Diseases of the aorta and peripheral arteries
What are diseases of the aorta and peripheral arteries?
First of all, let's take a quick look at the anatomy.
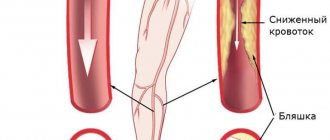
The aorta, the main artery of our body, is divided approximately at the level of the navel into branches - the common iliac arteries, which in turn are divided into external and internal iliac arteries. At approximately the level of the inguinal fold, the external iliac arteries become the femoral arteries. The continuation of the femoral arteries are the popliteal artery and the arteries of the leg. Many smaller branches arising from these arteries carry blood and nourish the entire leg. When the patency of the arteries is impaired, the tissues do not receive enough blood, and with it, oxygen and nutrients. Which leads to the occurrence of peripheral arterial diseases. The cause of arterial obstruction in the vast majority of cases is atherosclerosis. The inner surface of the arteries is normally smooth, but with age, so-called atherosclerotic plaques form in the artery walls - accumulations of cholesterol that narrow the lumen of the vessel. As a result, the tissues of the lower extremities do not receive blood and oxygen in adequate quantities. This lack of blood flow is called ischemia. The latter circumstance can cause discomfort or pain when walking. The pain can be localized in the buttocks, thighs, knees, legs, and feet.
In advanced cases, trophic ulcers or gangrene may develop, leading to loss of a limb. The insidiousness of atherosclerosis is that it certainly progresses and is systemic in nature, that is, it can simultaneously affect not only the arteries of the lower extremities, but also the arteries of the heart, the carotid arteries, which can lead to the development of heart attack and stroke. However, these events can be avoided if you consult a doctor in time and stop the progression of the disease. We must also remember that in approximately half of the cases the disease may not manifest itself in any way for a long time.
What are the signs of the disease?
In the early stages, the disease may not manifest itself in any way. Later, pain, cramps, or fatigue in the legs may appear when walking. Pain when walking usually occurs in the buttocks, thighs, and feet. This is the most characteristic symptom of damage to the arteries of the lower extremities, which is called intermittent claudication. It appears when you walk (when the need for oxygen increases) and goes away when you stop. Intermittent claudication occurs more quickly when climbing stairs. As the disease progresses, you may notice that over time the pain begins when walking shorter distances. Finally, in later stages, pain may occur at rest.
Without treatment, the disease progresses steadily. Signs of this are:
- Increased pain, coldness and loss of sensitivity in the limb
- Dryness, cracks on the skin of the limb. Large cracks can become infected if left untreated.
- Sores and sores on your toes, heels, or shins
- Gangrene (tissue death), which may require amputation
If there is pain at rest, trophic ulcers or gangrene, then, due to the severity of the condition and the seriousness of the consequences, such lesions are usually combined under the term critical ischemia. The presence of critical ischemia means that the legs do not receive enough blood even when you are resting.
What causes the disease?
As already mentioned, the cause of the disease in the vast majority of cases is atherosclerosis. The development and progression of the disease is facilitated by risk factors, the most significant of which are the following:
- Smoking,
- Diabetes,
- High blood cholesterol levels
- High blood pressure,
- High level of homocysteine in the blood,
- Excess body weight
- Increased blood viscosity,
- Presence of cases of cardiovascular diseases in the family.
Obliterating endarteritis (thrombangoitis, Buerger's disease)
With this disease, the arteries of the lower extremities are also affected, but of a smaller diameter, mainly the arteries of the lower leg. The cause of the disease has not been established, but there is a clear connection with smoking. It is known that without quitting smoking, circulatory decompensation quickly occurs in this disease, which often leads to the need to amputate a limb. In rare cases, the cause of damage to the aorta and arteries of the lower extremities is nonspecific aortoarteritis or the so-called Takayasu disease, which usually occurs in young women under 30 years of age.
What kind of examination are you undergoing?
First, the doctor conducts a survey and examination, including a detailed review of your complaints, history of the underlying disease, and family medical history. The condition of organs and systems and some other procedures are assessed. Particular attention is paid to assessing the pulse at all points accessible to palpation. If after this your doctor suspects damage to the arteries, you will be asked to undergo a series of special tests to clarify the diagnosis and determine the severity of the damage.
Ankle-brachial index (ABI)
This is a non-invasive and fairly simple method. To determine ABI, blood pressure is measured in the ankles and arms using a regular blood pressure cuff and an ultrasound probe and compared. Normally they should be approximately equal. Decreased pressure in the ankles indicates damage to the arteries of the aortoiliac region and/or arteries of the lower extremities.
Dopplerography and duplex scanning
Doppler ultrasound is another non-invasive method that, using high-frequency sound waves, makes it possible to determine the type and speed of blood flow. Duplex scanning combines Doppler ultrasound and conventional ultrasound. Using this method, you can see how and at what speed blood flows through the vessels, determine the diameter of the vessel and the degree of narrowing, as well as the structure of the atherosclerotic plaque.
