5 / 5 ( 1 voice )
Tachysystole is a collective concept used to designate disturbances in heart rhythm in the direction of its acceleration. Tachysystole includes several pathologies accompanied by accelerated contraction of the atria or ventricles. Some of them are relatively mild, while others are life-threatening.
Tachysystole is a type of arrhythmia
Characteristics of the concept
What is tachysystole? This concept comes from two words - “tachy” (quickly) and “systole” (contraction). Thus, tachysystole is an acceleration of heart contractions. The normal heart rate is between 60-80 beats per minute. Anything over 80 is called tachyarrhythmia.
These disorders are quite common in cardiology.
The following forms of tachysystole are distinguished:
- sinus tachycardia;
- atrial tachycardia, fibrillation and fibrillation;
- ventricular tachycardia and fibrillation.
Each condition has its own manifestations.
Normal heart rate
heart function is normal - in sinus rhythm
The concept of normosystole usually also refers to the fact that electrical signals that contribute to the sequential electrical excitation of all parts of the heart are generated in the sinus node, which is normally the first-order pacemaker. In all other cases, they speak of pacemaker migration or non-sinus rhythm. These processes are united by the concept of heart rhythm disturbances, or arrhythmias.
Therefore, usually in the ECG conclusion, in addition to the characteristics of the heart rate (HR), in the first place there is a mention of whether the patient has sinus rhythm or not. If the patient sees the term “normosystole” in the protocol, then most likely this means that he has not only a correct, normal heart rhythm, but also a sinus rhythm - that is, it comes from the sinus node, as it should be normally. (Nevertheless, there are formulations of “normosystole” with an even heart rate, but non-sinus rhythm - more on this at the end of the article).
Sinus tachycardia
This condition is not considered a disease and is not life-threatening. With sinus tachycardia, the heart rate exceeds 100 beats per minute.
There are two types of ST:
- Physiological . Appears with pronounced emotional excitement, physical stress, consumption of large doses of nicotine and caffeine. Physiological tachycardia is observed in young children and athletes.
- Pathological . Caused by certain diseases - anemia, fever, thyrotoxicosis, heart failure.
Symptoms of sinus tachycardia are rarely severe. A person may be bothered by a feeling of rapid heartbeat, interruptions in heart function, dizziness, and shortness of breath.
Sinus tachycardia is diagnosed by auscultation or by electrocardiogram. In the physiological form, it is necessary to avoid provoking factors and take sedatives. In the pathological form, the underlying disease is treated.
Sinus tachycardia is normal for newborns
Normosystole with atrial fibrillation
Of all rhythm disturbances, only this type of arrhythmia, such as fibrillation or atrial flutter, is divided into normo-, tachy- and bradysystolic variants. In this case, the diagnosis “atrial fibrillation, normosystole” indicates a pathology in the form of arrhythmia, but with a normal final heart rate.
normosystolic form of atrial fibrillation - despite the “waves” of atrial flutter/fibrillation, contraction of the ventricles of the heart occurs at a normal frequency
In this case, we are talking about both a permanent form of atrial fibrillation, when a person lives for a long time (months and years) with an irregular or non-sinus rhythm, and a paroxysmal form (paroxysm - attack), when a non-sinus rhythm occurs suddenly and may well recover spontaneously or with the help of medications. Diagnostic criteria are similar to those for normo-, brady- and tachysystole in sinus rhythm - from 60 to 80, less than 60 and more than 80 beats per minute, respectively.
With a permanent form of atrial fibrillation, normosystole is usually more easily tolerated by patients in terms of the sensation of interruptions in the work of the heart, since bradysystole is fraught with a decrease in cardiac output and resulting fainting, and the heart rate during tachysystole sometimes reaches 200 beats per minute, which can lead to severe circulatory disorders.
Supraventricular tachycardia
These conditions are associated with rapid contraction of the atria. There are several forms of pathology.
Table. Characteristics of atrial tachycardias:
| Form | Symptoms | Treatment instructions |
| Paroxysmal tachycardia - regular contractions are observed with a frequency of 150-230 per minute | Starts and stops suddenly. A person complains of an attack of rapid heartbeat and severe weakness. A decrease in pressure may be observed, and with significant hypotension, acute heart failure develops | You can stop the attack by inducing vomiting or coughing, inhaling with straining, and massaging the interclavicular fossa. The drugs used are adenosine or verapamil intravenously |
| Multifocal atrial tachycardia - the appearance of three or more consecutive extrasystoles | Usually not felt sick, numerous extrasystoles can cause weakness and dizziness | Verapamil is used intravenously |
| AV nodal tachycardia - increased frequency of atrial contractions up to 130 per minute | Manifested by dizziness. Usually occurs due to intoxication with glycosides, heart attack, heart surgery | Does not require specific treatment |
These diseases are also not life-threatening. For diagnosis, an electrocardiogram or Holter monitoring is used, where attacks of increased contractions are recorded.
