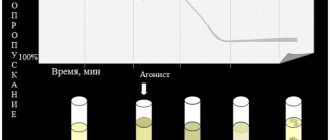
Increased aggregation is a marker of hyperaggregation syndrome and thrombophilia. The most commonly used are the Born turbidimetric method, based on recording changes in the light transmission of platelet-rich plasma, and the method for studying platelet aggregation, based on the analysis of light transmission fluctuations caused by a random change in the number of particles in the optical channel.
Material for research.
Citrate platelet rich plasma
Research method
is determined by the operating procedure on a particular type of aggregometer.
Solutions of ADP, ristocetin, collagen, adrenaline, and arachidonic acid are most often used as inducers. Solutions of thrombin, serotonin, etc. can also be used.
Platelet aggregation with ADP
Exposure to small doses of ADP (usually 1*10-7 mol) leads to the formation of a double wave of aggregation. The first phase (primary wave) depends on added exogenous ADP, and the second phase (secondary aggregation wave) occurs due to the release reaction of intrinsic agonists contained in platelet granules. Large doses of ADP (usually 1*10-5 mol) lead to the merging of the first and second waves of aggregation.
When analyzing aggregograms, attention is paid to the general nature of aggregation (single-wave, two-wave; complete, incomplete; reversible, irreversible) and the rate of aggregation. The appearance of two-wave aggregation upon stimulation of ADP at concentrations that normally cause reversible aggregation (usually 1-5 µmol) indicates an increase in platelet sensitivity, and the development of single-wave incomplete (and often reversible) aggregation upon stimulation of ADP at concentrations of 10 µmol or more indicates an increase in platelet sensitivity. impaired platelet release reaction.
PLT blood test - interpretation
How are platelets designated in a blood test
? Platelets: Platelets PL TRO PLT
Platelet units: ___x109/l (or x10^9/l) ___x109 cells/l
In addition to traditional “manual” microscopy, automated examination of blood smears determines a number of new characteristics of the general blood test and presents a graphical display of the study results - a histogram.
Parameters of the platelet part of the hemogram
PLT - platelets - this is the absolute number of platelets MPV - average platelet volume - reflects the average value (average diameter) of platelets PCT - thrombocrit - reflects the proportion of the volume of all platelets from the total blood volume PDW - width of platelet distribution by volume (degree of anisocytosis * PLT) - shows the relationship between different forms of platelets in the blood, or more precisely, which forms of platelets predominate: macroplatelet**, microplatelet*** or healthy platelets of normal size.
*anisocytosis – predominance of platelets of non-standard/pathological shape/volume **Macrocytic PLT – these are large immature (young) insufficiently functional platelets that leave the bone marrow early into the blood *** Microcytic PLT – these are old, small volume, poorly functioning platelets
Normal ratio of different forms of platelets in the bloodstream
| Characteristics of PLT | Relative content |
| Standard (mature) functional | 87% |
| Young (immature) macroplatelets | 3,2% |
| Old microplatelet | 4,5% |
| Non-standard (forms of irritation) | 2,5% |
PLT and MPV have the greatest diagnostic value in blood tests.
Thrombocrit (PCT) and platelet anisacytosis (PDW) are secondary indicators. So PDW directly depends on MPV. The PCT score has no clinical significance. Read more about MPV: Average platelet volume is reduced
PLT in blood test is normal
Standard rate of platelets in the blood PLT: 150 – 400 x109/l
Normal* indicators of the platelet component of the hemogram: PLT: 150 – 400 x109/l MPV: 7-11 fl (fl, femtoliters) PDW: 10-20% PCT: 0.15 – 0.40%
*it is better to evaluate the data of an automated blood counter according to the standards (reference values) of the local laboratory - the settings of different models of hemoanalyzers are not the same
Important!
- The error of the hemoanalyzer when calculating PLT is about ≈5%
- An automated blood test cannot completely replace the “manual” counting of a blood smear under a microscope
- It is impossible to reliably assess a disorder of the blood system or make a final diagnosis if any one blood indicator does not correspond to the norm
- If an increase/decrease in PLT is detected in an automated hemogram, a control microscopy of a stained blood smear with a “manual” platelet count is required.
False thrombocytosis, false thrombocytopenia - causes of hemoanalyzer errors
1. There are many giant macroplatelets in the smear - the heme analyzer counts them as red blood cells 2. Many microplatelets - the hemoanalyzer does not count them (takes them for debris - “cellular debris”) 3. Aggregated (“glued together”) platelets - not amenable to automated counting 4. Satelliteism - attachment of platelets to the surface of leukocytes - not amenable to automated counting
PLT blood test decoding - the norm in women and men
The number of platelets in the blood of women and men is almost the same.
- The PLT norm in blood tests for women and men is the same: 150-400 x10^9/l
However, the diameter of platelets in men and elderly people is slightly higher than in girls and women of childbearing age. Therefore, MPV norms for these populations are slightly higher.
