- What is atherosclerosis of the lower extremity vessels?
- Symptoms of the disease
- Risk factors
- Stages of development of atherosclerosis of the lower extremities
- Diagnostics
- Treatment
- Conservative treatment
- Surgical techniques
- Possible consequences and prevention
- Popular questions
Obliterating atherosclerosis (OA) of the arteries of the lower extremities
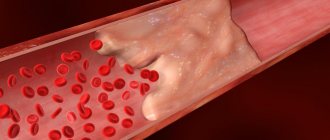
is a chronic vascular disease, which is based on lipid metabolism disorders, leading to the formation of atherosclerotic plaques, thickening of arterial walls and a decrease in the vascular lumen. As a result, ischemia develops - insufficient oxygen supply to cells and tissues.
Most often the popliteal, femoral and tibial arteries are involved in the pathological process.
OA of the arteries of the lower extremities is in first place among diseases of the peripheral arteries of atherosclerotic origin. According to literature data, obliterating arterial diseases account for about 16% of all vascular diseases Source: Podrezenko E.S. The influence of risk factors on the development of obliterating atherosclerosis of the vessels of the lower extremities / E.S. Podrezenko, S.S. Dunaevskaya // Health is the basis of human potential: problems and ways to solve them. - 2012. - pp. 576-578. .
Symptoms of atherosclerosis of leg vessels
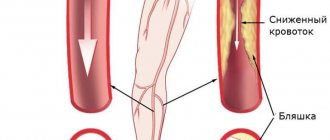
The development of the disease occurs gradually and in the first stages there may be nothing to show for it. Subsequently, the patient develops pain in the lower extremities, especially with prolonged walking, and a feeling of numbness in the feet. A decrease in temperature is felt on the legs, pallor and cyanosis are visible, and cramps occur. Over time, a person develops intermittent claudication and trophic changes occur in the form of delamination of nails and the formation of ulcers on the fingers and heels.
- with atherosclerosis, the patient may feel and observe the following:
- muscle pain in the legs, in the later stages even the feet hurt, and the pain cannot be relieved with painkillers;
- limited mobility of the affected leg;
- pain along the affected artery - first during physical activity, then at rest;
- intermittent claudication - after walking some distance, a person is forced to stand up and give his legs a rest, and then he moves on until the next attack of weakness;
- tingling, numbness in the affected area;
- thickening of nails;
- loss or slow growth of hair on the legs;
- paleness when raising the legs and sharp redness when lowering them;
- rapid freezing of feet;
- sores on the skin;
- purple fingers;
- absence of pulsation in the affected artery;
- areas of darkening on the skin are signs of the onset of gangrene in advanced stages;
- coldness of the skin of the leg;
- reduction in the mass and volume of the muscles of the thighs and legs.
At the beginning of the disease, as a rule, one limb suffers, then the process becomes symmetrical - this is a signal that the arteries are affected on both sides. An objective examination reveals the absence of pulsation in the popliteal fossa, thigh and ankle.
Complications
Vascular diseases of the lower extremities lead to forced limitation of physical activity and loss of ability to work. If the disease is caused by atherosclerotic plaques in the blood vessels, this is associated with a certain risk of complications:
- Critical ischemia of the lower extremities. With this disease, open ulcers appear that do not heal, damage or infectious lesions of the tissues of the legs. Critical limb ischemia occurs when injury or infection progresses and leads to tissue death (gangrene). In this case, amputation of the affected limb is performed.
- Stroke or myocardial infarction. Atherosclerotic plaques are not limited to the location only in the arteries of the legs. Fatty deposits form in the arteries of the heart and brain, causing the development of coronary heart disease and other diseases.
Even if you do not lead to the above complications, vascular diseases of the lower extremities are accompanied by very unpleasant symptoms: pain when walking and at rest, lameness, unpleasant sensations of chills, etc. If the vessels in the legs hurt, this prevents a person from leading a normal life, limiting him in physical activity.
