Home — For the public
- Map of medical organizations
- Vaccination
- Clinical examination
- Fluorography
- Addresses and opening hours of clinics
- Emergency rooms
- Oncology
- Where to take an HIV test
- Healthy child's office
- Services
- Prevention of CVD
- Disease Prevention
- World Patient Safety Day
- Newspaper "Medical News"
- specialist
- School of Health
— Disease prevention
- HIV infection
- All about vaccination
- All about proper nutrition
- Hepatitis
- Flu
- Dementia
- Schoolchildren's health
- STD
- Tick-borne encephalitis
- Whooping cough
- Measles
- Legionellosis
- Meningococcal infection
- Oncology
- Acute intestinal infection
- Pediculosis
- First aid
- Pneumococcal infection
- Pneumonia
- Prevention of rabies
- Dependency Prevention
- Rotavirus infection
- Diabetes
- Cardiovascular diseases
- Injuries
- Tuberculosis
- Tularemia
- Physical activity
- Obstructive pulmonary disease
- Exotic infections
- Ecology
- Why is swimming in ponds dangerous?
— Cardiovascular diseases — Disease of peripheral arteries and veins
Diseases of peripheral vessels and arteries are a group of inflammatory diseases, which in most cases are accompanied by damage to the arteries and veins of the lower (less often, upper) extremities. With these pathologies, a narrowing or significant expansion of the lumen of blood vessels occurs, blood circulation and tissue nutrition in the affected areas are disrupted.
A number of these diseases are caused by atherosclerotic changes in the walls of the arteries, and varicose veins or aneurysms of the aorta and arteries are provoked by pathological overstretching of the venous and arterial walls. The diagnosis is established on the basis of a physical examination and the results of some instrumental studies, which make it possible to visualize the nature of changes in the walls of blood vessels. In severe cases, patients with such diseases may require surgical operations to correct vascular pathology; in milder cases, the resulting disorders can be eliminated conservatively.
Obliterating atherosclerosis
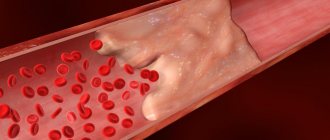
Peripheral artery disease (PAD) in most cases is caused by atherosclerosis, another systemic disease characterized by abnormalities in the structure of the artery walls. Atherosclerotic plaques form in the lumen of the vessels, leading to the settling of blood clots, narrowing of the arterial lumen and the appearance of areas of thrombosis. As a result, the trophism of the tissues surrounding the affected vessels is disrupted, they begin to suffer from ischemia (insufficient blood flow) and the patient develops obliterating atherosclerosis.
Thrombosis usually affects the vessels of the lower extremities at the level of:
- abdominal aorta (Leriche syndrome) – the infrarenal section of the abdominal aorta narrows and blood circulation is impaired in both legs;
- pelvis – the iliac artery is affected;
- hips – the lumen of the femoral artery is blocked;
- shins – blood clots settle in the arteries of the legs and feet.
With significant narrowing of the peripheral arteries of the legs, tissue trophism can be so disrupted that the patient develops trophic ulcers due to constant ischemia and gangrene can develop, leading to the need for amputation of the leg. In addition, atherosclerosis is prone to progression and the patient’s risk of developing myocardial infarction and stroke increases in the future, since both the coronary and carotid arteries are involved in the pathological process.
The process of occurrence and spread of atherosclerotic plaques occurs unnoticed in almost 50% of patients. Often, patients with such pathologies consult a doctor only when conservative treatment methods are not enough to restore blood flow and there is a need for surgical correction of the affected arteries.
The causes of PAD are the same as the factors that provoke the development of atherosclerosis:
- *imbalance in lipoproteins and accumulation of cholesterol in vascular walls;
- autoimmune pathologies accompanied by infiltration of vessel walls with leukocytes and macrophages;
- congenital defects in the structure of blood vessels;
- hormonal imbalances of adrenocorticotropic and gonadotropic hormones, leading to increased cholesterol levels in the blood;
- failures in antioxidant systems;
- brought infections.
*Elevated is considered to be a total cholesterol level of more than 8 mmol/l, an HDL level in men of less than 1 mmol/l and in women less than 1.3 mmol/l, an LDL level of more than 6 mmol/l, and a triglyceride level of more than 1.7 mmol/l.