Atrial fibrillation
This is an uncoordinated contraction of the muscle fibers of the atria, in which the heart rate reaches 700 beats per minute.
There are two forms of fibrillation:
- paroxysmal - lasts no more than two days;
- chronic - lasts more than two days.
Atrial fibrillation is registered in 0.5% of the population, but among people over 65 years of age it occurs in 5%.
Causes
30% of the population has an idiopathic form of the disease, that is, it has no apparent cause.
In the rest, the pathology develops against the background of cardiac and extracardiac diseases:
- heart attack;
- pericarditis or myocarditis;
- heart surgery;
- heart defects;
- hypertension;
- cardiomyopathy;
- alcoholism;
- thyrotoxicosis;
- TELA;
- electrical injury;
- pneumonia.
More often, the pathology develops against the background of heart disease. Many foci appear in the cardiac tissue that generate electrical impulses (photo). As a result, excitation and contraction of individual areas of the myocardium occur.
Mechanism of development of atrial fibrillation
Manifestations
Patients with atrial fibrillation complain of increased fatigue, dizziness, a feeling of rapid heartbeat, shortness of breath, and attacks of loss of consciousness. In some patients with underlying heart disease, signs of heart failure increase. Less commonly, there are no complaints - the asymptomatic form.
The examination reveals characteristic signs of the underlying disease. On auscultation, a rapid heartbeat is recorded.
Diagnostics
The diagnosis is confirmed after instrumental studies:
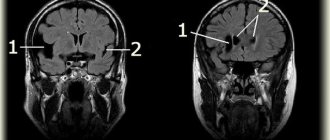
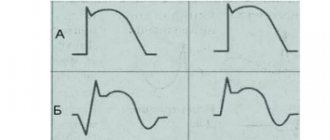
- ECG . There is an absence of P waves (normal atrial contractions); instead, specific f waves appear. There is an irregular heart rhythm.
- Holter monitoring . It is carried out to determine the number of attacks of fibrillation per day.
- Ultrasound of the heart . Detects heart disease, assesses ventricular function, and detects intracardiac blood clots.
To exclude thyrotoxicosis as a cause of fibrillation, the content of thyroid hormones in the blood is examined.
Therapeutic measures
Treatment goals for atrial fibrillation:
- restoration of normal rhythm;
- prevention of paroxysms of fibrillation;
- prevention of complications, primarily thromboembolic.
If the rhythm is severely disrupted, emergency defibrillation is performed.
Restoring a normal rhythm helps improve the patient’s overall well-being and reduces the risk of thromboembolic complications. For this purpose, first class antiarrhythmic drugs are used - Propafenone or Amiodarone. The drugs are administered orally or intravenously. In case of chronic fibrillation, anticoagulants are prescribed on a regular basis.
Surgical treatment is indicated when conservative methods are ineffective. It consists of destroying the AV connection with a radio knife and installing an artificial pacemaker.
A.M.Shilov PMGMU named after. I.M.Sechenova
The review examines risk factors for the development of cardiovascular diseases, including tachysystole. Data from epidemiological studies are presented, according to which increased heart rate is a risk factor for cardiovascular complications and should be considered by clinicians as a therapeutic goal. The results of our own study of patients are presented, which showed that an increase in the chronotropic reserve of the heart when prescribing cardioselective beta-blockers is the leading determinant in providing an antianginal effect and increasing exercise tolerance in patients with stable angina. Key words: stable angina, tachysystole, risk factors, bisoprolol.
Tachysystolic arrhythmia as a risk factor for cardiovascular disease AMShilov IMSechenov FMSMU The article reviews the risk factors for cardiovascular disease (CVD), including tachysystolic arrhythmia. The data from epidemiological studies revealed that increased heart rate should be considered as a risk factor for CVD and as an important therapeutic target. According to the author's own study, increasing of cardiac chronotropic reserve with selective b-blockers provides antianginal effect and exercise tolerance improvement in patients with stable angina pectoris. Keywords: stable angina pectoris, tachysystolic arrhythmia, risk factors, bisoprolol.
