Cardiomyopathy can come in various forms, among which left ventricular hypertrabecularity is considered the most rare. The disease is mainly identified in children, although it sometimes occurs among adults. In severe cases, even a heart transplant may be required.
Left ventricular hypertrabecularity (LVHT, non-compact myocardium, spongiform cardiomyopathy) is a condition in which the muscular wall of the left ventricle of the heart becomes “spongy”. This can affect the heart's ability to pump efficiently and the electrical conductivity of the myocardium.
Left ventricular (LV) hypertrabecularity cannot be completely cured, but medication can help patients reduce symptoms.
The disease occurs rarely and is considered a congenital pathology. During the embryological development of the heart, two layers are formed: normal and pathological (spongy). The development of the clinic and further examination of the patient makes it possible to make a diagnosis and prescribe symptomatic treatment.
Video: Noncompaction myocardium (NCM) - Non-compact (“spongy”) myocardium (NCM) or spongy cardiomyopathy
#2 2017-12-17 12:19:58
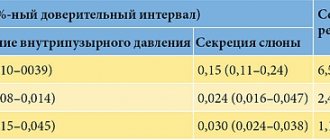
A trabecular bladder is formed due to a prolonged increase in intravesical pressure, as a result of impaired urine outflow from the bladder. High intravesical pressure deprives the detrusor muscles (the muscular lining of the bladder) of normal nutrition and oxygen supply. Some of the muscle bundles first hypertrophy (thicken from increased load) and then are replaced by scar. During cystoscopy they look like cords or trabeculae - constrictions. Between them, weaker areas protrude outward - pseudodiverticula. Such a bubble is called trabecular.
The degree of trabecularity varies. In some cases, the trabecular bladder may have a large volume.
Severe trabecularity of the bladder is a result of a chronic increase in intravesical pressure and does not develop back, since the scar cannot turn back into muscle. Therefore, it is very important to diagnose a violation of the outflow of urine from the bladder in time in order to prevent the development of a small-volume trabecular bladder - “cicatricial microcystis”.
After cervical plastic surgery or bladder closure, it is imperative (.) to maintain contact with the surgeon for timely correction of “obstruction”—difficulty in the passage of urine from the bladder.
Edited by Professor Nikolaev (2017-12-18 12:36:00)
Diagnostics
If left ventricular hypertrabecularity is suspected or symptoms that may indicate cardiac disease are present, various tests are performed. Most often, the diagnosis of LVHT includes the following:
- Analysis of the patient’s medical history and family tree - symptoms are determined and the presence of similar signs in other family members is determined.
- Physical examination is carried out to supplement the medical history with other signs characteristic of pathology.
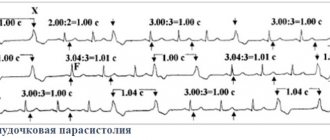
- ECG (electrocardiography) - the conduction of electrical impulses through the heart muscle is checked, and an ECG can also determine arrhythmias.
- Echo CG (echocardiography) with color Doppler is performed to assess the pumping function of the heart, the size of the walls of its chambers, including the left ventricle. With LVHT, the ratio of the compact to non-compact layer changes. In adults it is less than 2, and in children it is less than 1.4. Also, in one of the sections, several trabeculae and deep recesses are identified that communicate with the LV cavity.
- MRI (magnetic resonance imaging) - shows the structure of the heart. The movement of blood as it flows through the heart can also be determined. Such data can be used to detect trabeculation.
Criteria for diagnosing LVHT by MRI:
- Definition of two layers of cardiac muscle.
- Marked trabecularity evident on several diastolic sections.
- The ratio of the “spongy” layer to the normal one is 2.3 or more.
If misdiagnosed, LVHT may be mistaken for hypertrophic cardiomyopathy, fibroelastosis, and endomyocardial fibrosis. Also, instead of LVHT, a diagnosis of myocarditis, restrictive, dilated cardiomyopathy, etc. is often made.
Trabecular bladder
TRUE DIVERTICULUS
Along with the appearance of a trabecular bubble and the formation of false diverticula, in some cases limited, almost complete dissection of the vesical muscles and the formation of a true diverticulum may be observed. In such cases, the trabecularity of the bladder wall is weakly expressed or may be completely absent. At the same time, a round-shaped depression is usually formed outside the ureteral opening, which, gradually increasing, turns into a diverticulum, sometimes reaching a very significant size.
