Atherosclerosis: risk factors, prevention
Updated: 12/13/2016, 10:42 Published: 12/13/2016, 10:42
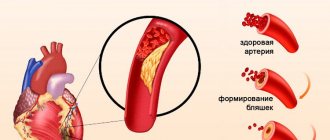
Atherosclerosis is a chronic disease of blood vessels, in which cholesterol and other fats are deposited on the inner wall of the arteries in the form of plaques and plaques, and the walls themselves become denser and lose elasticity . The vessels gradually become hard due to the settling of fats and lime on the walls, lose their elasticity and, as a result, narrow, which, as is known, reduces blood access to the organs. Eventually the vessel may close completely. And when this is accompanied by a blood clotting disorder, there is a tendency to thrombosis and ischemic damage to organs occurs.
Risk factors play a role in the development and progression of atherosclerosis
:modifiable (which can be eliminated or adjusted) and non-modifiable (they cannot be changed).
Modifiable factors include:
1. Lifestyle: physical inactivity, abuse of fatty, cholesterol-rich foods, personality and behavior characteristics - stressful character type, alcohol abuse, smoking.
2. Arterial hypertension, blood pressure 140/90 mm Hg. and higher.
3. Diabetes mellitus, fasting blood glucose level more than 6 mmol/l.
4. Hypercholesterolemia (blood cholesterol level more than 5 mmol/l).
5. Abdominal obesity (waist circumference in men is more than 102 cm and more than 88 cm in women).
Non-modifiable factors include:
1. Age: men over 45 and women over 55 or with early menopause.
2. Male gender (men develop atherosclerosis 10 years earlier than women).
3. A family history of cases of early atherosclerosis. Familial hypercholesterolemia with a genetic basis. Myocardial infarction, stroke, sudden death in close relatives under the age of 55 years for a man and 65 years for a woman.
What does it lead to?
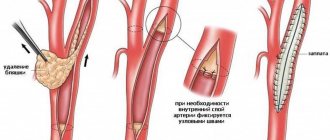
An atherosclerotic plaque or part of it can break off and, along with the blood flow, begin traveling through the arteries. Plaques get stuck in smaller vessels, block the movement of blood through them and cause disruption of blood supply
to entire areas of tissue.
If a vessel in a limb becomes clogged, the muscles die due to lack of nutrition and oxygen, and gangrene
.
And if the plaque reaches the arteries of the brain and gets stuck in them, a stroke develops. In some cases, atherosclerotic plaques stretch certain parts of the artery, causing the formation of an aneurysm
- a bulge in the artery wall due to its thinning and stretching.
Symptoms of atherosclerosis are not noticeable until plaque restricts or blocks blood flow in the arteries. The possible onset of an atherosclerotic process is indicated only by an increase in systolic (upper) pressure
.
Depending on the location of the artery, the lack of blood flow can manifest itself in the form of different symptoms
. Starvation of the heart muscle leads to pain in the heart - angina. Lack of blood supply to the brain impairs memory. Clogged blood vessels in the extremities lead to muscle pain, first while walking, and then at rest.
Symptoms of atherosclerosis
Vascular changes are often localized in the aorta, cardiac, cerebral, renal arteries and arteries of the extremities, most often the lower ones. The picture of the disease and the patient’s complaints depend on the damage to certain arteries. Thus, atherosclerosis of the coronary arteries (heart vessels) very often manifests itself in the form of angina pectoris and heart attack. At the heart of the pathological process, i.e. disease, there is a violation of the correspondence between the need of the heart for blood supply and its actual implementation. Often, severe forms of aortic atherosclerosis can be asymptomatic. The patient may experience pressing or burning pain behind the sternum, radiating to both arms, neck, back, and upper abdomen. But unlike angina, these pains last a long time, sometimes intensifying and sometimes weakening.