Information about the author Shilov Alexander Mikhailovich – Doctor of Medical Sciences, Professor, Perm State Medical University named after. I.M.Sechenova
According to analytical data from WHO experts, cardiovascular diseases (CVD) in 2010 occupied a leading place in the structure of mortality among the adult population in most economically developed countries of the world. Currently, in the countries of the European Union it is documented that CVDs are the main cause of every second death in the adult population and account for more than 1.9 million deaths per year. Research in the second half of the twentieth century put forward the concept of so-called “risk factors” (RFs), common to all CVDs: in particular, for coronary artery disease (in all its manifestations), hypertension, chronic heart failure (CHF), and cerebrovascular diseases. At the same time, the connection of the above pathologies with hypercholesterolemia has been convincingly proven. In the vast majority of cases, angina pectoris is a clinical manifestation of atherosclerosis of the coronary arteries as a precursor to acute coronary syndrome, MI and CHF. In turn, the risk of developing atherosclerosis increases significantly in the presence of risk factors such as old age, atherogenic dyslipidemia, arterial hypertension (AH), type 2 diabetes mellitus (DM), tobacco smoking, low physical activity, and excess body weight (BW). However, these lists of risk factors did not include such an indicator as heart rate (HR). At the beginning of the 21st century, increased heart rate at rest—tachysystole—began to be included in various diagnostic and treatment guidelines as one of the leading risk factors in the pathogenesis of the development and progression of CVD [1, 4, 10]. Modern recommendations for the diagnosis and treatment of CVD attach great importance to the identification and correction of risk factors for the development of pathologies of the cardiovascular system (CVS). These risk factors are largely universal, that is, they are characteristic of most CVDs and are well known. Currently, risk factors are divided into: “modifiable”: heart rate - tachysystole, obesity, cholesterol level, blood pressure level, presence of IGT or type 2 diabetes, smoking; “non-modifiable”: age, gender, race, family history; “soft” risk factors: low levels of HDL and a-lipoprotein, high levels of C-reactive protein, homocysteine, uric acid, tissue plasminogen activator-1, NFO-a, IL, etc. [2–6]. Each risk factor has its own share in the likelihood of developing a particular CVD disease. At the same time, the combined effect of several risk factors on one patient contributes to a significant increase in the risk of developing cardiovascular complications (CVD) (Fig. 1). It should be especially emphasized that the occurrence or progression of one disease is often a risk factor for the occurrence or progression of other cardiovascular diseases, primarily CHF. Moreover, the occurrence and progression of the disease is an evolutionary process in which one event becomes a logical continuation of the previous state and a predictor of the subsequent one. That is, RF, clinical manifestations of the disease and the outcomes of these diseases are interrelated phenomena, and the most likely link between these processes is endothelial dysfunction. In 1991, V. Dzau and E. Braunwald formulated the concept of a single “cardiovascular continuum,” which over the past 20 years of the late 20th and early 21st centuries has become firmly established in scientific and medical practice. In relation to practical medicine, “continuum” (from the English “continuous” - constant, continuous) implies a continuous sequence of stages in the development of the disease - from risk factors (RF) to death [11]. In 2001, at a joint meeting of the American College and the American Heart Association, stages of the cardiovascular continuum were developed and recommended: Stage A - these are years of prevention of RF and the beginning of treatment of any first signs of the disease using drugs to treat CHF. Stage B is years of treatment using all the preventive and therapeutic measures of stage A and the most important effective methods, including myocardial revascularization methods, which can effectively influence the progression of cardiovascular diseases and prevent their complications. Stage C consists of months of treatment with all the activities of stages A and B using drugs aimed at eliminating the complications and clinical signs of HF. Stage D is the most expensive and most difficult stage, when the patient often needs observation and treatment in intensive care units, in some cases he is forced to use cardiac resuscitation measures, implantation of an artificial left ventricle, cell therapy, heart transplantation, i.e. something that requires serious financial costs. Moreover, the financial costs of carrying out the first three stages are in total many times less than in stage D [2, 12]. Taken together, risk factors