To simplify the interpretation of a blood test, you can use the standards acceptable for practically healthy people of any gender and age.
| Index | Acceptable norm for healthy women and men of any age |
| PLT - platelets | 100 – 450 x10^9/l |
| MPV - mean platelet volume | 6 – 12 fl |
PLT blood test decoding - the norm in children
A number of laboratories, doing the classic “manual counting” of stained smears under a microscope, designate platelets in a blood test with alternative units of measurement: thousand/μl __x10^3 cells/μl
The conversion factor into standard units of measurement is 1: __x10^9/l = __x10^9 cells/liter = __x10^3 cells/μl = thousand/μl
TRO (PLT) standards in children
(microscopy of stained smears using the Fonio method)
| Age | Norm PLT __х10^3 cells/μl |
| 0-2 weeks | 144 — 449 |
| 2 weeks – 1 month | 248 — 586 |
| 1-2 months | 229 — 597 |
| 2-6 months | 244 — 580 |
| 0.5 – 2 years | 206 – 459 |
| 26 years | 189 — 403 |
| over 6 years old | 140 – 400 |
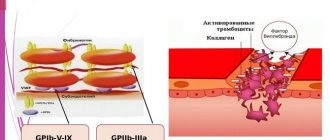
Platelet aggregation with ristocetin
Determination of platelet aggregation with ristocetin in plasma is used to quantify von Willebrand factor. The method is based on the ability of ristocetin to stimulate in vitro the interaction of von Willebrand factor with platelet glycoprotein Ib. In most cases of von Willebrand disease, there is a violation of ristocetin aggregation with a normal response to the effects of ADP, collagen and adrenaline. Disturbances in ristocetin aggregation are also detected in Bernard-Soulier disease. For differentiation, a test with the addition of normal plasma is used: in von Willebrand disease, after the addition of normal plasma, ristocetin aggregation is normalized, while in Bernard-Soulier syndrome this does not happen. Ristocetin-induced platelet agglutination is reduced in most cases of von Willebrand disease, except type IIB.
Platelet aggregation with collagen
Platelet aggregation with collagen has a fairly pronounced latent phase, during which phospholipase C is activated. Depending on the concentration of the reagent used, the duration of this phase can be 5-7 minutes. After the end of this period, processes occur in platelets that lead to the formation of second messengers, as a result of which the secretion of platelet granules and the synthesis of thromboxane A2 develop, which is accompanied by a sharp increase in interplatelet interaction.
In laboratory and clinical practice, collagen is most often used in a final concentration of 50 μg/ml, however, collagens from different companies may have different activities, which must be taken into account when using them.
Testing for PLT in children
Monitoring blood composition, including PLT levels, is especially important in childhood. If this indicator drops below normal, the following diseases can be assumed:
- allergic reactions to medications;
- intoxication;
- thyrotoxicosis;
- blood diseases;
- parasitic and viral infections.
The causes of elevated PLT levels in children are varied. There are primary and secondary thrombocytosis. The first is due to the fact that brain stem cells produce an excess amount of platelets with an altered structure, which, for example, is observed in leukemia.
Secondary, or reactive, develops as a result of some pathological process, which disrupts the production of these cells, as well as their structure and shape. Factors in the development of reactive thrombocytosis include:
- heavy operations;
- splenectomy;
- sudden bleeding;
- osteomyelitis;
- anemia;
- fractures of tubular bones;
- pulmonary infections;
- malignant diseases;
- some drugs.
Video about the functions of platelets and the reasons for changes in their number in the blood:
Platelet aggregation with adrenaline
Adrenaline, upon contact with platelets, interacts with α2-adrenergic receptors, which causes inhibition of adenylate cyclase. It is possible that the mechanism underlying the implementation of the effect of adrenaline and the development of the first wave of aggregation does not depend on the formation of thromboxane A2, the release reaction or the synthesis of platelet aggregation factor, but is associated with the ability of adrenaline to directly change the permeability of the cell membrane to calcium ions. The second wave of aggregation occurs as a result of the release reaction and production of thromboxane A2.
Platelet aggregation with arachidonic acid
Arachidonic acid is a natural aggregation agonist, and its action is mediated by the effects of prostaglandins G2 and H2, thromboxane A2, and includes activation of both phospholipase C with subsequent formation of second messengers, mobilization of intracellular calcium and expansion of the cell activation process, and phospholipase A2, which directly leads to release of endogenous arachidonic acid. Platelet aggregation with arachidonic acid occurs quite quickly, so the curve characterizing this process is often single-wave in nature.
To induce aggregation of blood platelets, arachidonic acid is used in concentrations of 10-3-10-4 mol. When working with arachidonic acid, it should be taken into account that in air this substance oxidizes very quickly.
An aggregation test with arachidonic acid is recommended in cases of using drugs that affect the aggregation reaction (for example, acetylsalicylic acid, penicillin, indomethacin, delagil, diuretics), which must be taken into account when assessing the research results.