Risk factors
The development of OA is based on the following most significant risk factors, the degree of influence of which can be different Sources: 1. Kuznetsov M.R. Basic principles of diagnosis and treatment of obliterating atherosclerosis of the arteries of the lower extremities / M.R. Kuznetsov // General medicine. - 2008. - No. 1. - P. 3-8. 2. Podrezenko E.S. The influence of risk factors on the development of obliterating atherosclerosis of the vessels of the lower extremities / E.S. Podrezenko, S.S. Dunaevskaya // Health is the basis of human potential: problems and ways to solve them. - 2012. - pp. 576-578. 3. Fattakhov V.V. Obliterating atherosclerosis of the lower extremities in the practice of a polyclinic surgeon / V.V. Fattakhov // Practical medicine. - 2010. - No. 2 (41). — P. 126-130. :
- male gender (men get sick 10 times more often);
- age (over 40 years);
- poor nutrition;
- overweight (obesity);
- smoking tobacco;
- hypokinesia (insufficient motor activity);
- hypofunction of the thyroid and gonads;
- heredity;
- some concomitant diseases (diabetes mellitus, coronary heart disease, heart rhythm disorders, lipid and carbohydrate metabolism, hypertension);
- exposure to adverse environmental factors.
Risk groups and concomitant diseases for atherosclerosis of the vessels of the lower extremities:
- male gender (distribution of disease: 85% men, 15% women);
- age 50 years and older, although the disease is getting younger;
- hereditary factor;
- smoking;
- diabetes;
- hypertension (high blood pressure);
- high cholesterol (infatuation with fatty foods);
Signs (symptoms) and stages of the disease
The main symptom signaling the onset of blockage of the arteries of the lower extremities is the so-called “intermittent claudication.”
When walking, pain appears in the muscles of the legs, which is characterized as “fettering”, “squeezing”, the leg seems to “go wooden”. The pain intensifies when running or climbing stairs. The location of the pain zones depends on the location of the compressed (affected) areas of the arteries. The most common pain is in the calf muscles. But pain can also occur in the muscles of the thighs and buttocks, which indicates damage to large arteries: the iliac, abdominal aorta. The extent to which circulation is impaired can be understood by the distance that the patient travels before the first attacks of pain appear.
Stages 1 and 2 : pain in the lower extremities after 500-1000 meters of walking, the toes go numb, the leg is cold, the skin of the lower leg and foot turns pale.
Stage 3 : pain occurs when walking short distances, up to 100 meters, hair loss on the lower leg, foot and toes, the skin acquires a purplish-bluish tint, wounds heal poorly, nail growth slows down, and deformation occurs.
Stage 4 : the legs hurt at rest, in a horizontal position, the pain temporarily subsides when lowering the legs down, then intensifies. Necrosis and tissue necrosis begin, non-healing trophic ulcers appear. Men experience impotence.
Stage 5 : gangrene of the leg develops, starting from the foot. Only surgical intervention and limb amputation can help save the patient’s life.
Atherosclerosis of the lower extremities occurring against the background of diabetes mellitus is especially dangerous. The disease progresses rapidly and leads to necrotic lesions and gangrene in just a matter of days and even hours.
Diagnosis of atherosclerosis of the lower extremities in our Center
Only comprehensive diagnostics using modern diagnostic systems provides reliable information on what stage of the disease the patient is at and what forms and methods of treatment will be most effective.
During the initial free consultation, the patient is interviewed and examined, complaints are listened to, visible changes in the skin are noted, and lesions are identified.
Further diagnosis of arteries is carried out using non-invasive painless methods: ultrasound scanning (ultrasound duplex scanning of the vessels of the lower extremities).
The walls of blood vessels are examined and assessed by a specialist, the speed of blood flow is established, and obstacles that disrupt healthy circulation are identified.
In severe forms of the disease, tests and additional diagnostic methods are prescribed (CT angiography of leg vessels, measurement of partial pressure of oxygen in tissues) in order to assess the patient’s condition in detail before surgery.
Modern treatment of atherosclerosis of the lower extremities
In the initial stages, it is possible to combine the use of medications and the use of physiotherapy, which includes a set of exercise therapy exercises and dosed (short) walking.
