Electrophysiological study of the heart - EPS
Contraindications
This type of research is strictly prohibited under the following circumstances:
- acute infectious disease or simply the presence of fever;
- heart attack or stroke in the acute stage;
- severe angina that occurs for the first time and progresses;
- in acute surgical pathology;
- in severe chronic heart failure or in its acute form;
- the presence of certain types of heart defects;
- if there is a suspicion of pulmonary embolism;
- diseases of the esophagus;
- the presence of cardiac or aortic aneurysms.
Proper preparation for the procedure
To undergo this procedure, the patient is referred after a complete examination by a cardiologist, arrhythmologist or cardiac surgeon. Before performing EPI, the attending physician conducts the following studies:
The patient will first of all have to carry tests for HIV, hepatitis, syphilis and blood clotting. These tests are necessary, since diagnosis using the electrophysiological study method will take place in a hospital, and the patient will have to be hospitalized.
- MRI or CT, these examinations are especially necessary if the patient experiences fainting, the doctor excludes the presence of brain pathologies;
- Ultrasound of the heart;
- 24-hour Holter monitoring;
- discharge summary with justification for the need for this procedure.
In addition, the patient himself must prepare for the upcoming examination. To do this he will need:
- fast for 8 – 10 hours;
- within a few days, stop drinking caffeine, alcohol and cigarettes;
- The doctor will stop the use of any medications.
Progress of the procedure
Considering that there are two types of research - invasive and non-invasive, there will be two ways to carry out the procedure.
Methodology for non-invasive EPI
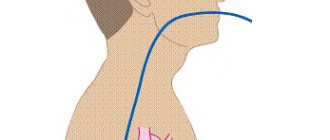
The most commonly used non-invasive examination method, in which a catheter with an electrode is inserted through the nose or mouth, which is used somewhat less frequently. This method is also called transesophageal EPI or TEE. It is carried out in functional diagnostic departments, usually in the morning. The examination takes place as follows:
- Preliminary blood pressure measurement.
- Taking an ECG.
- The doctor explains the procedures and specifies what the patient will experience during the examination. There is usually a burning sensation in the chest, and this is normal.
- All manipulations usually take about half an hour.
- Through the nasal opening or, in rare cases, through the mouth, the doctor inserts a probe with an electrode into the patient, which is connected to special devices. Using equipment, stimulation of the heart muscle is carried out with electrical impulses. During this procedure, the heart begins to contract vigorously, as if under increased stress. All received data is recorded.
- An electrogram is recorded.
- The doctor carefully removes the catheter.
- A complete analysis of the collected information is carried out and a conclusion is made, which is sent to the attending physician.
- The tachycardia caused by the procedure will go away after some time, but if the discomfort continues for a long time, the doctor can provide medication.
Method of performing invasive EPI
In cases where TEE does not produce results or for some reason it is contraindicated, the doctor will prescribe endocardial or epicardial EPI.
Endocardial EPI
Before the procedure, the patient is placed in the department of cardiology, cardiac surgery or cardiac arrhythmology. EndoEPI itself is done in the department of X-ray surgical diagnostic methods. The patient is given an antisedative and taken to the operating room. Local anesthesia is performed. In complete sterility, the doctor makes an incision to insert a catheter into the femoral or subclavian vein. An introducer (metal or plastic guide) is inserted into the incision. A probe with an electrode is passed through it. The passage of the probe is observed on the screen. This is possible due to the available contrast agent. The probe is passed to the atrium or ventricle. The doctor performs electrical stimulation. All data is recorded using a computer.
This entire medical procedure lasts approximately half an hour. The patient should feel absolutely no discomfort. After removing the probe, apply a tight bandage to the insertion site.
Epicardial EPI
This study is carried out in the cardiac surgery department. The entire operation is performed under general anesthesia. The doctor dissects the chest and gains access to the pericardial cavity. Using electrodes, the doctor stimulates the epicardium. All data is recorded and then the wound is sutured. Typically, the operation lasts about an hour and is the most difficult area of examination using the EPI method.
Radiofrequency ablation of the heart
The invention and active introduction into widespread practice of minimally invasive interventions with maximum effect is the main path of development of modern medicine. Radiofrequency catheter ablation refers to precisely such operations.
RFA is a technique for treating cardiac arrhythmias by physically destroying the focus of pathological excitation or areas of abnormal impulse conduction.
This operation made it possible to abandon complex open-heart surgery in the treatment of many types of arrhythmias, including those resistant to drug therapy.
