenergic agonists stimulate β1-adrenergic receptors in the myocardium, which leads to an increase in the strength and frequency of heart contractions (and, as a consequence, cardiac output and blood pressure).
β2-Adrenergic agonists stimulate β2-adrenergic receptors in the bronchi, providing a bronchodilator (bronchodilator) effect, and also, due to stimulation of β2-adrenergic receptors of the uterus, have a tocolytic effect (relax the muscles of the uterus).
β3-Adrenergic agonists stimulate β3-adrenergic receptors in the bladder, relaxing its muscles and preventing urinary incontinence.
New possibilities for drug treatment of overactive bladder
The issues of drug therapy for overactive bladder, a severe urination disorder that affects at least 17% of the population over 40 years of age, are considered. Traditionally, the treatment of overactive bladder has used drugs that target muscarinic receptors in the bladder. However, the pronounced side effects of this class of drugs and low patient adherence to therapy have necessitated the development of new drugs. The article provides data in favor of prescribing the first registered drug of an alternative pharmacological group recommended for the treatment of overactive bladder, the beta-3-adrenergic agonist mirabegron (Betmiga).
Table 1. Selectivity of action of M-anticholinergic agents in relation to the bladder
Table 2. Affinity of mirabegron for human adrenergic receptors [27]
Introduction
Overactive bladder (OAB) is a severe urinary disorder that affects at least 17% of the population over 40 years of age, of which 56% are women and 44% are men [1].
With age, the frequency of symptoms increases to 30 and 40% in people over 65 and 70 years of age, respectively. OAB occurs in 52–80% of men with bladder outlet obstruction due to prostatic hyperplasia, and 38–47% of men continue to suffer from OAB even after surgical removal of the obstruction [2, 3].
The prevalence of urinary frequency and urgency is almost the same among men and women, and urgency urinary incontinence is more common in women of older age groups. 70% of women associate their appearance with the onset of menopause, which is considered as one of the main risk factors for the development of OAB in women [4].
Etiology and pathogenesis
The etiology and pathogenesis of imperative urinary disorders caused by OAB are still unclear.
Nerve degeneration is a common feature of the development of an overactive bladder. It is possible that detrusor overactivity is caused by age-related changes not only in the urinary tract, but also in the central nervous system.
Disturbances in the parasympathetic and sympathetic innervation of the bladder are considered important in the pathogenesis of OAB. The sympathetic system is represented by alpha and beta adrenergic receptors. Alpha adrenergic receptors are mainly located in the neck of the bladder, the prostatic urethra, the prostate gland, as well as in the walls of blood vessels and, to a lesser extent, in the body of the bladder itself. Beta-adrenergic receptors are sensitive to norepinephrine and epinephrine, the main neurotransmitters of the sympathetic autonomic nervous system. In the bladder, the filling phase of the voiding cycle is regulated primarily by the sympathetic nervous system. In contrast, bladder emptying is stimulated by the release of acetylcholine in the parasympathetic nerve endings [5].
The human bladder contains beta-adrenergic receptors of the first, second and third types. Beta-3 adrenergic receptors make up at least 95% of all receptors in the bladder and are considered responsible for detrusor relaxation [6, 7]. Beta-3 adrenergic receptors are specific to the bladder and can be identified in the urothelium, interstitial cells of the detrusor and directly in the smooth muscle fibers of the bladder. Norepinephrine binds to beta-3 adrenergic receptors in the detrusor muscles, promoting relaxation [8].
Parasympathetic stimulation is mediated by the binding of acetylcholine to muscarinic receptors, which leads to detrusor contraction. Currently, five molecular subtypes of muscarinic M-cholinergic receptors are known (Table 1). The majority of muscarinic receptors in the bladder are of the M2 subtype (80%) [9]. The smooth muscle of the human bladder contains mixed populations of M2 and M3 subtypes.
Particular attention is paid to the M3-cholinergic receptors, through which the impulse to contract the detrusor is transmitted, and the M2-cholinergic receptors, the effect on which prevents the relaxation of the smooth muscles of the detrusor.
Stimulation of M3 receptors by acetylcholine leads to phosphoinositol hydrolysis and ultimately to the accumulation of intracellular calcium and smooth muscle contraction. Activation of M2 receptors leads to inhibition of adenylate cyclase and restores sympathetic-associated relaxation of bladder smooth muscle. This ensures the most complete emptying of the bladder.
Some current evidence suggests that M2 muscarinic receptors may play an important role in the age-dependent increase in alpha-1 adrenergic receptor response in bladder tissue, and facilitation of the contractile response associated with alpha-1A adrenergic receptors may be a cause of bladder overactivity in the elderly. of people.
With detrusor hypertrophy resulting from bladder outlet obstruction, metabolic demands increase and blood flow decreases, leading to anoxia and neuronal death. Moreover, there is evidence that the density of cholinergic nerve fibers in the detrusor is 60% less in patients with benign prostatic hyperplasia and bladder outlet obstruction compared with age-matched men without bladder outlet obstruction [10]. A significant decrease in nerve fiber density in response to bladder outlet obstruction due to benign prostatic hyperplasia can lead to impaired neuromuscular control of the bladder.