If there is a slight partial narrowing of the artery section, stenting is used: the affected artery is punctured, a catheter with a stent is inserted, which, using a compressed air cylinder, opens, expanding the narrow section and is fixed, thereby restoring blood circulation.
In case of serious disruption of blood flow, when the blocked areas of the vessels are prolonged, surgical methods are used to restore blood circulation:
- prosthetics or bypass surgery with a synthetic prosthesis (alloprosthesis);
- prosthetics or bypass with an autologous vein: using your own vein, a bridge is created, a bypass from the proximal to the distal end, that is, bypassing the blocked area;
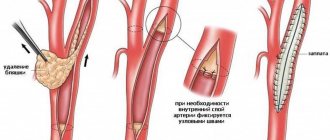
Profundoplasty is a surgical correction effective in terms of clinical results, which is performed for patients with occlusion of the superficial femoral artery and stenosis of the deep femoral artery with chronic ischemia of the lower extremities of severe stages. For this, endarterectomy from the deep femoral artery and angioplasty with a patch are used, which can be the patient’s vein or artery or special artificial synthetic substitutes. Today, profundoplasty is a method with highly proven effectiveness, which can be used to reduce the degree of ischemia and reduce the risk of limb amputation.
What to do for atherosclerosis of the arteries of the lower extremities
The first thing you need to know. Atherosclerosis is not a death sentence. Despite the fact that the vessels cannot be restored to their original form, with timely access to a vascular surgeon, the patient has every chance to continue to live and work fully. But even with serious changes and lost time, there are great hopes for the successful finalization of the process, which consists of preserving the lower extremities while following the doctor’s simple recommendations in the postoperative period. In our clinic, qualified vascular surgeons literally rescue people from the other world who were rejected by other medical institutions. We urge you not to be indifferent to your health, get free consultation, and, if necessary, stop atherosclerosis using modern methods of vascular surgery. Your operation can be performed free of charge, as it is high-tech assistance and is subject to quotas from budget funds.
Stages of development of atherosclerosis of the lower extremities
The most detailed is the modified classification of chronic arterial insufficiency of the lower extremities (CANF), which takes into account in detail the phenomena of critical limb ischemia, which is necessary when determining treatment tactics.
| Stage 1 | Muscle pain only during heavy physical activity (when walking over a distance of more than 1 km). Initial signs of stenosis appear - the skin turns pale, there is a feeling of goosebumps, it seems that the legs are always cold, fatigue quickly sets in when walking, excessive sweating is observed |
| Stage 2A | Feeling of fatigue and stiffness in the calf muscles, intermittent claudication after 200-1000 m |
| Stage 2B | Intermittent claudication in less than 200 m |
| Stage 3A | Intermittent claudication after a few steps or pain at rest when it is possible to keep the lower limb in a horizontal position for more than 2 hours |
| Stage 3B | Pain at rest, ischemic edema, inability to keep the lower limb in a horizontal position for 2 hours |
| Stage 4A | Gangrene of the fingers or part of the foot with the prospect of maintaining the supporting function of the limb |
| Stage 4B | Extensive necrotic changes in the limb without the possibility of maintaining its supporting function |
Thromboangiitis obliterans (Buerger's disease)
The disease is quite rare. The course and clinical manifestations are similar to obliterating endarteritis, but differ in a more aggressive course. One of the main symptoms that distinguishes Buerger's disease from other obliterating diseases of the extremities is migrating thrombophlebitis, mainly of the superficial veins. The disease is characterized by a chronic course with periodic exacerbations and remissions.
Treatment of thromboangiitis obliterans is not much different from therapy for endarteritis obliterans. If venous thrombosis occurs, they are treated according to the general rules (see treatment of venous thrombosis).
Diagnostics
There is a standard diagnostic program for this disease:
- Ultrasound of vessels of the lower extremities (duplex and Doppler scanning);
- coagulogram (determination of the blood coagulation system);
- determination of cholesterol and LDL levels in the blood;
- leg arteriography;
- establishment of pulsation in peripheral arteries;
- MR, MSCT angiography.