Indications for surgery
Radiofrequency catheter ablation of the heart is the option of choice in the treatment of arrhythmias in young patients, as it allows in a relatively short time not only to improve the patient’s well-being and quality of life, but also to reduce the risks of sudden cardiac death and disability.
Pathologies for which doctors strongly recommend RFA of the heart:
- Atrial fibrillation with ventricular tachysystole.
- Paroxysmal atrial tachycardia.
- Wolff-Parkinson-White syndrome.
- Paroxysmal ventricular tachycardia.
- Arrhythmic disorders associated with cardiomyopathies.
- The presence of additional pathways, subject to a family history of sudden death.
- Intolerance or serious side effects when taking traditional antiarrhythmics.
- Tachyarrhythmias resistant to drug therapy.
If absolutely necessary, RFA can be performed even on children without congenital heart defects, starting from an early age. In this case, the indications for RFA surgery will be the development of tachycardia-dependent cardiopathy with a decrease in the pumping function of the heart and the lack of the desired effect after the use of all groups of antiarrhythmic drugs.
It is worth noting that for a number of arrhythmic disorders, radiofrequency ablation of the heart is recommended even if the patient does not want to take antiarrhythmic drugs for life or does not tolerate them well.
8
24/7
Purpose of the operation
The goals pursued when performing RFA of the heart are always aimed at eliminating the cause of arrhythmogenesis - a pathological conduction pathway or an abnormally active area of the myocardium. To do this, during cardiac ablation, a targeted destruction of a malfunctioning section of the cardiac conduction system is performed, which can have two different effects, each of which is optimal for its own group of heart pathologies. Thus, in the treatment of atrial tachycardia with anomalies of AV conduction, the method of choice is complete or partial radiofrequency ablation of the atrioventricular junction. At the same time, in the case of ventricular tachycardia or the presence of bypass paths, RFA will be aimed at destroying the most pathological area of the heart.
Radiofrequency catheter ablation of the heart allows you to avoid a number of negative consequences of living with arrhythmia, such as:
- high risk of early and sudden death from arrhythmia;
- ischemic stroke;
- myocardial infarction;
- expansion of the cavities of the heart with subsequent development of heart failure;
- long-term use of a large number of medications;
- progressive decrease in working capacity;
- high risk of death for the mother during pregnancy (for some types of arrhythmias this is an indication for abortion).
Types of RFA
Since the principle of catheter ablation is to destroy a small area, all types of this procedure differ in the physical factor causing destruction:
- radiofrequency ablation;
- electroablation;
- Ultrasonic destruction;
- laser cardiac ablation;
- cryodestruction.
However, the effectiveness, controllability of destruction and implementation features for these methods are not the same. Nowadays, RFA is most often used, since it is this technique that has produced the largest number of positive results. Whereas, for example, most cardiac surgeons are moving away from ablation with direct electric current in favor of RFA of the heart and other techniques.
Preparation for surgery, necessary tests and examinations
Before the operation, when communicating with the cardiac surgeon who will perform radiofrequency ablation of the heart, it is necessary to clearly state the list of medications taken by the patient and their dosages. It is also important to provide your doctor with information about the presence of an implanted pacemaker, allergic reactions or intolerance to medications, if any.
The list of mandatory diagnostic procedures before cardiac ablation includes the following:
- General clinical blood test.
- Biochemical studies of venous blood: bilirubin and liver enzymes, glucose, creatinine and urea with GFR calculation, total protein, etc.
- Coagulogram.
- General urine analysis.
- Electrocardiography.
- Holter (24-hour) ECG monitoring.
- Echocardiographic study.
Also, in the presence of concomitant pathology, in addition to routine methods, additional tests and diagnostic procedures may be required. For example, patients with coronary artery disease may be prescribed a lipid profile, and patients with diabetes mellitus may be prescribed a study of the level of glycated hemoglobin. It is important to consider that many patients with arrhythmias receive anticoagulant therapy, so an INR study may be added to the above.
It is recommended not to take food or water the day before RFA (at least 12 hours).
Method of operation
When performing radiofrequency ablation, general anesthesia is not required, so the patient is only anesthetized at the insertion site of the catheter electrode and is also prescribed sedatives. Already in the operating room, stable venous access is provided: it will be needed for the administration of contrast agents, antiarrhythmics or other drugs that may be needed during RFA of the heart.