Physiological aging of the male or female body is associated with a deterioration in blood supply. This suggests that hypoxia may underlie intramural neuronal damage and lead to altered bladder smooth muscle function in patients with detrusor overactivity. The consequence of ischemia is apoptosis of smooth muscle cells, as well as disruption of nerve conduction. Nerve tissue is more sensitive to ischemia than smooth muscle, and some of this damage is almost irreversible. P. Abrams (1985) believes that detrusor overactivity in patients with benign prostatic hyperplasia is caused not by bladder outlet obstruction, but by age-related changes in the bladder wall.
Although data are inconsistent, it is recognized that both age and bladder outlet obstruction can lead to postsynaptic denervation of the bladder. This circumstance once again emphasizes the important role of the nervous system in controlling the storage function of the bladder.
In the development of OAB in menopausal women, the role of estrogen deficiency, associated atrophic changes in the urothelium, and dystrophic changes in the detrusor are actively discussed [11, 12]. Perhaps this is the reason for the sensory symptoms accompanying “dry” OAB (pollakiuria, nocturia, urinary urgency). Some studies have shown that individual neurons in the spinal cord contain estrogen receptors and are targets for estrogen. The presence of estrogen receptors in central brain neurons raises the possibility that endocrine age-related changes may act through supraspinal voiding control.
The role of hereditary factors is being studied, and a number of modern studies indicate the possibility of genetic changes in the presence of OAB [13].
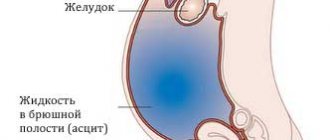
Clinically, detrusor overactivity is manifested by an urgent (urgent, imperative) urge to urinate, pollakiuria, nocturia and the so-called urinary incontinence upon urge (or urgent urinary incontinence). Occurring at any time and often in an inconvenient place, these symptoms bring significant anxiety to patients. Urgent urinary incontinence is not a prerequisite for diagnosing OAB, since approximately half of patients have symptoms: frequent daytime and nighttime urination, urgency. This variant of the symptom complex is called “dry” overactive bladder. In the case of urge urinary incontinence, it is customary to speak of a “wet” or “wet” overactive bladder [14, 15].
One of the latest definitions of OAB, approved by the International Continence Society, differs from the above [14]: overactive bladder is a symptom complex characterized by urgency with or without urgent urinary incontinence, and the presence of frequent urination.
Pharmacotherapy
According to generally accepted recommendations, the treatment of choice for OAB is pharmacotherapy, followed by behavioral therapy, physical therapy, and other types of treatment.
The advantages of pharmacotherapy are that it is accessible, gives a quick effect, and saves the doctor’s time. For patients, drug therapy is attractive because it does not require significant effort from them. In addition, drug therapy can be carried out long-term and personalized (individual selection of dose and regimen).
Pathogenetic pharmacotherapy should be focused on possible myogenic and neurogenic mechanisms of OAB development. Its goal is to eliminate the leading symptoms, which is directly related to the improvement of urodynamic parameters: a decrease in detrusor activity, an increase in the functional capacity of the bladder. The targets of pharmacotherapy can be divided into central and peripheral. The central ones include the areas of urinary control in the spinal cord and brain, and the peripheral ones include the bladder, urethra, prostate gland, peripheral nerves and ganglia.
Drugs for the pharmacological correction of OAB must meet the following requirements: be selective for bladder receptors, be well tolerated to allow long-term therapy, and effectively address the main symptoms of OAB, including urinary incontinence. An ideal drug for the treatment of OAB, providing an optimal balance between effective symptom relief and minimal adverse events, allowing for adherence to treatment and prolongation of therapy. Unfortunately, the number of patients receiving adequate OAB therapy in Russia is 17 times less than in the UK, and 15 times less than in Germany.
M-anticholinergics
Currently, the most commonly used drugs in the treatment of OAB are those that act on muscarinic receptors in the bladder. It has been proven that acetylcholine-mediated stimulation of detrusor M receptors plays a leading role in both normal and “unstable” detrusor contractions [16]. Most drugs are associated with inevitable adverse events, requiring the clinician to balance the benefits and drawbacks of treatment. The antimuscarinic effect is usually accompanied by dry mouth, constipation, accommodation difficulties, and drowsiness. The drugs should not be prescribed to patients with impaired urine flow from the bladder (obstructive uropathy), bowel obstruction, ulcerative colitis, glaucoma or myasthenia gravis.
Currently, the following M-anticholinergic blockers are used in Russia: solifenacin (Vesicare), oxybutynin (Driptan), trospium chloride (Spazmex), tolterodine (Detrusitol, Urotol). Solifenacin is the most selective for the subtypes of M3 cholinergic receptors of the bladder detrusor (Table 1) [17].
The good tolerability of solifenacin (Vesicar) in patients of the older age group determines the choice of this drug in the treatment of urgent urinary disorders. Patients in this age group, as a rule, have concomitant diseases and are forced to take several medications, which significantly increases the risk of developing side effects.
