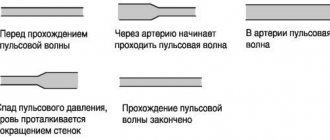
The main focus of the study is the registration of the electrocardiogram of the heart (atria, His bundle, ventricles), and the use of diagnostic stimulation to assess the electrophysiological parameters of the heart. There are non-invasive and invasive cardiac EPI.
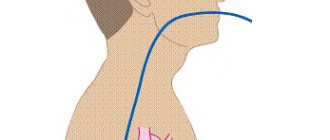
Transesophageal electrophysiological study (TEC cardiac EPS)
– a non-invasive method of electrophysiological examination of the heart, by introducing a diagnostic esophageal electrode through the nasopharynx (oropharynx) to a depth of 40-50 cm and recording an ECG. The examination is performed under local anesthesia (although more often without it) of the nasopharynx, the patient is in a supine position. The procedure usually does not require hospitalization. The study is performed on an outpatient basis (an EPI room or a cath lab) and usually takes no more than 20 minutes. Complications, as a rule, are not observed.
Endocardial electrophysiological study of the heart
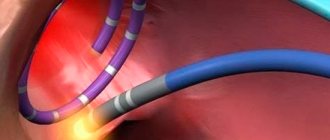
Endocardial electrophysiological examination of the heart (endoEPI of the heart) is carried out in a cath lab in compliance with the rules of asepsis and antisepsis under local anesthesia (“freezing”) from a small puncture (puncture) of vessels (femoral veins) and placement of introducers (“tubes”) through which into the heart catheters-electrodes are inserted under X-ray control. Using methods of electrical stimulation of the heart through inserted electrodes, the functional state of the cardiac conduction system is assessed and the mechanism and possibility of catheter ablation (destruction) of the tachyarrhythmia focus or an additional conduction pathway (WPW syndrome, etc.) is clarified. To conduct the study, the patient is hospitalized in a hospital, usually for 2 days. The study usually lasts up to 30-45 minutes.
The use of EPI in assessing the effectiveness of antiarrhythmic drugs
The transesophageal pacing (TEPS) method is predominantly used to evaluate antiarrhythmic drugs.
Electrophysiological serial drug testing allows for precise selection of medications that can effectively prevent arrhythmia paroxysms, as well as predict and monitor the duration of therapeutic success.
EPI in order to determine the antiarrhythmic effectiveness of medications is carried out if there are positive answers to the following two questions:
Is provoked tachycardia identical to spontaneous tachycardia?
Do changes in electrophysiological parameters observed during EPS with intravenous drug administration allow us to predict the effectiveness of treatment?
In clinical practice, there are absolute and relative indications for electrophysiological testing of medications:
I. Absolute:
1) History of attacks of cardiac arrhythmias, confirmed by EPI results.
2) Absence or loss of antiarrhythmic effectiveness of drug treatment, especially if there is a history of loss of consciousness or other signs of hemodynamic impairment.
II. Relative:
1) During EPI, no indications are found for the implantation of a pacemaker, defibrillator, or radical surgical treatment.
2) Against the background of electrical stimulation treatment, paroxysms of tachycardia occur - the need for combination with drug treatment.
3) Recurrence of tachycardia after surgical treatment.
4) The purpose of drug testing during EPI is to find an antiarrhythmic drug that stops tachycardia that is identical to that occurring spontaneously, or prevents its provocation.
After determining the possibility of provoking and stopping tachycardia, an acute pharmacological test is performed. For this purpose, against the background of induced paroxysm, no less than 5 minutes after its onset, the patient is slowly administered an antiarrhythmic drug intravenously, under monitor control, and its effect on arrhythmia is determined by conducting a comparative assessment of the electrophysiological parameters of the heart.
before and after drug administration. The dose of the drug should not exceed the calculated one (slide 18), but if restoration of sinus rhythm occurs earlier, the infusion can be stopped.
Initially, the relief effect of the drug is assessed. If, after a period of time sufficient for its manifestation, sinus rhythm has not been restored, vagal maneuvers are performed again. If they are ineffective, paroxysm is stopped with the help of ES, which does not exclude further evaluation of the protective effect of the drug.
After restoration of sinus rhythm, the study preceding the drug test is repeated to assess the protective effect of the drug. It should be noted that, in some cases, the same drug can stop paroxysm and not prevent its occurrence, and vice versa.