All these reasons can trigger the process of formation of atherosclerotic deposits, but the leading role in damage to peripheral arteries lies in lipid balance disorders. According to statistics, men over 40–45 years of age are more likely to encounter such pathologies.
The following controllable and uncontrollable factors can predispose to the development of atherosclerotic lesions of the arteries:
- age (for women after 55 years and men after 45 years);
- smoking;
- postmenopausal period;
- excess weight and waist circumference in women is more than 88 cm, and in men more than 100 cm;
- arterial hypertension more than 180/110 mm Hg. Art.;
- diabetes;
- hypothyroidism;
- hereditary disorders (coagulopathies, homocystinuria);
- hereditary predisposition to vascular and heart diseases;
- congenital vascular anomalies;
- adynamia;
- taking a large amount of fast food, fatty, fried, flour, sweets, baked goods, carbonated drinks;
- taking medications that increase blood cholesterol levels;
- taking hormonal contraceptives;
- disorders in the blood coagulation system, accompanied by increased thrombus formation;
- frequent stress;
- chronic sleep deficiency.
Uncontrollable factors cannot be eliminated. They contribute to the formation of atherosclerotic plaques, but in the absence of controlled conditions are not capable of causing obliterating atherosclerosis.
With the development of atherosclerosis, the following occurs:
- on the inner wall of the artery, a lipid stain is formed that transforms into liposclerosis, leading to the formation of unstable atherosclerotic plaques, which can still dissolve;
- fibrous plaques appear that can no longer resolve, and atheromatosis develops, accompanied by the disintegration of the contents of plaques, collagen and elastin in the vessels;
- when plaques disintegrate, the stage of complications of atherosclerosis begins: thrombosis, embolism, rupture of the aneurysm formed in the lumen of the artery;
- the formation of atherocalcinosis - this stage is accompanied by the deposition of calcium salts in the atherosclerotic plaque and severe ischemia of tissues and organs.
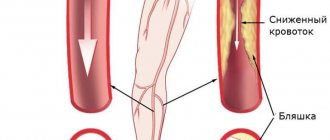
Symptoms of peripheral artery disease do not appear immediately, but only at the stage of severe ischemia of a particular area. Initially, the patient complains of pain, cramps and fatigue in the legs after walking or physical activity. The pain is usually located in the thighs, buttocks and feet. Sometimes patients may experience swelling. There is also no pulsation in the area of damage to the arterial vessel. The skin on the affected limb becomes paler and cooler to the touch at the level of the arterial lesions. Men may experience problems with potency due to impaired blood flow.
Somewhat later, the patient develops a symptom characteristic of obliterating atherosclerosis of the lower extremities, such as intermittent claudication (claudication) - pain and cramps in the calf muscles, aggravated by walking. It is provoked by a lack of oxygen, which is most pronounced during walking, and disappears after the person stops.
Intermittent claudication is most pronounced when climbing stairs. Initially, it occurs after walking long distances, and then, as atherosclerotic lesions of the arteries and ischemia progress, it appears even after covering very short distances. In the most advanced stages, it occurs even during rest. This condition is commonly called critical ischemia.
The stages of PAD are:
- I – symptoms of thrombosis and narrowing of the arteries are not felt;
- IIa – pain and intermittent claudication occur after covering more than 200 m;
- IIb – pain and lameness occur when covering less than 200 m;
- III – pain and intermittent claudication occur at rest;
- IV – due to ischemia, ulcers and wounds occur due to tissue necrosis.
The progression of PAD is indicated by the following manifestations:
- increased pain syndrome;
- sensory disturbances and coldness of the limb;
- dry skin and the appearance of cracks prone to infection;
- the occurrence of ulcers and wounds on the feet, legs or toes.
When PAD is complicated, it leads to the development of gangrene and the need for urgent surgery to amputate the limb.
Peripheral circulatory disorders
6
Disorders
of peripheral circulation
Blood circulation is distinguished :
1. central (systemic, in the great vessels),
2. peripheral (in small vessels and microvasculature).