To date, the effectiveness of solifenacin has been confirmed (with the possibility of increasing the dosage) in the treatment of the main symptoms of OAB and the need to use 10 mg of the drug at the start of therapy has been updated. Thus, Vesicare 10 mg effectively eliminates all symptoms of OAB [18]. Vesicare 5/10 mg reduces urgency by 89%, while solifenacin is more effective than tolterodine in reducing urgency and urge urinary incontinence [19]. Increasing the dose of Vesicare to 10 mg allows achieving better results in the treatment of patients with OAB [20]. The effectiveness of Vesicare 10 mg is accompanied by a favorable safety and tolerability profile [20]. Vesicare 10 mg does not have a significant effect on cognitive function in elderly patients, unlike oxybutynin [21]. Vesicare 10 mg, due to its optimal balance of efficacy and safety, is characterized by the highest compliance among the available M-anticholinergics [22].
However, it is necessary to note some realities of life that are the reasons for stopping antimuscarinic therapy for OAB: 46% of patients do not have the expected effect, 25% switched to a new drug, 23% learned to do without medications, 21% of patients are forced to stop taking M-anticholinergics due to intolerable side effects [23].
Due to severe adverse events and insufficient patient adherence to treatment, attempts have been made to develop new drugs.
Beta-3 adrenergic agonist
The mirabegron molecule was developed by Japanese scientists and initially had the code name YM178 [24]. In 2011, the drug was introduced into the local pharmaceutical market in Japan. In 2012, Mirabegron was approved for use in the United States under the name Mirbetric. In 2013, the drug became available in Europe, but under a different name - Betmiga. Mirabegron is produced in the form of an Oral Controlled Absorption System. The drug is available in tablet form in dosages of 50 and 25 mg. The last dosage is intended for patients with liver or kidney failure.
Mirabegron is highly selective for beta-3 adrenergic receptors: its affinity for beta 3 adrenergic receptors is 105 and 33 times higher than for beta 1 and beta 2 adrenergic receptors, respectively (Table 2) [25]. Activation of beta-3 adrenergic receptors by mirabegron stimulates detrusor relaxation and promotes urinary continence, leading to an increase in bladder storage capacity and voiding interval [26, 27]. Mirabegron does not affect the parasympathetic stimulation of detrusor contraction and bladder emptying and therefore, unlike antimuscarinics, may reduce the risk of acute urinary retention [26–28].
The concept of treating OAB with mirabegron was confirmed in the BLOSSOM study, which was published by S. Chapple et al. in 2008 [29]. Clinical centers from six European countries participated in this study. Patients with OAB (n = 260) were randomly assigned to four groups and received placebo, mirabegron 100 mg twice daily, mirabegron 150 mg twice daily, or tolterodine sustained release 4 mg once daily for four weeks. Significant benefits were found for both doses of mirabegron compared to placebo and tolterodine in the treatment of pollakiuria, as well as a clear advantage of mirabegron compared to placebo in the treatment of urgency, urinary incontinence and nocturia. The incidence of adverse reactions was 39.2% for mirabegron, 36.4% for placebo, and 48.4% for tolterodine.
Under the leadership of S. Chapple, the European DRAGON study was initiated to find the optimal dose of mirabegron, which included 919 patients [30]. Patients were assigned to five groups: placebo, mirabegron 25, 50, 100 and 200 mg. Treatment was carried out over 12 weeks. Doses of 50, 100 and 200 mg showed little difference in effectiveness. It was on the basis of this study that the standard dose of the drug was determined at 50 mg. The incidence of adverse reactions for mirabegron in this study was not higher than that for tolterodine, and the incidence of dry mouth was significantly lower compared to anticholinergics.
Another large study examining mirabegron was the North American and Canadian ARIES study [31]. A double-blind comparative analysis of the effectiveness of mirabegron 50 and 100 mg and placebo was conducted. 1328 patients with OAB were divided into three appropriate groups. After 12 weeks, the mirabegron groups compared with the placebo group showed a reduction in episodes of urinary incontinence (-1.13, -1.47 and -1.63 for placebo, 50 and 100 mg mirabegron, respectively) and urinary frequency (-1. 05, -1.66 and -1.75, p
The European-American randomized, double-blind, placebo-controlled trial CAPRICORN included 1306 patients. They were randomized to receive placebo and mirabegron 25 or 50 mg for 12 weeks [32]. Mirabegron 50 mg was eventually adopted as the primary formulation for the treatment of OAB. Mirabegron was more effective than placebo in women and men with OAB, but the effect was less pronounced in men, especially those with prostate hyperplasia.
In the SCORPIO study, V. Khullar compared the effectiveness of mirabegron and sustained-release tolterodine [33]. This one of the largest studies included 1978 patients with OAB from Europe and Australia. The duration of treatment was 12 weeks, patients were divided into four groups: placebo (n = 494), mirabegron 50 mg (n = 493), mirabegron 100 mg (n = 496), tolterodine sustained release 4 mg (n = 495). Despite the significant improvement in the patients' condition in all symptoms of OAB, the benefits of mirabegron did not reach statistical significance compared to tolterodine. Mirabegron turned out to be very effective in patients who had previously received anticholinergics and stopped taking them due to insufficient effect or severe adverse reactions. While taking the drug, there were no cases of urinary retention; significantly fewer episodes of dry mouth, constipation and other adverse events from the gastrointestinal tract were recorded.