The entrance to a true diverticulum looks like an oval or round hole with a pouch of collected mucous, simulating the picture of a sphincter. The bottom and walls of a diverticulum that has reached a large size are usually not visible, as a result of which the entrance to the diverticulum appears as a black gaping hole in the wall of the bladder. Sometimes the diverticulum carries with it the orifice of the ureter, which is then located along the edge of the entrance to the diverticulum or on its inner wall at the very entrance. Preliminary clarification during cystoscopic examination of the relationship between the mouth of the ureter and the true diverticulum is of great importance during the operation of removing the diverticulum sac.
True diverticulum
CYSTOCELE
Bladder deformation is also caused by prolapse of the anterior vaginal wall, with which the bottom of the bladder is closely connected. With significant prolapse of the anterior vaginal wall, especially associated with simultaneous prolapse or prolapse of the uterus, the entire bladder is located under the pubic symphysis. In these cases, inserting the cystoscope into the bladder presents certain difficulties, since the beak of the cystoscope rests against the wall of the bladder. Filling the bladder does not change its topography, but only leads to the formation of a spherical protrusion that fills the vagina. In such cases, cystoscopy allows one to see only the cervical part of the bladder and the longitudinal, downward folding of the posterior wall of the bladder. To view the orifices of the ureters, a gauze or cotton swab should be inserted into the vagina. The mucous membrane, which previously had longitudinal folds, gathers into transverse folds. The bottom of the bladder has the appearance of a hill protruding into the bladder; at the top of the hill one can discern a funnel-shaped depression, at the bottom of which the mouth of the ureter is located.
Bladder trabecularity - what is it?
A man should remain a man at any age. To do this, you must always remember the main secret of his strength - health. But is he paying enough attention to this? Experience shows that this is not always the case. In this regard, we appeal to women. Dear ladies! Don't you want your men to be healthy? Why you? Yes, because most men begin to collect information about their diseases and methods of treating them when they are already sick. It is well known that prevention of any disease is cheaper than its treatment, both financially and morally. Women understand this better than men.
The author of the book, the famous urologist Lev Kruglyak, will help you understand the causes of male diseases, such as prostatitis, adenoma and prostate cancer, infertility and some others. You will learn how to prevent them, and also, if the disease has already made itself felt, how to cure it in time. The author’s main task is to help men maintain their health in order to create conditions for a full and fulfilling life into old age.
The book presents extensive material on alternative treatment methods (herbal medicine, massage, therapeutic exercises, shiatsu, homeopathic and anthroposophical preparations, traditional medicine recipes, etc.), tested by the author’s many years of practice.
Men, take care of your health - this is the key to male strength!
Causes and prevalence
LVH is basically a genetic disorder caused by an altered or “mutated” gene. If the disease is genetic, it can be inherited (passed from parent to child) and is therefore often common in certain families. For this reason, it is recommended to screen first-degree family members (parents and siblings) if someone close to them has previously been diagnosed with LVHT.
The prevalence of LVH is not really known, although some have suggested that the disease affects men more often than women. Nowadays, more people are diagnosed with LVH because cardiography is now more advanced, so non-consolidated areas can be seen and diagnosed quite accurately.
LVHT is sometimes diagnosed in patients with dilated or hypertrophic cardiomyopathy.
Some statistics:
- LVHT is registered in 80% of cases in men.
- In children, LVH is most common, as it ranks third after hypertrophic and dilated forms of cardiomyopathy.
- Among diagnosed cardiomyopathies, LVHT is detected in 9.2% of cases.
- The total share of pathology accounts for 0.014% of cases (according to E. Oechslin).
Trabecular bladder
Trabecular bladder
In principle, this is not a complication in the usual sense, but a typical sign of the third stage of the disease, when the capacity of the bladder increases and the tension of the walls decreases. This weakness of the bladder leads to involuntary urination and the appearance of residual urine. With chronic overstrain of the bladder, already in the second stage, without proper treatment, the development of the so-called trabecular bladder is possible. In this case, the muscles of the inner layer constantly thicken and protrude into the cavity like a beam through the thin mucous membrane of the bladder. The depressions located between them are usually called pseudodiverticula. In rare cases, the integrity of the thin mucous membrane may be compromised, allowing urine to leak into the abdominal cavity, creating a life-threatening situation.