form a cardiovascular continuum, being both the cause and outcome at different stages and stages of pathology formation, ultimately leading to the development of chronic heart failure as the main cause of death (Fig. 2). The main risk factors, such as increased initial heart rate - tachysystole at rest, obesity, hypertension, diabetes, atherogenic dyslipidemia, represent the initial stage in the “cardiovascular continuum” - in a continuous sequence of pathophysiological events leading to progressive damage to cells of various organs, in particular , to damage to the arterial wall (remodeling) and ultimately to clinical manifestations of CVD. Carrying out treatment and preventive measures at an early stage of the disease (stages A and B of the cardiovascular continuum) can reduce morbidity (improve quality of life) and mortality (improve life prognosis) from CHF. Therefore, it is logical - early prevention of RF - pharmacological control of heart rate, adequate treatment of coronary artery disease, type 2 diabetes, arterial hypertension, CHF. Since ancient times, doctors have determined the patient's pulse to assess the state of health and prognosis of the disease. However, this assessment depended on the physician's knowledge and clinical experience. Relatively recently (the second half of the last century), scientific evidence was obtained of the influence of this important indicator on the quality and prognosis of human life. [4, 6, 8, 10, 15]. In the last two decades (the end of the 20th and the beginning of the 21st centuries), the scientific and clinical medical literature has recorded an increase in interest in the prognostic value of heart rate for a person’s life expectancy, especially among patients with existing pathology of the cardiovascular system, even with its latent course. Numerous epidemiological observational studies have provided evidence that heart rate is a risk factor for CVD in the general population of the world. These studies confirmed the important role of heart rate as an independent risk factor not only for cardiovascular mortality, but also for all-cause mortality. There is now compelling clinical evidence regarding the association of high heart rate (HR) with cardiovascular disease (CVD) and mortality [1, 7]. Back in 1986 and 1996. the prognostic significance of a persistent increase in heart rate as a risk of sudden death (SD) was confirmed by large Gothenburg and Framingham epidemiological studies: “... with an increase in heart rate, there is an increase in the rates of total and sudden death” [2, 13, 16]. In particular, in men, a high heart rate (>84 beats/min) is associated with a threefold increase in rates of sudden death compared with individuals whose heart rate did not exceed 68–75 beats/min, and a similar trend can be seen among women (Fig. 3). Data from a study of 30,729 patients in three countries (France, Italy and Japan) confirm that high resting heart rate is an independent predictor of cardiovascular mortality in men and all-cause mortality in both sexes. When comparing two groups of patients with heart rate ≥90 and ≤60 beats per minute, the risk of mortality was 2.4 times higher in the first group; with equal “traditional” risk factors, an increase in heart rate by 20 beats per minute leads to a 50% increase in the risk of mortality [17]. Currently, the independent role of heart rate in the prognosis of life of patients with coronary heart disease and heart failure has been documented (data from the McAlister meta-analysis) - the improvement in the prognosis of patients with heart failure is determined by the severity of the decrease in heart rate. The validity of this approach was fully confirmed by the recently completed large, prospective SHIFT study (SHIfT), which included more than 6.5 thousand patients with CHF from 37 countries, with an average follow-up of 2 years. The SHIFT results showed that, against the background of a decrease in heart rate by an average of 10.9 beats per minute over 28 days, as a result of taking Coraxan, the risk of death from CVD or hospitalization for CHF decreased by 18% (p84 beats per 1 minute [13, 14] The CASS (Coronary Artery Surgery Study), which included a 15-year follow-up of 25,000 patients, analyzed the long-term prognostic significance of resting heart rate on the course of suspected or documented coronary artery disease, which convincingly demonstrated the negative impact of an increase in resting heart rate on the quality and duration of life of patients. A number of publications show a highly reliable direct correlation between heart rate and the incidence of myocardial infarction during 5-10 years of observation of patients. In 2005, data from the study “The Cooper Clinic Mortality Risk Index” were published, in which, based on developed a scoring system for assessing the probability of death from all causes among 21,766 men aged 29–69 years without clinically obvious serious diseases, showed a one and a half times (1.46) increase in the risk