Of interest are the results of the multicenter TAURUS study, which included 2444 patients from North America, Europe and other countries [34]. Patients were assigned to four groups: placebo, mirabegron 50 mg, mirabegron 100 mg, and tolterodine sustained release 4 mg. Drugs and placebo were continued for 12 months. It is the long treatment period that determines the value of the data obtained. Patients were examined one, three and 12 months after the start of treatment. Over the course of a year of therapy, there was a persistent decrease in the number of episodes of urinary and urinary incontinence while taking mirabegron. Both mirabegron and anticholinergics caused adverse events such as hypertension, constipation, and headache with equal frequency. Dry mouth was much more common in patients receiving anticholinergics. There was no prolongation of the QT interval on the electrocardiogram with long-term use of mirabegron.
Mirabegron is not contraindicated in patients with glaucoma and is comparable to placebo in its effect on intraocular pressure [28, 33, 34]. The incidence of central nervous system side effects in clinical trials is also comparable to placebo, and the drug does not affect cognitive function. Thus, the drug can be safely prescribed to elderly patients.
To date, Mirabegron is the first registered drug of an alternative pharmacological group, which has undergone numerous clinical studies and has proven highly effective in eliminating urinary urgency and urinary incontinence associated with urgency.
Basics of treatment with β-adrenergic agonists
β-Adrenergic stimulants are classified as prescription drugs - drugs are dispensed from pharmacies only with a doctor's prescription.
The β1-adrenergic agonist dobutamine is administered intravenously in a hospital setting under the constant supervision of a physician. The effect of the drug develops after 1-2 minutes, the maximum effect is observed after 10 minutes.
For the treatment of bronchial asthma and chronic obstructive pulmonary disease, β2-adrenergic agonists are used by inhalation.
To prevent premature birth, β2-agonists are used as intravenous injections, infusions, or taken orally (orally) as tablets.
Mirabegron is used orally in tablet form once a day.
Features of treatment with β-adrenergic agonists
Salbutamol and fenoterol have a rapid (the effect develops within 1-3 minutes) but short-lived (3-6 hours) effect, so they are used to relieve (eliminate) attacks of bronchial asthma.
Salmeterol and formoterol have a long-lasting effect - more than 12 hours; in addition, the effect of these drugs does not develop immediately, but only 30 minutes after use. That is why salmeterol and formoterol are used to prevent the development of bronchospasms.
In the long-term treatment of bronchial asthma and chronic obstructive pulmonary disease, combination drugs are used, which include both β2-adrenergic agonists and M-cholinergic blockers (ipratropium bromide, tiotropium bromide, umeclidinium bromide, aclidinium bromide, glycopyrronium bromide), as well as hormonal drugs of the class glucocorticosteroids (fluticasone, budesonide).
PsyAndNeuro.ru
The material was prepared jointly by the educational project “Psychiatry & Neuroscience” and the Clinic of Psychiatry and Narcology Doctor SAN.
We present to your attention comprehensive practical recommendations for psychopharmacotherapy for diseases of the respiratory system. The recommendations describe psychiatric symptoms often encountered in diseases of the respiratory system, their differential diagnosis, neuropsychiatric side effects of drugs for the treatment of diseases of the respiratory system, drug interactions, as well as the effectiveness and safety of psychotropic drugs in diseases of the respiratory system.
Asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis, tuberculosis, obstructive sleep apnea, vocal cord dysfunction, pulmonary embolism - all of these diseases may have symptoms that require psychopharmacological treatment. Most of these diseases (except for cystic fibrosis, or if the patient smokes) do not affect the metabolism of pulmonary or other drugs. The main thing is to avoid taking medications that suppress the activity of the respiratory center or otherwise negatively affect ventilation of the lungs.
Asthma:
Anxiety, depression, substance abuse (marijuana, crack cocaine), sleep disorders
COPD:
Anxiety, depression, nicotine addiction, cognitive decline, sleep disorders, sexual dysfunction, fatigue
Cystic fibrosis:
Depression, anxiety, eating disorders
Vocal cord dysfunction:
Anxiety, depression, conversion disorder
Hyperventilation syndrome:
Anxiety, depression, pseudoconvulsions
Sleep apnea:
Drowsiness, sleep disturbances, irritability, depression, cognitive decline
Tuberculosis:
Psychosis, sleep disturbances, substance abuse, cognitive impairment, fatigue, lethargy, mania, delirium
In all of these diseases, psychiatric symptoms often occur, requiring the prescription of psychotropic drugs. Diagnosis can be difficult because symptoms of respiratory diseases overlap with symptoms of mental disorders. In addition, a cyclical sequence of psychiatric and respiratory symptoms is common, making it difficult to determine the underlying cause of the condition in the presence of associated factors.