If prescribed by a doctor, MRI and CT scans with contrast and rheovasography can be performed.
To make a timely diagnosis of atherosclerosis of the vessels of the lower extremities, consultation with a vascular surgeon or phlebologist and a number of diagnostic measures are necessary.
Due to the systemic nature of the atherosclerotic process, patients with OA of the lower extremities often experience combined damage to various arterial basins, therefore, in such patients, an integral part of instrumental diagnosis is the study of extracranial and coronary arteries. Identification of pathology in them may require a change in treatment tactics or the order of surgical interventions Source: Kuznetsov M.R. Basic principles of diagnosis and treatment of obliterating atherosclerosis of the arteries of the lower extremities / M.R. Kuznetsov // General medicine. - 2008. - No. 1. - P. 3-8. .
Diagnosis of atherosclerosis of the extremities
To make a correct diagnosis and find out whether you have atherosclerosis of the lower extremities, you need to undergo a full examination. This will help to identify the degree of vascular patency and blood supply to the legs, determine the level of occlusion and the extent of vascular pathology in atherosclerosis.
1 Determination of pulsation of arteries of the extremities
2 Determination of pulsation of arteries of the extremities
3 Determination of pulsation of arteries of the extremities
To do this you need:
- get advice from a vascular surgeon;
- measure blood pressure in the arms and legs;
- determine the pulsation of the arteries of the limbs;
- undergo MCT angiography;
- undergo duplex scanning of peripheral arteries.
1 Consultation with a vascular surgeon in MedicCity
2 Ultrasound of arteries in MedicCity
3 Ultrasound of arteries in MedicCity
Treatment of atherosclerosis of the vessels of the lower extremities
The approach to treatment is determined depending on the stage of the disease and is primarily about choosing the right regimen. It is necessary to adhere to a diet limiting fried and fatty foods, eliminating smoking and alcohol, as well as combating excess weight. The patient should follow a walking and physical activity regimen, choose comfortable and spacious shoes, and treat even the smallest injuries on the skin of the lower extremities. Treatment of concomitant chronic diseases is mandatory.
Medicinal methods include anticoagulants, antiplatelet drugs, agents that improve blood microcirculation, vasodilators, and physiotherapeutic procedures.
In severe cases, surgical treatment may be necessary.
General recommendations:
- normalize weight;
- follow a diet with low cholesterol;
- give up alcohol and smoking;
- wear shoes that fit;
- do not overcool your feet;
- even minor injuries should be carefully treated and treated;
- trim nails carefully without damaging soft tissues;
- engage in moderate physical activity - walking, swimming, cycling or exercising on an exercise bike.
Vein disease of the lower extremities: causes, symptoms and stages of the disease
Varicose veins are a rather insidious disease. In the first stages, the disease is practically asymptomatic, although irreversible internal processes are already beginning to progress. The walls of blood vessels become thinner and lose their functional significance. The direction of blood flow is reversed. Veins carry blood to the heart and move upward against gravity. The system of venous valves prevents the reverse flow of blood by closing their valves in a timely manner.
In a damaged vessel, the operating mechanism fails. The wreath takes on a sinuous shape, changes its color and becomes a pronounced spot on the limb. Heaviness and swelling in the legs, fatigue, cramps and severe trembling of the calf muscles are added to the visual picture. With the development of subsequent stages, varicose veins acquire a deeper character, causing the patient severe pain, dizziness, chronic fatigue and swelling of the limbs. In case of complications, trophic ulcers may form and bleeding may develop.
Varicose veins of the lower extremities are not the only disease of the vascular system. Diseases of the venous vessels, depending on the severity and symptoms, can be divided into several characteristic types of disorders:
- Phlebitis is a venous disease that is characterized by inflammation of the lining of the superficial veins and impaired blood flow. The causes of phlebitis are complications of varicose veins, infection and damage to the vessel by chemicals. The site of inflammation swells and redness appears. The process is accompanied by pain and increased body temperature. If the symptoms are not treated, the disease will become chronic.