Examination methods
Malformations of the bladder and urethra, which have severe symptoms, require careful examination. After this, treatment tactics will be chosen. The bladder is examined first using ultrasound, and then using other, more complex methods.
When performing an ultrasound, you can see the shape and size of the bladder, the presence of stones, and determine whether there is stagnation of urine. This method is considered the most popular and comfortable for the patient.
If bladder atrophy in men is suspected, then in addition to ultrasound, MRI may be recommended. This study is even more informative. Using a tomograph, you can see the presence of neoplasms and various types of anomalies that cause deformation.
Invasive methods of examination include cystoscopy. It is performed using a special device called a cystoscope. It is inserted through the urethra to examine the features of the bladder from the inside.
X-rays with contrast injection can also help evaluate the condition of the organ, but are rarely performed today. This is due to a large list of contraindications.
Blood and urine tests are important for diagnosis. They can be used to see whether there is inflammation in the body.
When the diagnosis is determined, they proceed to the choice of therapeutic methods of assistance. Each pathology requires its own set of remedies. If a trabecular bladder is diagnosed, treatment will consist primarily of eliminating urine stagnation.
Tumors that interfere with the functioning of the bladder are removed surgically. Sometimes it is necessary to remove the entire organ if the tumors are malignant and metastases have occurred. Then, to restore the functioning of the urinary system, plastic surgery is performed, forming an artificial bladder.
If there are stones, first determine their size in order to understand how best to remove them from the body. To treat urolithiasis, medications are used that can dissolve and remove stones.
With frequent urination, many people ask the question of how to enlarge the bladder in men. Unfortunately, this is physically impossible to do. But it is quite possible to improve the functioning of the organ. The doctor will recommend therapy, after which the bladder will be able to hold more urine and then the number of trips to the toilet will be reduced. Often, such symptoms are caused by inflammatory processes, if there are no other organic disorders.
It is very important to deal with inflammatory pathologies in a timely manner, otherwise fibrosis of the bladder will develop. With it, the organ shrinks and shrinks, and its walls are replaced by connective tissue.
If the ligaments and muscles are weak, then gymnastics will be necessary. After childbirth, the bladder returns to normal on its own; it only takes some time to recover.
Treatment
The absence of symptoms in the patient allows not to carry out specific treatment. If the clinical picture of chronic heart failure is determined or problems arise with the electrical conductivity of the heart, then appropriate pathogenetic and symptomatic therapy is carried out.
Treatment is aimed at improving heart function and reducing the chance of developing any complications. The treatment plan is based on the results of diagnostic tests and clinical manifestations and is therefore individualized to the needs of the individual patient and the symptoms they are experiencing.
The drug treatment regimen may include any drugs from the following pharmacological groups:
- Anticoagulants - reduce the risk of blood clots forming in trabeculae, which can lead to blockage of blood vessels in the brain, that is, stroke. Blood clots can also form due to atrial fibrillation (abnormal heart rhythm). An example of an anticoagulant is warfarin, which may also be prescribed when the pumping function of the left ventricle is weakened.
- Diuretics (diuretics) - reduce the accumulation of any fluid in the lungs or other parts of the body, stimulate the kidneys to remove water from the body in the form of urine.
- ACE inhibitors (angiotensin-converting enzyme inhibitors) - they relax the smooth muscle around blood vessels, reducing the workload of the heart, and reduce blood volume, which makes the pumping organ easier to work with.
- Angiotensin II receptor blockers - drugs dilate (increase) the lumen of blood vessels, which helps lower blood pressure. They may be used if a person cannot tolerate ACE inhibitors.
- Beta blockers—reduce the rate and force of the heart's contraction by reducing the stimulating effect of adrenaline, which normally causes the heart to beat faster.
Surgical methods of treatment
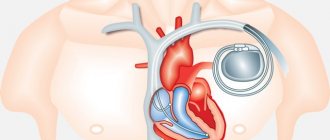
- Implantable cardioverter-defibrillator implantation - this option may then be used when a person experiences or is at risk of developing arrhythmias, which, if unfavorable, can lead to cardiac arrest.
- Pacemaker - a device that monitors the electrical activity of the heart and, if necessary, restores normal heart rhythm. This is important for people with arrhythmias such as heart block, which reduce the heart rate.
If there are concomitant diseases, they are treated accordingly. Otherwise, it will be difficult to control the course of LVH. Patients should be examined at least twice a year.