Anxiety
Shortness of breath, chest tightness and a feeling of suffocation are common in anxiety disorders and respiratory diseases. Somatic manifestations of anxiety may be caused by a comorbid anxiety disorder, anxiety in response to a respiratory disorder, or the respiratory disorder itself.
It is important, if possible, to carry out differentiated diagnostics; if the symptoms have a physiological basis (for example, hypoxia), then they need to be addressed regardless of the treatment of anxiety or in conjunction with this treatment. For example, with pulmonary embolism, shortness of breath and hyperventilation may occur in the absence of chest pain, which may be mistaken for a panic attack.
Anxiety disorders, especially panic disorder, must be considered in the differential diagnosis of vocal cord dysfunction. Anxiety disorders occur in nearly one in three patients with asthma presenting to primary care; Anxiety can trigger asthma attacks. Theophylline and many beta-agonists may cause or worsen anxiety. Anxiety often accompanies vocal cord dysfunction and pulmonary embolism. Anxiety disorders, especially panic disorder with agoraphobia, occur with increased frequency in patients with COPD.
Depression
Patients with asthma, COPD and cystic fibrosis are more likely to experience depressive symptoms than the general population. Diagnosing depression can be difficult in patients with chronic respiratory diseases because many symptoms overlap, such as fatigue, poor sleep, decreased ability to perform activities, weight loss, and anorexia. Tuberculosis may cause diagnostically confusing signs of depression, such as weight loss, lethargy, sleep disturbances, loss of interest in daily activities, and confusion.
Sleep disorders
Sleep disturbances can be caused by apnea, nocturnal cough, nocturnal asthma attacks, medication side effects, and comorbid anxiety or depression. More than 50% of COPD patients complain of sleep disturbances. Many patients with COPD have obstructive sleep apnea, leading to daytime sleepiness, insomnia, and very often irritability and depressive symptoms. These patients may experience significant difficulties with concentration, attention, and memory.
Cognitive deficit
Cognitive dysfunction is common in patients with COPD, even in those who do not have chronic hypoxia or hypercapnia. Patients with severe COPD may develop irreversible cognitive deficits and subclinical encephalopathy due to repeated episodes of hypoxia or chronic hypoxia. Oxygen therapy helps minimize cognitive deficits in patients with mild hypoxia. Cognitive deficits may have potentially reversible causes, such as hypercapnia or exacerbation of underlying cardiac disease.
Drugs used in the treatment of diseases of the respiratory system often cause neuropsychiatric side effects.
Anticholinergics
Atropine: Paranoia; tactile, visual and auditory hallucinations; memory loss; delirium; agitation
Beta-agonists
Salbutamol, levosalbutamol: Anxiety, insomnia, paranoia, hallucinations, tremors, rapid heartbeat
Formoterol, arformoterol: Insomnia, anxiety, tremor, rapid heartbeat
Isoproterenol: Anxiety, insomnia, tremor
Metaproterenol: Anxiety, insomnia
Pirbuterol: Anxiety, tremors
Salmeterol: Anxiety, tremors, rapid heartbeat
Bronchodilators
Aminophylline, theophylline: Anxiety, insomnia, tremor, restlessness, withdrawal syndrome, hyperactivity, psychosis, delirium, mutism
Oral corticosteroids
Prednisone, prednisolone, dexamethasone: Depression, mania, emotional instability, anxiety, insomnia, psychosis, hallucinations, paranoia, personality changes
Leukotriene inhibitors
Montelukast: Fatigue, asthenia, suicidal ideation
Adrenergic agonists of mixed action
Adrenaline: Anxiety, tremors, psychosis
Phenylephrine: Depression, hallucinations, paranoia
Phenylpropanolamine: Restlessness, anxiety, insomnia, psychosis, hallucinations, aggressiveness
Other drugs
Acetazolamide: confusion, feeling unwell
Modafinil: Nervousness, depression, anxiety
Corticosteroids
Inhaled corticosteroids rarely produce side effects, but oral corticosteroids (eg, prednisone, prednisolone, dexamethasone) may cause depression, mania, emotional lability, anxiety, insomnia, psychosis, hallucinations, paranoia, and personality changes.
Bronchodilators
The most common side effects of beta-adrenergic bronchodilators include nervousness and tremor. Albuterol may cause insomnia. Over-the-counter inhalers containing epinephrine or ephedrine can cause anxiety and, if taken in large doses, psychosis.
Adrenergic agonists of mixed action
Mixed-action adrenergic agonists are often used for asthma. Epinephrine, ephedrine, phenylephrine and phenylpropanolamine can cause anxiety, insomnia, tremor and psychosis.
Theophylline
Theophylline can cause increased neuro-reflex excitability, insomnia, anxiety, restlessness and irritability, which can be mistaken for a primary anxiety disorder or akathisia. Symptoms caused by theophylline are usually dose dependent and develop soon after taking the drug. Treatment involves reducing the dose to the lowest effective dose, changing the timing of administration, and/or switching to other asthma medications. A patient with anxiety may be able to avoid oral theophylline by using inhaled cromoglycic acid, ipratropium bromide, or steroids.