- Thrombophlebitis – deep vein thrombosis is an inflammation of the venous lining, which leads to the formation of blood clots or blood clots. Blood clots completely block the patency of the vessel, which can cause serious consequences with a fatal outcome. The main causes of thrombophlebitis are mechanical damage to a venous vessel, infection, tissue abscess, purulent wound or bleeding disorder. Symptoms: swelling, severe pain, change in skin color.
- Chronic or acute venous insufficiency of the lower extremities is a genetically predisposed circulatory disorder that leads to deformation of the walls of blood vessels and malfunction of the valve apparatus. The venous vessel begins to expand, swelling and heaviness in the legs appear. A kind of mesh pattern appears on the legs, which over time will stick out from under the skin tissue. The disease can also be caused by an inactive lifestyle with “sedentary” or “standing” work.
Risk factors and causes of the disease
Varicose veins usually affect women. An additional risk factor is pregnancy, when hormonal changes occur in the body of the expectant mother and all body systems fail. Men get sick less often, but their symptoms are more pronounced and fleeting.
Also, varicose veins can be caused by reasons that the patient cannot control and correct. These are bad genetics (several people in the same family suffer from the disease), age over 40 years, gender, the presence of other vascular disorders, which can be a provoking factor. Often the disease is caused by everyday factors, by eliminating which you can return the condition of the blood vessels to normal and relieve all symptoms:
- Monotonous work in one position;
- Inactive lifestyle, lack of physical activity;
- Excess weight;
- Alcohol abuse, smoking;
- Improper diet and impaired water balance;
- Passion for saunas and steam baths, sun tanning;
- Tight clothes and uncomfortable high-heeled shoes.
Symptoms of vein disease
Varicose veins of the extremities have a variety of symptoms depending on the stages of development of the disease and the severity of their course.
Stage 0-1 – symptoms of varicose veins are practically absent. Externally there are no signs of varicose veins. You may feel slightly tired at the end of the working day. These signs may indicate varicose veins.
Stages 2-3 – venous vessels become noticeable and more pronounced. Fatigue is accompanied by swelling and pain with periodic intensification of pain.
Stage 4 – strongly pronounced altered vessels in the form of convoluted cords, trophic changes in the skin and subcutaneous tissues, hyperpigmentation of the varicose veins. Tissue atrophy or eczema formation is possible. Characterized by severe pain in the limbs, itching, burning.
Stages 5-6 - to all the symptoms listed above are added a trophic ulcer of the open and closed type, bleeding of the damaged vessel.
Treating atherosclerosis
- Shishkin A.A.
- Volkov A.M.
- Kabirov A.V.
- Baranov V.S.
Shishkin Andrey Andreevich
Candidate of Medical Sciences. Surgeon, proctologist, phlebologist at SM-Clinic. Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
Read moreVolkov Anton Maksimovich
Phlebologist, surgeon at SM-Clinic. Performs operations with a modern proprietary method of treating varicose veins using a laser (modified endovenous laser coagulation. M-EVLC).
Surgical treatment of varicose veins of any complexity (phlebectomy, miniphlebectomy) More detailsKabirov Alexander Vitalievich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
More detailsBaranov Vladimir Sergeevich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Treats lower varicose veins using non-surgical and surgical methods (aesthetic sclerotherapy, ECHO sclerotherapy, stem sclerotherapy, phlebectomy, miniphlebectomy, EVLT).
More details
Treatment of varicose veins
To eliminate varicose veins, both conservative and surgical techniques are used. The patient is recommended to wear compression products (stockings, tights or knee socks) and periodically take medications to strengthen the walls of venous vessels (Troxevasin, Detralex, Cyclo 3 Fort, etc.). For local application, agents such as Lyoton, Curiosin, Venoruton, Heparin ointment, etc. are used. To normalize the condition of veins and blood flow, physiotherapy can be prescribed: amplipulse therapy, local darsonvalization, intermittent pneumocompression, magnetic therapy, hyperbaric oxygenation, laser therapy, balneo- and hydrotherapy.