of death with a heart rate ≥80 beats/min, and optimal, with from a prognosis point of view, heart rate was ≤59 beats/min [14]. A study conducted in Russia, which included approximately 15,000 men and women over the age of 35 years, analyzed long-term follow-up results on the effect of heart rate on mortality rates. This study found an inverse relationship between resting heart rate and cardiovascular morbidity and mortality, and resting heart rate was an independent predictor of survival [7]. Thus, according to epidemiological studies, increased heart rate is a risk factor for cardiovascular complications and should be considered by clinicians as a therapeutic target. Today, four classes of drugs with a pulse-lowering effect are used: cardioselective b-blockers (Bisoprolol), cardiac glycosides (Digoxin), if-channel blockers (Coraxan), physiological calcium antagonists (magnesium preparations - Magnerot). Bisoprolol (Concor) is a highly selective b1-blocker that does not have internal sympathomimetic activity and a membrane-stabilizing effect, with a long half-life (10–12 hours). In therapeutically recommended doses (from 2.5 to 10 mg), the drug exhibits almost no antagonistic activity against b2-adrenergic receptors and therefore does not cause metabolic effects such as hyperglycemia, dyslipidemia or hypokalemia, does not have an angiospastic effect on the arteries, and does not cause bronchospasm. From the standpoint of the above, in order to study the effect of cardioselective beta-blockers, we examined and treated 51 patients with stable angina (Classification of the Canadian Society of Cardiology) over the age of 50 years (the average age in the group as a whole was 56.7 ± 3.4 years), of which there were 36 men and 15 women. The basic treatment for IHD was the drug bisoprolol from 5 to 7.5 mg per day (the average daily dose for the subgroup was 6.2 ± 0.4 mg). In order to identify the frequency of ischemic attacks, patients included in the study program underwent 24-hour ECG and blood pressure monitoring on a Card(X)plore bifunctional monitor (Hungary). The functional class of angina was determined using a stress test - the number of meters covered in 6 minutes without “discomfort in the heart” under ECG monitoring (Table 1). To objectify the diastolic function of the left ventricle and the global pumping activity of the heart, all patients underwent Doppler-EchoCG examination. The studies were carried out using a Vivid 3 device (General Electric Medical System, USA), a sensor with a frequency of generated signals of 7.5 MHz, followed by calculation of heart pump performance parameters (MO, l/min; SI, l/min/m2; SV, ml ; EF, %) and the functional state of left ventricular diastole (E, m/sec – the speed of early diastolic relaxation; A, m/sec – the speed of late diastolic relaxation; DT, msec – the time of slowing down the blood flow in diastole to atrial systole; LVVIvRZh, msec – time of isovolumetric relaxation of the left ventricle). According to the level of exercise tolerance, in general, in group II FC was registered in 22 patients (43.1%), III FC – in 29 patients (56.9%); In subgroups A and B, patients with FC II–III stable angina were evenly distributed. The frequency of ischemic episodes (requiring the use of short-acting nitrates) in the group as a whole was 9.3 ± 0.9 per day. The results of ultrasound examination of patients before and after treatment are presented in table. 2. After the treatment, against the background of a decrease in heart rate from 82.1±7.6 to 64.6±3.5 per 1 min – an increase in chronotropic reserve by 21.7%, a statistically significant decrease in the number of ischemic episodes was noted (almost twice) by 54.9% (from 9.3±0.9 to 4.2±0.5 per day, pLiterature 1. Andreicheva N., Galeeva Z. Pulse-lowering and anti-ischemic effects of ivabradine. Vrach. 2011; 2: 48–52 2. Belenkov Yu.N. The contribution of various risk factors to cardiovascular mortality. What unites them? Plenum. Supplement to the journal “Heart.” 2006; 5 (5): 1–3. 3. Diagnosis and treatment of heart failure. Russian recommendations (third revision). Developed by the Expert Committee of the All-Russian Scientific Society of Cardiologists. Heart failure. 2010; 11: 1 (57). 4. The Beautiful study is a step forward in the treatment of coronary heart disease. Med. Vestn. 2008; 30: 3– 8. 5. Karpov Yu. Treatment of patients with stable angina: towards the release of new recommendations VNOK.RMZh. 2008; 16: 21: 1379–1381. 6. Basic provisions of the recommendations of the European Society of Cardiology for the management of patients with stable angina (2006). Effective pharmacotherapy in cardiology and angiology. 2007; 2:1–9. 7. Shalnova S.V., Deev A.D., Oganov R.G. and others. Pulse frequency and mortality from cardiovascular diseases in Russian men and women. Results of an epidemiological study. Cardiology. 2005; 10:45–50. 8. Boraso A. Why is reduced heart rate beneficial. Dialogues in Cardiovascular Medicine. 2001; 6:19–24. 