The toxic effects of theophylline include severe anxiety, severe nausea, headache, insomnia, and can cause delirium with severe agitation and psychosis. Theophylline should be discontinued until symptoms subside and blood test values return to the therapeutic range. Theophylline can cause and worsen tremors. If theophylline cannot be stopped, beta blockers or benzodiazepines can be used against tremor. Although beta blockers have relative contraindications in COPD and asthma due to their bronchoconstrictor effect, beta blockers with high cardioselectivity such as acebutolol, atenolol, celiprolol, metoprolol and practolol can be prescribed to patients with mild to moderate reactive airway disease, and also for patients with COPD.
Antibiotics and anti-tuberculosis drugs
Antibiotics used to treat infections associated with asthma or COPD usually produce minimal side effects. At the same time, taking anti-TB drugs is associated with more frequent and severe side effects, including depression, anorexia, anxiety, insomnia, delusions, hallucinations and toxic psychosis.
Anticholinergic drugs
Atropine, an anticholinergic drug that is rarely used to treat asthma, can cause paranoia, tactile, visual and auditory hallucinations, memory loss, delirium and agitation. Inhaled ipratropium bromide and tiotropium bromide are anticholinergic drugs that do not cause significant psychiatric side effects.
Leukotriene inhibitors
Montelukast may cause dizziness, fatigue, asthenia, and suicidal ideation, although it is not associated with an increase in suicide attempts. Another leukotriene inhibitor, zafirlukast, does not appear to cause significant psychiatric side effects.
Drugs for the treatment of obstructive sleep apnea
Taking acetazolamide may cause confusion and feelings of illness. Modafinil, approved in the US as a treatment for daytime sleepiness, can cause nervousness, depression and anxiety.
For the most part, respiratory diseases do not affect pharmacokinetics, but there are two important exceptions: cystic fibrosis and smoking. Cystic fibrosis may alter pharmacokinetics due to impaired transport function of the cell membrane. The rate of absorption of the drug slows down, but the degree of absorption usually does not change, and the bioavailability remains the same. This does not affect the volume of distribution in any way. Cystic fibrosis increases oxidative hepatic metabolism, but only for the drug substrates cytochrome P450 (CYP) 1A2 and 2C8; metabolism by other cytochromes remains unchanged. There are few scientific studies on the use of lithium in patients with cystic fibrosis and the available data are contradictory. There are reports that renal clearance is reduced, resulting in higher lithium levels. At the same time, a clinical case was described in which the lithium level did not change. It is prudent to begin treatment with lithium in patients with cystic fibrosis at low doses and monitor their condition closely.
Smoking, in addition to causing diseases of the respiratory system, affects the pharmacodynamics and pharmacokinetics of many drugs. Smoking causes bronchoconstriction, which interferes with treatment and weakens the effect of taking bronchodilators. Smoking induces CYP1A2, which increases the metabolism of substrates of this hepatic enzyme, including clozapine, olanzapine, duloxetine and theophylline.
Psychotropic drugs for diseases of the respiratory system
Antidepressants
Antidepressants are often used to treat anxiety and depression in patients with chronic respiratory diseases. Most published studies have focused on the use of these drugs in patients with asthma and COPD; There is virtually no information on the use of antidepressants in patients with cystic fibrosis or tuberculosis, and little data has been collected on the use of antidepressants in patients with obstructive sleep apnea.
When treating patients with severe forms of COPD or obstructive sleep apnea, special care must be taken when combining sedating antidepressants with other sedatives, such as anxiolytics and hypnotics; sedative effects can lead to a weakening of the activity of the respiratory center. Very few studies have been conducted to evaluate the safety and effectiveness of antidepressants in patients with pulmonary disease, and therefore their safety can only be inferred from the lack of published reports of dangerous reactions.
It was previously thought that anticholinergic drugs were contraindicated in bronchospastic conditions, but tiotropium bromide is now often used? inhaled anticholinergic agent. Thus, although data are still limited, it can be assumed that the anticholinergic effect of a tricyclic antidepressant may reduce bronchoconstriction. It can also be expected that the drying effect of anticholinergic TCAs will be beneficial for asthma patients with heavy fluid secretions, but will worsen the condition in patients whose airways are clogged with thickened mucus. TCAs should not be prescribed to patients with cystic fibrosis because the anticholinergic drying effect will increase difficulty clearing mucus.
Apart from drug interaction issues, the use of antidepressants in patients with tuberculosis is safe. There are no studies examining the use of monoamine oxidase inhibitors in the setting of respiratory disease, but these drugs are known to be associated with serious drug interaction problems.
Benzodiazepines
The inhibitory effect of benzodiazepines on respiratory activity can significantly impair the response of pulmonary ventilation. This may lead to the development of respiratory failure in patients with limited respiratory reserve, so benzodiazepines are contraindicated in hypercapnia. Patients with severe bronchitis, severe restrictive pulmonary disease, or sleep apnea are most susceptible to the adverse effects of benzodiazepines.
At the same time, benzodiazepines are not contraindicated in COPD and asthma. Worsening anxiety often has a negative impact on the respiratory system, and in such cases, benzodiazepines improve the condition of patients with asthma or emphysema. In contrast, in patients with obstructive sleep apnea, benzodiazepines suppress respiratory activity, which can increase the duration of apnea episodes and lead to dangerous consequences.