Types of
peripheral circulatory disorders :
1. arterial and venous hyperemia
2. ischemia
3. stasis
4. thrombosis
5. embolism
6. hemorrhage.
Based on
anatomical and functional capabilities there are 3 types circulatory collaterals :
- functionally - absolutely
insufficient
collaterals - the sum of the lumen of the anastomoses is much less than the diameter of the afferent artery, when blockage occurs, an ischemic (white) infarction occurs (occurs in the heart, spleen, kidneys, terminal arteries are often found here); - functionally - absolutely
sufficient
- the amount of the lumen of the anastomoses is equal to (or exceeds) the diameter of the afferent artery; when a vessel is blocked, blood is delivered through another vessel; - intermediate type (typical of the lungs) - functionally
relatively insufficient
collateral - the sum of the lumens of the anastomoses is less than the diameter of the afferent artery, but blood also flows through fairly large branches, although they are thin and tortuous. When blockage occurs in this case, a hemorrhagic infarction often develops due to the abundance of blood and hypoxia.
Hyperemia
- excessive filling of tissue with blood.
Arterial hyperemia is increased blood flow to an organ through the arteries.
Microscopic changes:
- expansion of capillaries, increase in functioning vessels;
- increased blood pressure in arteries and arterioles;
- acceleration of blood flow through the vessels;
- The supply of oxygen to tissues increases, metabolism increases.
Macroscopic signs:
- an increase in organ volume due to blood supply, there may be a slight increase in heat production;
- metabolism increases, blood flow in the skin accelerates (increased skin temperature);
- redness (because there is a lot of oxidized hemoglobin);
- the arteriovenous difference in O2 decreases.
Classification of arterial
hyperemia :
1) physiological (physical activity, emotions, food intake):
a) working - this is an increase in blood flow in an organ with an increase in its function (for example, hyperemia of the pancreas during digestion);
b) reactive - this is an increase in blood flow after its short-term restriction (develops in the kidneys, brain, skin, intestines, muscles).
2) pathological (action of pathological stimuli).
According to
the mechanism of action of stimuli, pathological arterial hyperemia is divided into the following types :
- neurotonic (increased tone of parasympathetic fibers or sympathetic vasodilator => vasodilation, reverse impulse current => formation of prostaglandins => vasodilation);
- neuroparalytic (when nerves are blocked or cut => vasodilation; bradykinin and other substances have a vasodilating effect);
- myogenic (production of certain substances and their effect on smooth vascular myocytes => vasodilation). It is caused by difficulty in the flow of calcium into the cell due to the effect of lack of oxygen, hypercapnia, accumulation of lactate, ADP, adenosine, potassium, bradykinin, serotonin, histamine, GABA, prostaglandins, and increased blood pH. It happens with burns, injuries, exposure to ultraviolet and ionizing radiation, etc.
Causes of
arterial hyperemia :
- the effect of environmental factors (biological, chemical, physical);
- increased load on the organ;
- psychogenic effects.
Pathological
arterial hyperemia ( PAH ).
Occurs under the influence of a pathological irritant (chemicals, products of metabolic disorders due to inflammation, burns, fever, under the influence of mechanical factors.
There is increased sensitivity of blood vessels to irritants due to allergies.
Appears in diseases (rash, redness due to nerve damage, etc.).
Depending on the PAG factor, it happens:
1. inflammatory;
2. thermal
3. ultraviolet erythema, etc.
Prostaglandin I2 (prostacyclin) is released in the muscular wall of blood vessels, relaxing the arteries and having a powerful anti-aggregation effect on platelets.
The meaning of
pathological arterial hyperemia :
Good: 1. Removal of toxins,
2. Increased oxygen delivery to tissues,
3. This is the mechanism of action of diathermy, quartz, solux, galvanization, compresses, heating pads;
Bad: there may be rupture of sclerotic vessels with hemorrhages.
Venous
hyperemia ( VH )
is a violation of the outflow of blood from an organ through the veins. Causes: blockage (thrombus, embolus); pressure (tumor, edema, pregnant uterus, ligature).
Contributing factors: low elasticity of veins (constitution).