9. Casstelli WP, Levy D, Wilson PWF et al. Sudden death: The view from Framingham. The Prevention of Sudden Death. New York. 1990; 1–8. 10. Diaz A, Bourassa M, Guertin MC et al. Long-term prognosis value of resting heart rate in patients with suspected or proven coronary artery disease. Eur. Heart J. 2005; 26:867–874. 11. Dzau V., Braunwald E. Resolved and unresolved issues in the prevention and treatment of coronary artery disease: a workshop consensus statement. Am Heart J. 1991 Apr; 121(4 Pt 1): 1244–63. 12. Gillum RF, Makuc DM, Feldman JJ and all. Pulse rate, coronary heart disease and death: NHANES I epidemiologic follow-up study. Am. Heart J 1991; 121:172–177. 13. Goldberg R., Larson M., Levy D. Factors associated with surviving to 75 years of age in middle-aged men and women: the Framingham Study. Arch. Intern. Med. 1996; 156:505–509. 14. Janssen I., Katzmarzyk P., Church TS et al. The Cooper Clinic Mortality Risk Index. Clinical Score Sheet for Men. Am.J.Prev.Med. 2005; 29: 194–203. 15. Jouven X, Empana JP, Schwartz J, et al. Heart-rate profile during exercise as a predictor of sudden death. N.Engl. J. Med. 2005; 352: 1951–1958. 16. Levin HJ Heart rate and life expectancy. J. Amer. Coll. Card. 1997; 30: 1104. 17. McAlister FF, Wiebe N, Ezekowitz JA et al. Meta-analysis: ß-Blocker Dose, Heart Rate Reduction and Death in Patients With Heart Failure. Ann. Intern. Med. 2009; 150: 784–790. 18. Teerling JR Ivabradine in heat failure – no paradigm SHIFT. Lancet. 2010; 376:847–849.
Atrial flutter
This is a regular contraction of the atrium muscle with a frequency of 250-300 per minute. It is rarely observed, as it is an unstable condition that quickly turns into a normal rhythm or fibrillation. It can be paroxysmal or chronic.
The causes and symptoms of flutter are no different from those of fibrillation. The ECG shows sawtooth F waves at the site of the P waves.
Treatment is similar to fibrillation.
F waves in atrial flutter
Paroxysmal ventricular tachycardia
This is a condition that occurs as a result of the appearance of three or more ventricular extrasystoles following each other.
Causes
There is an idiopathic form that occurs for no apparent reason. In other cases, ventricular tachycardia develops against the background of any heart disease. An ectopic focus forming in the ventricle causes its extraordinary contractions.
Symptoms
The clinical picture of paroxysmal tachycardia is poor. The patient complains of dizziness, clouding of consciousness. A decrease in pressure is objectively determined.
Diagnostics
Ventricular tachycardia is determined using an electrocardiogram. There is a deformation of the QRS complex (contraction of the ventricle), overlapping of the atrial and ventricular complexes.
Treatment
In most cases, the condition does not require specific treatment. A persistent attack of VT is treated with intravenous lidocaine. Signs of hemodynamic compromise require defibrillation.
Ventricular fibrillation and flutter
These rhythm disturbances are characterized by uncoordinated contraction of the ventricles at a rate of 250-300 per minute. On the ECG it is recorded as a sinusoidal curve. Leads to cardiac arrest and clinical death.
Emergency defibrillation is required and resuscitation measures are taken. To prevent this condition, patients have a cardioverter-defibrillator installed in the heart area.
Tachysystolic heart rhythm disturbances are a large group of conditions characterized by various types of increased heart rate. Some of them are safe for life and do not cause any clinical manifestations. Some arrhythmias are life-threatening and require urgent treatment.
Common deviations from the norm (brady- and tachysystole)
Sometimes the ECG conclusion may include a combination of normosystole and irregular sinus rhythm - “normosystole, irregular rhythm.” The latter can occur, for example, with respiratory or sinus arrhythmia. In this case, the rhythm comes from the sinus node (as it should be normally), but there are minor functional fluctuations in the heart rate due to the phases of inhalation and exhalation (normally, when inhaling, the heartbeat speeds up slightly, and when exhaling, it slows down slightly). Therefore, if a patient sees a conclusion about normosystole with an irregular but sinus rhythm, there is no point in panicking.
When a patient experiences an increase or decrease in heart rate, the doctor describes this as tachycardia or bradycardia. But sometimes he may write about tachysystole or bradysystole, which literally means frequent or rare heartbeats, respectively. In this context (assuming sinus ri and “systole” are synonymous.
Again, tachysystole and bradysystole can occur both in a completely healthy person and in various diseases of the heart or other organs. Here everything depends on other nuances obtained from the ECG. But if a person has a sinus rhythm with a slightly slow heart rate (at least 50 per minute) or increased heart rate (90-100) - especially from excitement, then we can talk about normal indicators.