Benzodiazepines help with severe episodes of vocal cord dysfunction. When prescribing benzodiazepines, it is best to use reduced doses of shorter-acting drugs (for example, lorazepam) so that side effects are mild and disappear quickly after stopping use.
Other anxiolytics and hypnotics
Some nonbenzodiazepine drugs are useful for improving sleep in patients with respiratory diseases. Zolpidem helps patients with severe obstructive sleep apnea fall asleep without compromising the effectiveness of CPAP therapy. In addition, it does not worsen respiratory performance and pulmonary function tests in patients with COPD. In patients with mild to moderate sleep apnea, zopiclone improves sleep without impairing breathing. The effectiveness of trazodone in this group of patients has not been studied.
The drug of choice in patients with respiratory diseases suffering from chronic anxiety should be buspirone due to the fact that it does not have a depressant effect on breathing. Buspirone may improve respiratory status in patients with sleep apnea, exercise capacity, and shortness of breath in patients with chronic lung disease. There is evidence that buspirone is effective and well tolerated in combination with bronchodilators.
The use of barbiturates should be avoided in patients with respiratory impairment, severe COPD, or obstructive sleep apnea who are experiencing alcohol withdrawal. An exception may be long-term treatment of epilepsy with phenobarbital.
Antipsychotics
Although studies are small, clinical experience suggests that atypical and typical antipsychotics can be used in patients with respiratory disorders, with certain precautions regarding how extrapyramidal symptoms, weight gain, and tardive dyskinesia affect respiratory function and risk of aspiration pneumonia in elderly patients with dementia.
Laryngeal dystonia, manifested as acute shortness of breath, is an extremely rare form of acute dystonic reaction. It is usually associated with high-potency typical antipsychotics, but there are case reports with ziprasidone. Typically, this, like other dystonic reactions, occurs within 24-48 hours of starting antipsychotic therapy or, in rare cases, after increasing the dose. Laryngeal dystonia can be life-threatening, but usually resolves completely with intramuscular injection of anticholinergic drugs. Tardive dyskinesia affecting the respiratory muscles is a rare phenomenon that usually occurs with long-term use of typical antipsychotics and can lead to significant deterioration in breathing in patients with reduced tidal volume.
Weight gain while taking olanzapine, quetiapine, and other atypical antipsychotics is particularly problematic in patients with obstructive sleep apnea; additional weight worsens apnea. In addition, increased body weight may lead to decreased tidal volume in patients with impaired respiratory function, especially those with restrictive pulmonary disease. There is evidence that olanzapine and possibly risperidone may be associated with an increased risk of pulmonary embolism.
Patients taking atypical antipsychotics have a significantly increased risk of death from asthma. The risk is especially high in patients who have recently stopped taking antipsychotic medications. Patients with asthma and COPD are at increased risk of arrhythmia. If an antipsychotic must be prescribed, it is best to avoid the use of those drugs most likely to cause QT prolongation (ziprasidone, thioridazine), or, otherwise, carefully monitor the patient's condition. Abruptly stopping antipsychotics with significant anticholinergic effects, such as clozapine, may cause cholinergic rebound syndrome, which reduces the effectiveness of anticholinergic drugs for treating asthma. These medications should be discontinued slowly to prevent cholinergic rebound syndrome.
The use of antipsychotics in the treatment of older patients with dementia is associated with an increased risk of death from cardiovascular complications and infection, particularly pneumonia. Pneumonia in such cases may be associated with aspiration of secretions resulting from sedation and dysphagia.
Mood stabilizers
Several case reports suggest that carbamazepine is associated with pulmonary eosinophilia, diffuse parenchymal lung disease, and respiratory failure. Carbamazepine has also been found to be an effective treatment for asthma.
Psychostimulants
Chronic diseases of the respiratory system often lead to insomnia and daytime sleepiness. There is little research on the use of stimulants in patients with sleep apnea. Modafinil (and also armodafinil, the R-enantiomer of modafinil) increases daytime wakefulness when used as an adjunctive treatment in patients with obstructive sleep apnea who improve with CPAP therapy but still experience daytime sleepiness. Concentration and functioning are improved while sleep architecture remains unaffected. Atomoxetine improves the quality of wakefulness in patients with mild to moderate obstructive sleep apnea without worsening the index of respiratory events. However, since this topic remains poorly researched, and also because of the increased risk of arrhythmia in chronic diseases of the respiratory system, the use of psychostimulants should be treated with caution.
Antidementia drugs
The use of cognitive enhancers in patients with respiratory diseases has been poorly studied. Cholinesterase inhibitors increase acetylcholine levels and may cause bronchoconstriction. In addition, they are likely to block the therapeutic effect of bronchodilators, especially anticholinergic agents such as ipratropium bromide and tiotropium bromide. The most common pulmonary side effects of these drugs are shortness of breath and bronchitis, while uncommon side effects include pneumonia, hyperventilation, pulmonary edema, wheezing, hypoxia, pleurisy, pulmonary collapse, sleep apnea, and snoring.