It is recommended to study the effectiveness of only one, or less often two, drugs within one day. Studying the effectiveness of several medications during one study is acceptable only if it is possible to determine the concentration of the drug in the patient’s blood so that the previous drug does not affect the effect of the subsequent one.
There are three possible modes of action of the drug:
I. positive action;
1) tachycardia stops;
2) the use of the drug prevents the (previously possible) provocation of arrhythmia;
3) stable tachycardia becomes unstable;
4) the duration of the cardiac cycle increases (heart rate decreases) during paroxysm.
5) difficulty in provoking paroxysm (narrowing of the “window” of tachycardia by more than half, the need for more aggressive methods of stimulation, the emergence of sensitivity of tachycardia to vagal techniques).
II. Absence of any effect on tachycardia.
III. Negative effect (arrhythmogenic effect):
1) paroxysms of tachycardia become more severe;
2) the aggressiveness of methods for inducing tachycardia is reduced;
3) side effects appear (they are also possible with the first two options for influencing tachycardia).
The presence of a protective effect allows the drug to be prescribed for oral administration in doses that allow it to achieve concentrations in the blood similar to those for intravenous administration. A few days later (after reaching the required concentration of the drug in the blood serum), the study must be repeated.
Reliable criteria for the effectiveness of selected antiarrhythmic therapy are the absence of paroxysms or a significant reduction in their frequency and duration, facilitating the conditions for their relief.
In conclusion, the following generalizations can be made:
1) EPI allows you to select antiarrhythmic drugs to stop and/or prevent paroxysms of tachycardia;
2) drug testing with EPI significantly reduces the time to search for an effective drug, while other testing methods (without the use of stimulation) are quite lengthy;
3) if all antiarrhythmic drugs are ineffective, indications arise for non-drug treatment (electric stimulation or radical surgery).
to the top of the page
Contraindications for endoEPI
- acute infectious diseases,
- acute myocardial infarction,
- unstable angina for 4 weeks,
- chronic heart failure III-IV f.k. according to NYHA,
- left ventricular aneurysm with thrombus,
- blood clots in the cavities of the heart,
- cardiac mechanical prostheses of the left chambers of the heart with access from the left.
When performing endoEPI, the incidence of complications does not exceed 1%. In order to prevent the latter, all necessary measures are taken at all stages of diagnosis and treatment.
The X-ray endovascular diagnostics and treatment room provides diagnosis and treatment of all types of arrhythmias (brady- and tachyarrhythmias). The department carries out operations within the framework of the state program for the provision of high-tech medical care (HTMC). This type of medical care is provided according to quotas allocated by the Russian Ministry of Health. Patients can also be operated on on a self-supporting basis, taking into account the cost approved by the Clinic.
Diagnostic application of EPI
The use of EPI in the diagnosis of arrhythmias and conduction disorders depends not only on the nature of the rhythm disturbances, but also on its clinical consequences. A number of tachyarrhythmias require immediate contact with a cardiac surgeon, since their therapeutic treatment is futile and even dangerous.
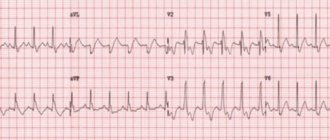
Before proceeding with invasive diagnostic tests, it is necessary to carefully review the results of noninvasive electrophysiological tests, ranging from 12-lead ECG to dynamic studies such as ambulatory Holter monitoring or exercise testing.
Necessary procedures for EPI
| Procedure | Target |
| History and physical examination | Detection and differential diagnosis of cardiac and neurological pathologies Determining the factors that provoke episodes of arrhythmia Detailing syncope |
| Neurological examination | |
| EEG | Exclusion of pathological activity of the central nervous system |
| CT/MRI | Identification of pathological foci |
| Carotid Dopplerography | Detection of significant cerebrovascular insufficiency |
| ECG in 12 standard leads | Cicatricial changes in the myocardium Intraventricular conduction disorders QT prolongation Ventricular preexcitation syndromes |
| Daily ECG monitoring | Correspondence between the occurrence of symptoms and changes on the ECG Quantification of ectopic activity Daily dynamics of arrhythmias |
| Orthostatic tilt test | Diagnosis of vasovagal/vasodepressor syncope |
| EchoCG | Determining the size of the heart chambers Contractility assessment Detection of local hypo- and akinesias Detection of intracardiac pathology |
| Stress test | Detection of transient ischemia Assessment of the arrhythmogenic function of catecholamines |
| CT – computed tomography; MRI – magnetic resonance imaging; CNS – central nervous system; EchoCG – echocardiography; EEG – electroecephalography. | |
Supraventricular tachycardia in young and practically healthy people sometimes causes minor symptoms or does not cause any symptoms. The same arrhythmia in a sick person with damage to the coronary arteries can cause angina, heart attack or congestive heart failure.