VH is distinguished by etiology :
1. obstructive
2. from compression
Microscopic
signs :
1. expansion of venules and veins, and later arterioles, drop in blood pressure, mainly increase in pressure;
2. the number of functioning vessels increases due to the opening of previously closed vessels;
3. blood flow speed decreases, linear and volumetric blood flow speed decreases;
4. jerky and pendulum-like movement of blood;
5. decreased metabolism, accumulation of under-oxidized metabolic products;
6. temperature drop due to a decrease in heat production and an increase in heat transfer;
7. arteriovenous difference in O2 increases sharply, hypoxia, increase
capillary permeability.
Macroscopic
signs :
1. enlargement of the organ due to dilation of blood vessels, an increase in their number, due to tissue swelling due to increased capillary permeability;
2. bluish color of the organ (a lot of reduced Hb, which has a dark cherry color);
3. ischemia (may be phlebosclerosis due to thickening of the venous wall, varicose veins) => stimulation of connective tissue growth => hardening of the organ, but sometimes this is useful for cavernous tuberculosis and trophic ulcers.
Venous
hyperemia develops with :
1. weakening of the function of the right ventricle;
2. reducing the suction effect of the chest (exudative pleurisy, hemothorax);
3. obstruction of the duct in the pulmonary circulation (pneumosclerosis, pulmonary emphysema);
4. weakening of left ventricular function.
VG value :
Good: increased rate of scar formation,
Bad: 1. Atrophy and dystrophy (due to inhibition of metabolism),
2. Sclerosis and fibrosis of the organ with dysfunction.
Ischemia
- a violation of peripheral circulation, which is based on the restriction or complete cessation of arterial blood flow to the organ.
Etiology
:
1. blockage (embolism, thrombosis, sclerosis) of the artery,
2. obturation,
3. vasospasm.
Accordingly ,
according to the etiology ischemia is :
1. compression
2. obstructive
3. angiospastic
Causes:
1. compression – compression of the artery by a ligature, scar, tumor, foreign body, etc.
2. obstructive – thrombosis, embolism (atherosclerosis, obliterating endarteritis, periarteritis nodosa)
3. angiospastic – emotions (fear, anger), physical and chemical factors (cold, trauma, mechanical irritation, chemicals, bacterial toxins).
The differences between a physiological spasm and a pathological one are the persistence and duration of the latter.
Microscopic
changes during ischemia :
1. narrowing of arterioles,
2. reduction in the number of functioning vessels (collapse of many vessels),
3. slowing down of blood flow with a more pronounced slowdown in volumetric velocity than linear,
4. lowering blood pressure,
5. tissue hypoxia,
6. arteriovenous difference in O2 increases slightly
7. decreased metabolic rate
8. accumulation of under-oxidized metabolic products => acidosis. Macroscopic
changes during ischemia :
1. pallor of tissues (low blood flow),
2. reduction in organ volume, decrease in tissue turgor,
3. decrease in organ temperature,
4. painful sensations (paresthesia - tingling, goose bumps; pain up to painful shock).
Stages
of ischemia :
- stage of decreased metabolic rate;
- stage of dystrophic changes: decreased synthesis of enzymes, NK, structural proteins => changes in organelles (swelling of mitochondria, disruption of the structure of crypts, then their reduction and destruction, death of the nucleus), cell death ^> necrosis (infarction);
- stage of sclerosis: synthesis of connective tissue => scarring (synthesis of collagen, acidic and neutral glycosaminoglycans) => sclerosis.
Angiospastic (neurospastic) ischemia: mechanism: spasm of the renal artery in one kidney leads to a reflex spasm in the other, spasm of other arteries (maybe the conditioned reflex nature of the spasm), reasons: fear, stress, predominance of the tone of the sympathetic nervous system, maybe direct irritation of the vasomotor center by toxins, tumors, cerebral hemorrhages, with increased intracranial pressure, inflammation in the diencephalon.
Outcome
with ischemia :
1. dystrophy
2. atrophy
3. necrosis
Factors that
determine the outcome of ischemia :
1. diameter of the damaged artery;
2. Duration of spasm, compression, thrombosis, embolism;
3. the rate of development of ischemia and the degree of obliteration of the artery (if the vessel is abruptly ligated, there will be a reflex spasm of other arteries);
4. tissue sensitivity to hypoxia (the most sensitive neurons, then the myocardium);
5. initial state of the organ (hyperfunction worsens the consequences of ischemia);
6. the nature of the development of collateral circulation.