How to normalize the number of platelets in the blood
Obviously, in order to normalize PLT in the blood, it is necessary to conduct a further examination, find out and cure (eliminate) the reason for their decrease or increase.
In case of secondary thrombocytosis or thrombocytopenia, cure of the primary disease leads to normality and PLT.
Thrombocytosis - how to reduce the number of platelets in the blood
| Thrombocytosis | How to reduce PLT |
| Secondary (reactive) | 1. Treatment (or elimination) of a primary disease (or condition), one of the symptoms of which was an increase in PLT in the blood 2. Stop smoking 3. Normalization of body weight 4. Sufficient consumption of clean water (at least 30-40 ml per 1 kg of body weight per day) |
| Primary (essential) | 1. Aspirin at a dose of 81 mg per day (to reduce the risk of blood clots) 2. Medicines that reduce the level of platelets in the blood (hydroxyurea, anagrelide, etc.) 3. Thrombocytopheresis (according to indications) 4.Interferon alpha-2b (according to indications) 5. Cytotoxic antitumor agents (according to indications) 6. Bone marrow transplant (if indicated) |
Products useful for thrombocytosis
Unrefined vegetable oil (flaxseed, olive, pumpkin, etc.) Fish oil, seafood Tomatoes, tomato paste Lemons Sea buckthorn Ginger Garlic Green tea Drinking water 40-50 ml per 1 kg of body weight per day or more
Thrombocytopenia - how to increase the number of platelets in the blood
When platelets decrease to 100-50 x10^9/l, special treatment, as a rule, is not required. This condition is not dangerous, but requires mandatory monitoring and clarification of the cause of the decrease in PLT.
Important! Patients with thrombocytopenia are recommended to completely abstain from alcohol.
Foods useful for thrombocytopenia
Pomegranate Beetroot Nuts Green leafy vegetables, herbs Liver, red meat Buckwheat Oatmeal Rosehip decoction Chokeberry Stinging nettle (tea, decoction)
It is important to note that there is no special diet to truly effectively increase blood platelets.
The patient's diet should be hypoallergenic and complete and varied: rich in proteins, vitamins and microelements. Dishes are steamed, boiled or baked. Spicy, mechanically rough, too hot or cold foods should be avoided.
How to increase platelets in the blood
- Treatment of thrombocytopenia begins when PLT is below 50 x10^9/l
| How to increase PLT in the blood | Note |
| Prednisolone (corticosteroid hormone) | Used for the treatment of immune (autoimmune, drug) thrombocytopenia (ITP). The individual daily dose and duration of taking prednisolone is prescribed by the doctor |
| Human immunoglobulin (Intraglobin, Imbiogam) | It is administered intravenously, drip-wise, slowly, in a hospital setting. Used for the treatment of ITP, chronic lymphocytic leukemia, multiple myeloma |
| Stimulator of thrombopoiesis in the bone marrow (thrombopoietin receptor agonist): Eltrombopag (Revolade) | Indicated for chronic ITP and unspecified thrombocytopenia when treatment with prednisolone, immunoglobulin is ineffective, and with insufficient effect of splenectomy |
| Stimulators of hematopoiesis in the bone marrow (recombinant erythropoietins): Recormon, Eralfon, Erythrostim | Used strictly according to indications under the supervision of an oncologist-hematologist for the complex treatment of symptomatic thrombocytopenia and anemia in patients receiving chemotherapy |
| Transfusion of donor platelets (thrombomass) | Performed in the hospital for life-threatening conditions associated with severe thrombocytopenia, including in patients receiving chemotherapy |
| Vincristine (antitumor drug) | Used to treat ITP when prednisolone is ineffective |
| Vitamin B12 | Indicated for the treatment of thrombocytopenia in megaloblastic anemia |
| Splenectomy (surgical removal of the spleen) | Performed when treatment with ITP with prednisone is ineffective |
| Bone marrow transplantation | Use strictly according to indications |
Which doctor should you contact if you have low or high PLT in your blood test: general practitioner, hematologist
- Tags:
Save the article for yourself!
3 comments
Tatyana08/14/2018 at 20:20
Everything is very detailed, just chewed on the shelves. Thank you very much for the article.
Christina 08/17/2018 at 16:19
Please help me decipher the smear analysis! Leukocytes uterus>100, vagina>100. Epithelium. cells of the cervix um/n, vagina b/n. Cocci cervix b/p, vagina vol.?
Tatyana21.10.2018 at 09:16
Hello! Please help me with decoding. Description b/m sticks +++, squamous epithelium in the form of layers of mature cells. Description of c/c mucus, erythrocytes, fibrin, groups of flat cells, numerous glandular structures proliferating, including hyperplastic type glandular cells, their endometrial origin cannot be excluded; groups of cylindrical cells. NILM. Signs of hyperplasia of the glandular epithelium. Thank you