Thus, cholinesterase inhibitors should be prescribed with caution, or better not at all, in patients with asthma and COPD. An alternative is memantine, which does not produce respiratory side effects.
Opioids
When dyspnea in patients with advanced pulmonary disease cannot be controlled, a variety of pharmacological agents, including opioids, are used. COPD studies show that opioids have a beneficial effect on shortness of breath, and are better when administered orally or parenterally than when administered inhaled. Harmful effects on arterial blood gases and oxygen saturation have not been demonstrated. Low-dose oral or parenteral opioids are used to treat dyspnea in end-stage pulmonary disease.
Sedative-hypnotics and morphine are often prescribed to patients with end-stage pulmonary disease. Although these drugs have been shown to be effective, when prescribing them, the benefits of comfort must be weighed against the risk of potential shortening of life due to respiratory depression. Opioids (usually morphine) and sometimes benzodiazepines are used to remove ventilators in terminal conditions.
Some psychotropic drugs adversely affect lung function. The most common cause of respiratory depression is the use of sedatives, hypnotics and opioids. There are reports that methylphenidate causes shortness of breath, asthma, pulmonary infiltrate, idiopathic pulmonary fibrosis, respiratory failure and pulmonary vascular disease. Carbamazepine can cause cough, shortness of breath, pulmonary infiltration, and idiopathic pulmonary fibrosis. Benzodiazepines may cause coughing. A case of acute pulmonary edema following an overdose of phenothiazine has been described. Typical and atypical antipsychotics are associated with pulmonary embolism. In addition, high-potency antipsychotics such as haloperidol are associated with laryngeal dystonia and tardive dyskinesia of the respiratory muscles, causing respiratory distress. Overdose of trazodone can cause eosinophilic pneumonia and respiratory failure. TCAs have been associated with Loeffler's syndrome (eosinophilic pneumonia), and overdose can lead to pulmonary edema and subsequent respiratory distress syndrome. Isolated cases of eosinophilic pneumonia have been reported while taking other antidepressants, but this appears to be an extremely rare occurrence.
Drugs prescribed for chronic diseases of the respiratory system may enter into pharmacokinetic and pharmacodynamic interactions with psychotropic drugs.
It is important to note that smoking, which is a cause or one of the factors in the development of various diseases of the respiratory system, can enhance the metabolism of psychotropic substances by inducing CYP 1A2, 2B6 and 2D6. These substances include benzodiazepines, zolpidem, antipsychotics (aripiprazole, quetiapine, risperidone, and ziprasidone are important exceptions), and antidepressants, including fluvoxamine, duloxetine, TCAs, and mirtazapine. After reducing or stopping smoking, it may be necessary to reduce the dose of psychotropic drugs whose metabolism has been induced.
Many anti-infectives, including macrolides, fluoroquinolones and antifungals (miconazole, ketoconazole, fluconazole, voriconazole, itraconazole, posaconazole, etc.) are potent inhibitors of one or more of the CYP isoenzymes, and rifamycins, such as rifampicin, induce several CYP enzymes. Taking anti-infective drugs may cause psychotropic drug toxicity or lead to loss of therapeutic effect if the psychotropic drug is not adjusted accordingly.
Taking isoniazid, a weak MAOI, together with TCAs, SSRIs, SSRIs and MAOIs can be dangerous due to the risk of hypertensive crisis and serotonin syndrome. When isoniazid alone is taken, its action as an MAOI does not require changes in diet, but if it is combined with antidepressants, it is necessary to limit the consumption of products with tyramine. Patients taking isoniazid should not be prescribed sympathomimetics such as epinephrine, ephedrine, and pseudoephedrine, which are often included in over-the-counter cold, cough, and sinusitis medications, and oral beta-agonists should be used with extreme caution. Inhaled beta-agonists appear to be safer due to their lower systemic absorption. SSRIs and SSRIs are safely combined with selective beta2-agonists (terbutaline, metaproterenol, albuterol, isoetarine).
Theophylline may decrease the levels of alprazolam and possibly other benzodiazepines and reduce their therapeutic effect, causing anxiety and insomnia. Theophylline may increase the clearance of lithium; When taking these drugs concomitantly, lithium levels should be monitored.
Some psychotropic drugs, including TCAs, low-potency antipsychotics, and anticholinergic modifiers of extrapyramidal symptoms, produce anticholinergic effects that may enhance the bronchodilator effects of atropine and inhaled anticholinergic bronchodilators such as ipratropium bromide and tiotropium bromide.
Drugs for the treatment of diseases of the respiratory system may enter into pharmacokinetic interactions with psychotropic drugs. Fluvoxamine inhibits CYP1A2 and may significantly increase theophylline levels. Carbamazepine and phenobarbital significantly reduce the blood levels of many drugs, including theophylline and doxycycline. St. John's wort also induces CYP1A2 and may reduce theophylline levels to subtherapeutic levels.
The material was prepared jointly by the educational project “Psychiatry & Neuroscience” and the Clinic of Psychiatry and Narcology Doctor SAN.
Translation: Filippov D.S.
Editor: Kasyanov E.D.