Thrombosis
– intravital formation of blood clots on the inner surface of the vessel wall. Types of blood clots:
1. a) wall
b) clogging
2. a) red
b) white
c) mixed
Stages
of thrombus formation ( phases ):
1. cellular (when it predominates, the thrombus is white)
a) formation of active thrombokinase
b) prothrombin => thrombin
c) fibrinogen => fibrin
2. plasma (if it predominates, the blood clot is red) – fastening of fibrin threads with a stabilizing factor and getting stuck in the fibrin threads of blood cells
Mechanism:
- damage to the vascular wall (trauma, the action of chemicals: NaCl, FeCl3, HgCl2, AgNO3, microbial endothelins), trophic disturbances, atherosclerosis - damage without injury;
- violation of the coagulation and anticoagulant system - an increase in thromboplastin or a decrease in heparin, maybe. thrombocytosis;
- disturbance of blood flow - its slowdown, jerky, pendulum-like flow - with atrial fibrillation.
With a significant slowdown in blood flow, there are more conditions for erythrocytes to get stuck and coagulation and the blood clot will be red, but with fast flow there are no conditions for erythrocytes to get stuck, blood clotting factors are carried away, red blood cells are washed out and the blood clot will be white. That. Red blood clots often form in veins, and white ones in arteries. Red blood clot forms faster
Outcome
of thrombosis :
- aseptic melting (enzymatic, authentic) – typical for small blood clots;
- organization of a blood clot - germination by connective tissue;
- recanalization – germination of connective tissue with the formation of a canal;
- purulent septic melting of a blood clot by microbes;
- rupture and embolism (until the thrombus has sprouted with connective tissue);
- deposition of calcium salts in the veins – petrification with deformation (formation of phleboliths).
Strict bed rest for phlebothrombosis is necessary for about 3 weeks to organize a blood clot so that it does not break off and lead to ischemia and necrosis.
Factors that
determine the severity of the consequences ( consequences - ischemia , necrosis ):
1. diameter of the vessel (the larger the diameter, the worse);
2. type of vessel (artery – necrosis, vein – venous hyperemia, edema);
3. the nature of the thrombus (parietal - less dangerous, clogging - more dangerous);
4. rate of thrombus formation;
5. sensitivity of organs and tissues to hypoxia;
6. the possibility of a reflex disturbance of blood flow in nearby vessels;
7. degree of severity of collateral circulation.
Embolism
– blockage of blood vessels by bodies (emboli) brought by blood or lymph flow. Types of emboli:
1. endogenous (blood clots, pieces of tissue from injuries, tumor metastases, in case of fractures of tubular bones, yellow bone marrow enters the non-collapsing vessels of the bones with the development of fat embolism, amniotic fluid embolism)
2. exogenous
a) air – it enters large veins
- air embolism - when large veins are damaged (subclavian, jugular, chest veins - due to negative pressure, neck veins - because they are fused to the fascia and do not collapse)
- gas embolism – decompression sickness
b) bacterial embolism (squeezing a boil on the face => veins of the face communicate with the veins of the brain => brain abscess)
c) foreign bodies
d) parasites
Types
of embolism by location :
1. small circle
2. large circle
3. Gate system
Sources of large circle emboli are the lungs, the left half of the heart, and large arteries.
The sources of emboli in the small circle are the veins of the systemic circle and the right heart.
The sources of portal system emboli are the vessels of the unpaired abdominal organs.
Retrograde embolism occurs when a thrombus moves against the blood flow due to the weak suction effect of the chest.
Paradoxical embolism occurs with defects of the septum of the heart (a thrombus from the right heart goes to the left).
Pulmonary embolism :
Pathogenesis :
1. drop in blood pressure, multiple small embolism is more dangerous; a drop in systemic pressure due to the fact that there is a reflex decrease in arterial tone;
2 myocardial hypoxia;
3. increased pressure in the pulmonary artery due to spasm of the arteries of the pulmonary artery system (a protective reaction that prevents pulmonary edema);
4. acute cor pulmonale (overload of the right parts) => decreased contractility => fibrillation => death;
Clinic – severe shortness of breath, collapse, cyanosis, drop in blood pressure, swelling of the neck veins.