Rhythm disturbances can cause various neurological, cardiac, pulmonary and general symptoms. Reduced reserve capacity of the heart in cardiovascular and pulmonary diseases can aggravate existing clinical manifestations.
to the top of the page
Progress of the procedure
Considering that there are two types of research - invasive and non-invasive, there will be two ways to carry out the procedure.
Methodology for non-invasive EPI
The most commonly used non-invasive examination method, in which a catheter with an electrode is inserted through the nose or mouth, which is used somewhat less frequently. This method is also called transesophageal EPI or TEE. It is carried out in functional diagnostic departments, usually in the morning. The examination takes place as follows:
- Preliminary blood pressure measurement.
- Taking an ECG.
- The doctor explains the procedures and specifies what the patient will experience during the examination. There is usually a burning sensation in the chest, and this is normal.
- All manipulations usually take about half an hour.
- Through the nasal opening or, in rare cases, through the mouth, the doctor inserts a probe with an electrode into the patient, which is connected to special devices. Using equipment, stimulation of the heart muscle is carried out with electrical impulses. During this procedure, the heart begins to contract vigorously, as if under increased stress. All received data is recorded.
- An electrogram is recorded.
- The doctor carefully removes the catheter.
- A complete analysis of the collected information is carried out and a conclusion is made, which is sent to the attending physician.
- The tachycardia caused by the procedure will go away after some time, but if the discomfort continues for a long time, the doctor can provide medication.
Method of performing invasive EPI
In cases where TEE does not produce results or for some reason it is contraindicated, the doctor will prescribe endocardial or epicardial EPI.
Endocardial EPI
Before the procedure, the patient is placed in the department of cardiology, cardiac surgery or cardiac arrhythmology. EndoEPI itself is done in the department of X-ray surgical diagnostic methods. The patient is given an antisedative and taken to the operating room. Local anesthesia is performed. In complete sterility, the doctor makes an incision to insert a catheter into the femoral or subclavian vein. An introducer (metal or plastic guide) is inserted into the incision. A probe with an electrode is passed through it. The passage of the probe is observed on the screen. This is possible due to the available contrast agent. The probe is passed to the atrium or ventricle. The doctor performs electrical stimulation. All data is recorded using a computer.
This entire medical procedure lasts approximately half an hour. The patient should feel absolutely no discomfort. After removing the probe, apply a tight bandage to the insertion site.
Epicardial EPI
This study is carried out in the cardiac surgery department. The entire operation is performed under general anesthesia. The doctor dissects the chest and gains access to the pericardial cavity. Using electrodes, the doctor stimulates the epicardium. All data is recorded and then the wound is sutured. Typically, the operation lasts about an hour and is the most difficult area of examination using the EPI method.
Data decryption
The data obtained is deciphered by the doctor who performed this manipulation.
Normally, the doctor will note the presence of sinus tachycardia with a heart rate of 100 – 120 beats per minute. It goes away on its own and is not life-threatening for the patient. The doctor will note that all types of stimulation were performed and no deviations from the norm were found, which means that there are no types of arrhythmia that were suspected. Here the doctor will also indicate the absence of obvious signs of myocardial ischemia.
If the suspicions are confirmed, the type of arrhythmia and the parameters used for stimulation will be noted in the protocol. Next, the attending physician, based on the EPI analysis, will prescribe further treatment.
Complications after the procedure
Complications after such medical procedures are extremely rare, but they are still possible. Most often, negative consequences are expressed in the manifestation of acute heart problems. This is caused by artificially provoked tachycardia. Usually observed:
- severe paroxysmal angina;
- myocardial infarction;
- thromboembolism - may occur as a result of a detached blood clot that was not identified before the start of the study.
To avoid such undesirable consequences, a particularly thorough examination of the patient is required before the procedure begins.
After the examination, inflammatory processes or life-threatening arrhythmias may sometimes occur.