As a minimally invasive technique for minor manifestations of varicose veins, sclerotherapy can be performed - the introduction of a sclerosant drug (for example, Fibro-Vein, Athoxysclerol, Sodium tetradecyl sulfate, Sclerowein, etc.) into the dilated areas of the veins, causing “gluing” of the pathologically dilated vessel. Other minimally invasive techniques can be used to remove varicose veins - ablation using laser or radiofrequency ablation. These procedures seem to seal the dilated vessels. In other cases, traditional surgical interventions are performed to remove veins, consisting of ligation or removal of the large and sometimes small saphenous veins. They are performed using different methods (stripping, miniphlebectomy, crossectomy) and can be supplemented with minimally invasive methods. The patient may also be prescribed some endoscopic types of interventions: endoscopic dissection and transluminal phlebectomy.
Conservative treatment
The patient may be prescribed various medications:
- prevent the formation of blood clots, prevent stroke and heart attack;
- increasing physical activity, improving blood flow in the lower extremities;
- antiplatelet drugs that lower blood cholesterol levels;
- anticoagulants, which prevent blood clotting in blood vessels and prevent blood clots;
- antispasmodics to relieve pain and spasms;
- antimicrobial ointments that need to be used to treat trophic ulcers;
- medications that promote better tissue nutrition;
- vasodilators;
- vitamins.
Also, as part of conservative therapy, physiotherapy is performed - electrophoresis with novocaine, darsonvalization, hyperbaric oxygenation.
Causes
The causes of obstruction of the vessels of the lower extremities are the following:
- Obliterating endarteritis. As a result of the inflammatory process localized in the vessels, their lumen gradually narrows, causing complete or partial ischemia.
- Obliterating atherosclerosis. This disease can cause acute arterial obstruction of the great vessels of the lower extremities. Obliterating atherosclerosis develops under the influence of lipid metabolism disorders and is characterized by the formation of plaques on the walls of the arteries.
Causes of obstruction of blood vessels in the legs
- Thrombosis. The formation of blood clots (blood clots) in the vessels of the lower extremities is usually caused by increased blood viscosity, injuries, and varicose veins.
Surgical techniques
Surgery is a last resort and is usually prescribed for severe ischemia and very severe complications. Nowadays, different types of surgical interventions are performed. Some involve a day hospital, some require a long-term hospital stay under observation. Patient rehabilitation plans and post-operative care vary. Our doctors advise patients in detail on all aspects related to surgical intervention and carefully monitor their health in the pre- and postoperative period.
Surgical treatment of atherosclerosis of the lower extremities:
- bypass surgery - an additional “bypass” path for blood flow is created around the area of narrowing of the artery;
- stenting - a special tubular spacer is placed in the affected vessel, which ensures the required diameter of the artery;
- balloon angioplasty - similar to stenting, only a balloon is inserted into the vessel cavity rather than a spacer, which expands its lumen;
- autodermoplasty - if trophic ulcers are poorly treated conservatively, they are operated on and covered with the patient’s own skin;
- endarterectomy - removal of the affected part of the artery in which the atherosclerotic plaque is located;
- prosthetics – replacement of the affected vessel with the patient’s own vein, taken from another place, or with a synthetic prosthesis;
- amputation - prescribed in severe cases when gangrene occurs, after which prosthetics are performed.
In 75-85% of cases, after surgery, blood circulation is completely restored for an average of 5-8 years.
Indications for surgery:
- an aneurysm that may rupture;
- chronic ischemia of critical stage;
- hemodynamically significant carotid artery stenosis or plaque accompanied by symptoms of cerebral ischemia;
- decompensation of blood circulation in the leg due to embolism, trauma, thrombosis.
Contraindications to surgical treatment:
- wet gangrene with sepsis;
- severe disruption of vital organs - renal and liver failure, circulatory disorders in the brain, myocardial infarction, heart failure, etc.