Portal vein embolism :
When the portal vein is blocked, up to 90% of the blood accumulates in the veins of the portal system, because Normally, portocaval anastomoses do not function, and portal hypertension does not occur. If there is thrombosis of a branch of the portal vein (splenic, superior and inferior mesenteric veins), then there will be portal hypertension. If there is a blockage of the portal vein itself, then death occurs within 15 minutes. - 2 hours due to cerebral ischemia. With gradual obstruction, portal hypertension develops (ascites, dilatation of the superficial veins of the anterior abdominal wall, enlargement of the spleen, drop in blood pressure, decrease in blood volume due to accumulation of blood in the gastrointestinal tract, shortness of breath, then decreased breathing, apnea, loss of consciousness, respiratory paralysis).
Factors that
determine the severity of the consequences of embolism ( consequences - ischemia , necrosis ):
1. diameter of the vessel (the larger the diameter, the worse);
2. type of vascular system;
3. duration of embolism;
4. the nature of the embolus (the bubble dissolves, microbes cause an abscess, the tumor causes metastases);
5. multiplicity of vascular damage;
6. sensitivity of organs and tissues to hypoxia;
7. the possibility of a reflex disturbance of blood flow in nearby vessels;
8. degree of severity of collateral circulation.
Stasis
– slowing down and stopping blood flow in capillaries, small arteries and veins.
Types
of stasis :
- ischemic – a consequence of cessation of blood flow, reversible;
- venous – a consequence of venous hyperemia (compression of veins, thrombosis, embolism), reversible;
- true (capillary) – a consequence of pathological changes (damage by toxins, chemicals, temperature, radiation, mustard, castor oil) in the capillaries or a drop in blood rheology, irreversible.
Mechanism:
In true stasis, red blood cells stick together => obstructed blood flow => increased peripheral resistance, increased capillary permeability, slowed blood flow due to blood thickening, release of Hb from red blood cells. BAS (serotonin, bradykinin, histamine) and acidosis are also important in the mechanism. The release of plasma albumin into tissue causes a decrease in the charge of erythrocytes. The adhesion of red blood cells is also explained by the fact that
that their surface becomes rough, their sorption properties decrease.
Microcirculation
– orderly movement of blood and lymph through microvessels, transcapillary metabolism, as well as the movement of fluids in the extravascular space.
The microvasculature includes: arterioles, precapillaries, capillaries, postcapillaries, venules, arteriovenular shunts, lymphatic capillaries.
Microcirculation disorders:
- intravascular: aggregates (sludge syndrome) - a violation of the suspension state of the blood (the more globulins and fibrinogen that have a “+” charge (in erythrocytes there is a “-“ charge), the stronger the sludge syndrome), a violation of blood viscosity.
- extravascular
- transmural
Aneurysms
Aneurysms of peripheral arteries are characterized by the appearance of pathologically dilated areas of the arterial wall, resulting from its weakening. As a result, the artery wall bulges and this condition can be complicated by thromboembolism, strokes, or, if the arterial wall is significantly thinned, ruptures.
About 70% of such aneurysms occur in the popliteal arteries, and 20% in the iliofemoral segment. Sometimes they are combined with abdominal aortic aneurysms, which in 50% of cases are bilateral. Typically, aneurysms of peripheral arteries are provoked by atherosclerosis and infectious diseases (in such cases, the protrusion is most often localized in the femoral artery). Sometimes the root cause of their occurrence is entrapment of the popliteal artery or septic emboli, leading to the formation of a mycotic aneurysm.
Peripheral aneurysms are often asymptomatic. In some cases they are manifested by the following symptoms:
- pain when palpating;
- pallor and coldness of the affected limb;
- sensitivity disorders;
- absence of pulse in the affected area due to thromboembolism or rupture of a pathological protrusion;
- pain, fever, general malaise (if the aneurysms are infectious).
The risk of artery rupture in the area of the aneurysm is low - no more than 5% for popliteal bulges and 1 - 14% for iliofemoral aneurysms.