Angiography
Contrast arteriography is a more invasive method, but provides an accurate diagnosis. After puncture of the artery, under the control of an x-ray image, a contrast agent is injected into the lumen of the artery and the arteries are visualized. Using this method, the exact location and degree of narrowing of the arteries is found. The contrast agent is removed from the body through the kidneys. In some cases, angioplasty and stenting of a narrowed vessel can be performed simultaneously.
Accurate diagnosis can also be made using computer and magnetic resonance imaging (CT and MR) methods.
Treatment
Lifestyle change
Undoubtedly, a very important stage of treatment is lifestyle changes. In this regard, your doctor may recommend the following:
- quit smoking if you are a smoker;
- optimize weight, diet and exercise regimen;
- Constantly monitor and adjust your blood pressure levels if you have high blood pressure;
- Manage your blood sugar levels with appropriate diet and treatment if you have diabetes.
Drug treatment
Depending on the situation, the doctor may prescribe treatment aimed at reducing pain, blood viscosity, normalizing cholesterol, blood pressure and glucose levels.
Surgery
The choice of surgical treatment method depends on many factors: location, severity of the lesion, age.
Artery bypass : bypassing a narrowed or completely blocked section of an artery, an additional path is created for blood flow - a shunt. One of your own veins or a prosthesis made of artificial material can be used as a shunt. Examples of such operations include the so-called aortofemoral, aortoiliac, iliofemoral, femorofemoral, femoropopliteal, femoro-tibial bypass.
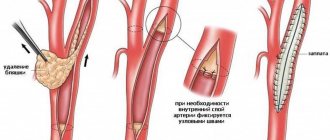
Artery replacement : the affected area of the artery is replaced with an artificial vascular graft. Endarterectomy and arteryplasty: an operation in which atherosclerotic plaque is removed through an incision in the artery to restore blood flow. For a better result, a special patch can be sewn between the edges of the arterial incision, thereby expanding the lumen of the artery.
Operations used for atherosclerosis of the lower extremities
Endovascular methods
Along with traditional operations for diseases of the aorta and peripheral arteries, newer treatment methods can be used. These include balloon angioplasty with or without arterial stenting. The balloon angioplasty method involves inserting a long narrow tube called a catheter into its lumen through a small puncture of the artery in the thigh. The catheter is passed to the site of narrowing of the vessel. After this, the balloon located at the end of the catheter is inflated, the lumen of the artery expands and patency is restored.
To improve the results, after angioplasty, a special metal device, a stent, is installed in the lumen of the vessel. The stent expands the lumen of the artery and serves as a scaffold that maintains normal patency of the vessel.
These techniques are significantly less invasive compared to surgery, that is, they are easier for the patient, require less recovery time, and are associated with a lower risk of serious complications. However, endovascular methods cannot be used in all patients.
In the last 30 years, the goal of many studies has been to study the possibility of normalizing blood circulation in the lower extremities by stimulating angiogenesis, the process of developing a capillary network from existing vessels.
In the department of surgical treatment of arterial pathology of the Scientific Center for Cardiovascular Surgery named after. A. N. Bakuleva RAMS is treating chronic ischemia of the lower extremities with the help of angiogenesis stimulators (autologous CD 133+ endothelial progenitor cells in the 1st group of patients and “Angiostimulin” - a gene preparation of the vascular endothelial growth factor VEGF165 - in the 2nd group).
The A. N. Bakulev Scientific Center for Cardiovascular Surgery of the Russian Academy of Medical Sciences, together with the Institute of Gene Biology of the Russian Academy of Sciences, developed and obtained the gene preparation “Angiostimulin”; based on a plasmid construct containing the human VEGF165 gene. Autologous mesenchymal pluripotent endothelial blast precursor cells expressing the CD 133+ antigen on the surface are isolated from bone marrow punctate by magnetic separation using magnetic antibodies CD 133+, CD 34+, CD 45- (Miltenyi Biotec).
Successful preclinical studies and promising results from clinical trials have created strong hopes that angiogenesis will become another promising area in the treatment of chronic lower extremity ischemia, either alone or in combination with other techniques.
Department of Vascular Surgery and Arterial Pathology of the Scientific Center for Cardiovascular Surgery named after. A. N. Bakuleva RAMS has all the modern methods of treating this pathology. The choice of the optimal intervention for each patient, an individual approach, as well as the patient’s desire to recover and lead a healthy lifestyle are the keys to the success of treatment of peripheral arterial diseases.
1. Occlusive-stenotic lesions of blood vessels
Occlusive-stenotic vascular lesions
is a group of diseases characterized by impaired patency of the main arteries.
The etymology of vasoconstriction is different, and the location is found in different basins of the circulatory system. The result of such changes is a disruption of the blood supply to certain parts of the body or organs and, as a result, their functional failure.
A must read! Help with treatment and hospitalization!