Treatment
In the early stages of the disease, drug treatment aimed at preventing the development of atherosclerotic plaques and improving the rheological properties of blood is acceptable. For this purpose, statins and antiplatelet agents (aspirin) are used.
If the lumen of the vessel is so closed that the blood supply to the limb is disrupted, surgical treatment is necessary:
- balloon dilatation and stenting of the vessel (expansion of the narrowed part and installation of a stent to prevent re-narrowing of the lumen),
- endarterectomy (removal of plaque with the inner layer of the vessel),
- shunting (creating bypass paths for blood flow around an irreversibly damaged area of the vessel).
Possible risks associated with the disease
The disease is insidious in that it is impossible to predict its course and symptoms. Approximately 20% of patients over 65 years of age, having severe plaques, do not feel any discomfort. The seriousness of the progressive course of OA ANC is also due to the fact that after the appearance of the first symptoms, 10-40% of patients develop gangrene within 3-5 years, which leads to amputation of a limb or death Source: Kazantsev A.V. A new approach to surgical tactics for obliterating atherosclerosis of the arteries of the lower extremities / A.V. Kazantsev, E.A. Korymasov // Saratov Medical Scientific Journal. - 2010. - T. 6. - No. 4. - P. 850-856. .
Atherosclerosis can be complicated by arterial thrombosis. This complication, if not immediately sought by a doctor, leads to loss of a limb or embolism of other arteries. If the clot detaches and enters the coronary artery, a myocardial infarction may develop, and if it migrates to the carotid artery, a stroke may occur.
Data from laboratory and instrumental examination methods
Laboratory examination allows us to identify patients at risk of developing atherosclerosis (increased blood cholesterol, atherogenicity index), identify patients with diabetes mellitus (increased blood glucose levels), which significantly complicates the course of the disease, and assess the state of the blood coagulation system (coagulogram). Culture from a trophic ulcer allows you to identify the causative agent of infection and prescribe rational antibiotic therapy.
Instrumental methods.
The most accessible and informative method, successfully used in outpatient settings, is currently recognized as duplex ultrasound scanning of the arteries of the lower extremities (USAS) - an ultrasound method that allows you to assess the condition of the vascular wall, identify atherosclerotic plaques, determine the level and extent of arterial occlusion, and assess the type blood flow, measure important indicators (brachial-ankle index, etc.). The study should be carried out in all patients suspected of having any stage of CANDC.
Currently, surgeons in Moscow practically do not use rheovasography (RVG) in the diagnosis of OASNK, because it allows you to determine only the deterioration of the arterial blood supply to the lower extremities, which is easily diagnosed based on clinical signs and USAS data.
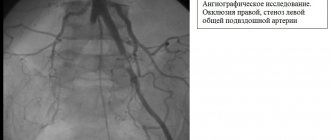
Angiography is a radiopaque research method used in a hospital setting to clarify the localization of the process and select the method of surgical intervention. The method is highly informative, but since it is not used in outpatient practice, we will not dwell on it in detail.
Microcirculation disorders are determined using capillaroscopy, transcutaneous determination of oxygen tension in superficial tissues and laser Dopplerography - they are of more scientific than practical interest.
Prevention methods
For prevention purposes, you need to start controlling the levels of lipids, sugar and cholesterol in the blood as early as possible. Even with a slight increase in numbers relative to the norm, you should consult a doctor. It is also recommended to regularly do ultrasound of the lower extremities - once every 1-2 years.
It is important to watch your diet, because the reason for the increase in “bad” cholesterol in the blood is the saturated fats that we consume in food. These are products of animal origin - fatty meat, lard, butter. There is a lot of cholesterol in eggs, or rather in the yolks. All these products should be consumed in the smallest possible quantities.
| Name of service (price list incomplete) | Price, rub.) | In installments* |
| Appointment (examination, consultation) with a cardiovascular surgeon, primary, therapeutic and diagnostic, outpatient | 1 750 | — |
| Program “Risk of atherosclerosis and ischemic heart disease, predisposition to dyslipidemia” | 19 000 | — |
* You can read more about the conditions here - Treatment on credit or in installments.