Pathogenesis and mechanism of development of pathology
The pathogenesis of venous hyperemia is due to the following factors:
- low arteriovenous pressure;
- venous blockage (thrombosis or embolism);
- decreased elasticity of venous walls;
- difficult movement of venous blood due to its thickening and increased viscosity;
- compression of veins by edema, tumor, etc.;
- impaired cardiac performance;
- decreased suction function of the chest due to accumulated blood or air in the pleural plane.
So, let us repeat that the mechanism of development of venous hyperemia is:
- compression of veins by external factors - tumor, scars, uterus during pregnancy, surgical ligation of blood vessels;
- compression of veins by edematous fluids;
- venous blockage by a thrombus.
Prolonged venous hyperemia can cause complete atrophy of the organ.
- Venous encephalopathy: causes, symptoms, diagnosis, treatment and consequences
Phlebeurysm
Varicose veins are a pathological expansion of the lumen of superficial venous vessels, accompanied by incompetence of the venous valves and leading to impaired blood flow. It is usually not possible to determine the underlying cause of vascular damage. Such a disorder is usually caused by primary valvular insufficiency and reflux, primary dilatation of the venous walls due to weakness of vascular tissues, chronic venous hypertension or insufficiency.
Varicose veins are more often detected in women. It often occurs during pregnancy or difficult childbirth. There are usually no risk factors for its development, but sometimes its occurrence is explained by hereditary predisposition. As a rule, it is the veins of the lower extremities that are affected.
Symptoms of varicose veins are not always visually noticeable. At the beginning, the veins may be tense and palpable. As the disease progresses, they enlarge, protrude above the surface of the skin and become visible. The patient complains of leg pain, discomfort, fatigue, tension and pressure. Particularly pathological dilated vessels are noticeable in a standing position.
When a vein thromboses, the patient experiences severe pain, and the superficial veins can form venous bullae, which rupture and bleed at the slightest physical impact. Sometimes such bleeding goes unnoticed (for example, during sleep), and leads to death.
Ulcers and other dermatological disorders with varicose veins rarely occur. They can manifest as eczema or pigmentation that appears in the ankle area. Ulcerative lesions usually occur after injury and are small in size and superficial.
What types of disease?
The following types of venous hyperemia are distinguished:
- Natural - does not cause consequences. Occurs with prolonged exposure to heat, significant emotional stress, changes in hormonal levels in women and physical overload.
- Pathological - develops against the background of exposure to negative factors (the influence of medications, cosmetics, edema and tumors, allergies, viral infections, the influence of high and low temperatures).
The following types are also distinguished:
- Working. Improves the functioning of organs and tissues.
- Reactive. Occurs with prolonged disruption of the blood supply to soft tissues and compression of organs.
There are also:
- acute;
- chronic.
Return to contents
Diagnosis of vascular diseases of the lower extremities
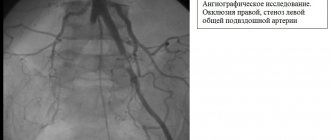
To identify obliterating diseases of the arteries of the lower extremities (LOAD) and aneurysms, the patient is referred to a vascular surgeon. After a physical examination, the patient may be prescribed the following tests:
- determination of the ankle-brachial index;
- Doppler and duplex ultrasound scanning;
- digital angiography;
- CT angiography and MRI angiography;
- blood tests for the level of lipoproteins VP, NP and SNP, SC myoglobin and C-reactive protein, the level of total cholesterol and triglycerides, sugar, atherogenicity coefficient.
To find out the root cause of the disease and prevent complications, the patient may be recommended to consult other highly specialized specialists: cardiologist, neurologist, endocrinologist, hematologist, ophthalmologist. If necessary, the examination of the patient is supplemented by ECG, Echo-CG, Dopplerography of the vessels of the head and neck, renal arteries, etc.
Varicose veins are usually detected during an objective examination and special tests. If necessary, the examination is supplemented with duplex ultrasound scanning of the leg veins.
Treatment of obliterating atherosclerosis and superficial aneurysms of peripheral vessels
Treatment of OZANK is carried out depending on the nature and severity of the manifestations of the disease. If there is a slight disturbance in the structure of blood vessels, the patient is prescribed conservative therapy and dynamic observation.