The main instruments of the team of electrophysiologists and cardiac surgeons are flexible catheter electrodes. They are introduced through a large vessel, preferably through the femoral artery. Other options for introducing electrodes, for example, through the subclavian vein or other vessels, are not excluded. Radiofrequency ablation is performed under fluoroscopy guidance, so the patient does not have to worry that cardiac surgeons are operating blindly.
Typically, RFA surgery is performed in two stages:
- Performing an electrophysiological study.
- Actually radiofrequency ablation.
In the case when pathology (for example, atrial fibrillation) requires destruction of the atrioventricular connection, then another stage is added - implantation of a pacemaker, since with such ablation of the heart the conduction of impulses from the tissues of the atria to the myocardium of the ventricles completely stops.
An electrophysiological study is the compilation of a kind of map of the heart, which will reflect the areas where pathological conduction or formation of electrical impulses occurs. This procedure is performed by introducing a specific contrast and electrical stimulation of areas of the heart. During this procedure, disturbances in the rhythm of the heart are usually induced, but in an operating room these arrhythmias do not pose a threat to the patient.
Upon completion of mapping, cardiac surgeons insert an ablation electrode through the same access and begin performing RFA of the heart. A catheter ablation electrode is installed in the projection of the pathological area and its destruction is carried out by the point action of radio frequency waves. If there is a large lesion or several abnormal zones in the tissues of the heart, their destruction can be performed during one operation or RFA will need to be repeated later.
After the RFA procedure, if indicated, a pacemaker can be installed and programmed.
Since the patient is conscious during cardiac ablation, this is sometimes associated with some discomfort. Therefore, if you experience any unpleasant sensations, it is advisable to inform your doctor. At the same time, you should not be afraid of this intervention, because almost all manipulations with the electrodes are painless for the patient.
The amount of time spent performing radiofrequency ablation ranges from 3 to 7 hours.
Description of the postoperative period and rehabilitation
One of the most significant advantages of RFA compared to open heart surgery is its low morbidity and rapid recovery. While a patient after a sternotomy will feel pain in the sternum, wear a special bandage for months, and limit his exercise, a patient after RFA will be able to return to his normal rhythm of life in a couple of weeks, which will no longer be burdened by arrhythmia.
8
24/7
Directly from the operating room, the patient is transferred to the intensive care unit, where he spends the first day after RFA. Here, constant monitoring of heart rate and blood pressure is carried out. To prevent bleeding from the ablation catheter insertion site, it is recommended to lie down for the first 4-5 hours after surgery.
If there are no complications, the patient will be able to leave the clinic where the cardiac ablation was performed the next day.
Possible complications with RFA
An intervention such as cardiac ablation has a very low risk of serious complications, but does not completely eliminate them. Most often, patients experience a hematoma at the site of electrode insertion, but they usually do not require any specific treatment and go away on their own within a few weeks.
Less common are more serious complications:
- perforation of the walls of blood vessels or tissues of the heart;
- pneumothorax;
- development of complete atrioventricular block.
The risk of death with this operation is usually about 0.2% or less.
RFA results
The effectiveness after RFA surgery will depend on the type of arrhythmia, the anatomical features of the patient’s heart and the presence of concomitant pathology of the internal organs in general and the heart in particular. The percentage of successful RFA ranges from 75% to 95%, for example, in the treatment of supraventricular arrhythmias it is about 96%. The incidence of complications when performing cardiac ablation is no more common than 1.5-2%.
Sometimes, after a successful first RFA operation, new abnormal areas are formed over time, which is associated with the peculiarities of the electrophysiology of the heart of a particular patient; in such clinical situations, repeated ablation may also be required.
In the vast majority of cases, patient reviews of quality of life after RFA are positive. They can engage in activities that were previously denied access due to the risk of arrhythmia. Patients can exercise, women of fertile age can safely carry and even give birth to a child on their own. A significant advantage is that for a number of pathologies after RFA of the heart it is not necessary to continue taking medications continuously.
Cost of the operation
Performing radiofrequency ablation requires high-tech equipment and the presence of qualified specialists, so it is not yet carried out everywhere. Typically, clinics with these resources are located in large cities, and there are even several of them in St. Petersburg and Moscow.
The cost of radiofrequency cardiac ablation is calculated individually for each patient and can vary significantly due to different volumes of intervention, the need for implantation of a stimulator, and the level of the clinic in which the operation is performed. The average price is from 150 thousand rubles.
It should be noted that in the Russian Federation there are quotas for free RFA of the heart.