All patients are recommended to eliminate the factors that provoke the progression of the pathology:
- to give up smoking;
- weight normalization;
- treatment of arterial hypertension and control of blood pressure;
- sufficient physical activity: walking, walks, physical therapy;
- changing your diet to reduce bad cholesterol and triglycerides;
- blood sugar control;
- the use of pneumatic cuffs and stockings to eliminate stress on blood vessels.
Drug treatment is aimed at reducing thrombus formation, normalizing blood flow and treating pathologies that increase the risk of stroke and myocardial infarction. For this purpose, the patient is prescribed antiplatelet agents (Aspirin, Cardiomagnyl, etc.), Pentoxifylline, ACE inhibitors, blood thinners (for example, Clopidogrel, Cilostazol, etc.).
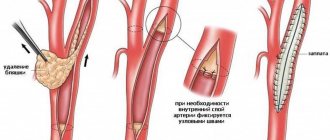
If it is impossible to restore normal blood flow, patients with stage II-III OZANK can undergo the following types of surgical operations:
- thromboendarterectomy - performed to eliminate short localized lesions of the aorta, common or deep femoral, iliac arteries;
- artery bypass - an additional vessel (shunt) is created to bypass the blocked artery to normalize blood supply;
- artery replacement – the affected area of the artery is replaced with an artificial vascular prosthesis;
- endovascular operations (balloon angioplasty and artery stenting) - the lumen of the artery is expanded using a special balloon, which is inserted into the lumen of the artery and inflated; if necessary, a cylindrical wire structure (stent) can be installed at the site of narrowing, restoring normal blood flow.
The choice of surgical treatment method is determined by the clinical manifestations of the pathology. Endovascular interventions are less invasive and therefore doctors try to give preference to their implementation.
If surgical techniques turn out to be ineffective and the patient still develops gangrene, then to save his life, operations to amputate the limb (full or partial) are performed.
Also, for the treatment of patients with chronic ischemia of the lower extremities, angiogenesis stimulators (from autologous CD133+ endothelial progenitor cells) and Angiostimulin (a gene preparation of the vascular endothelial growth factor VEGF165) can be used.
Surgical removal of peripheral aneurysms of the vessels of the legs is indicated when the artery is dilated more than 2 times, and for protrusions in the arteries of the arms, operations are performed in all cases. To eliminate them, the affected area of the arterial vessel is excised and replaced with a graft. Sometimes an endovascular stent graft is used to repair aneurysms - a woven polyester tube covered with a metal frame is installed into the aneurysm without open surgery. This technique is used for patients who cannot undergo other types of surgery. Its purpose is to strengthen the vessel wall and prevent its rupture.
Treatment of varicose veins
To eliminate varicose veins, both conservative and surgical techniques are used. The patient is recommended to wear compression products (stockings, tights or knee socks) and periodically take medications to strengthen the walls of venous vessels (Troxevasin, Detralex, Cyclo 3 Fort, etc.). For local application, agents such as Lyoton, Curiosin, Venoruton, Heparin ointment, etc. are used. To normalize the condition of veins and blood flow, physiotherapy can be prescribed: amplipulse therapy, local darsonvalization, intermittent pneumocompression, magnetic therapy, hyperbaric oxygenation, laser therapy, balneo- and hydrotherapy.
As a minimally invasive technique for minor manifestations of varicose veins, sclerotherapy can be performed - the introduction of a sclerosant drug (for example, Fibro-Vein, Athoxysclerol, Sodium tetradecyl sulfate, Sclerowein, etc.) into the dilated areas of the veins, causing “gluing” of the pathologically dilated vessel. Other minimally invasive techniques can be used to remove varicose veins - ablation using laser or radiofrequency ablation. These procedures seem to seal the dilated vessels. In other cases, traditional surgical interventions are performed to remove veins, consisting of ligation or removal of the large and sometimes small saphenous veins. They are performed using different methods (stripping, miniphlebectomy, crossectomy) and can be supplemented with minimally invasive methods. The patient may also be prescribed some endoscopic types of interventions: endoscopic dissection and transluminal phlebectomy.