When the renal vessels are damaged, severe arterial hypertension occurs. Atherosclerosis of the cerebral arteries is manifested by decreased performance (especially mental), decreased memory, active attention, and fatigue. Over time, dizziness and insomnia appear, patients become fussy, obsessive, and picky. Their intelligence decreases. A complication of atherosclerosis of the cerebral arteries is a violation of cerebral circulation, hemorrhage (stroke), thrombosis. Atherosclerosis of the arteries of the extremities, most often the lower ones, manifests itself in the calf muscles when walking (“intermittent claudication”). Chilliness and coldness of the extremities appear. Thus, atherosclerosis leads to the development of most modern “diseases of civilization.”
If atherosclerotic changes are suspected, consultation with specialists is indicated:
cardiologist (for coronary heart disease); ophthalmologist (atherosclerosis of the fundus vessels); neurologist (cerebral atherosclerosis); nephrologist (atherosclerosis of the renal arteries); vascular surgeon (atherosclerosis of the vessels of the lower extremities, aorta). To clarify the degree of atherosclerotic lesion, additional instrumental research methods may be prescribed: electrocardiography, angiography, coronary angiography , intravascular ultrasound, duplex and triplex scanning, magnetic resonance imaging and others.
Prevention of atherosclerosis
Anti-atherosclerotic diet. Diet recommendations are given to all patients taking into account cholesterol levels and other risk factors: obesity, arterial hypertension, diabetes mellitus. The diet should be varied, in accordance with the cultural traditions of the patient. The calorie content of the daily diet should be sufficient to achieve and maintain normal weight.
Consumption of total fat should not exceed 30% of the calorie content of the diet. It is recommended to limit the consumption of animal fats (butter, cream, meat, lard), replacing them with vegetable fats. Daily consumption of fresh vegetables and fruits should be at least 500g per day.
It is recommended to consume lean meat and skinless poultry, fermented milk products, low-fat cottage cheese, grain bread, with bran, and foods enriched with unsaturated fatty acids (sea and ocean fish - salmon, mackerel, tuna, etc.). Limit the consumption of table salt to 6g per day, which corresponds to 1 teaspoon. Following a diet can reduce cholesterol levels by up to 10%.
Refusal to drink alcohol.
Health-safe alcohol consumption (no more than 20-30 ml of pure ethanol per day for men and no more than 20 ml per day for women) is permissible only for practically healthy individuals. Drinking 5 servings of alcohol (60g per day) increases the risk of cardiovascular complications by 65%.
Normalization of body weight indicators. Excess body weight and obesity, especially abdominal obesity (waist circumference in men more than 102 cm and more than 88 cm in women), increase the risk of developing cardiovascular diseases. To lose weight, an individual diet is selected taking into account age and concomitant diseases.
Physical activity for atherosclerosis. Increasing physical activity has a positive effect for patients with atherosclerosis. Patients without clinical manifestations of atherosclerosis are advised to exercise for 30 minutes daily. Patients with cardiovascular diseases require a constant regime of dynamic physical activity, taking into account the results of stress tests. Walking, swimming, and dancing of moderate intensity for 60-90 minutes a week are beneficial. Isometric (power) loads are unacceptable. It is recommended to use any opportunity for physical activity: walking, using a car less often.
The most important
The main reasons for the development of atherosclerosis - clogging of arteries with fatty plaques - are smoking, alcohol and eating large amounts of fatty foods. Atherosclerosis leads to heart attacks, strokes and impaired blood flow in various organs of the body. A healthy lifestyle will help you avoid this disease. A smoker can call 8-800-200-0-200
(the call is free for residents of Russia), say that he needs help quitting smoking, and he will be switched to specialists at the Advisory Call Center for Help in Quitting Tobacco Consumption (CTC) . If all KTC specialists are busy at this moment, his phone number will be sent to KTC by e-mail, and they will call him back within 1-3 days. Psychologists and doctors provide counseling to those who contact the CTC. Psychologists help prepare for the day of quitting smoking, help find a replacement for smoking rituals, together with the client they will determine the optimal ways to overcome addiction, and support in difficult moments in the fight against nicotine addiction. Doctors will advise on the most effective therapeutic methods for quitting smoking, and give advice to patients with various diseases on how best to prepare for quitting smoking, taking into account existing health problems. Illustration: The Junk Food
Tags:
- Smoking
- Heart and blood vessels
- Alcohol
- Cholesterol
To leave a comment you must be an authorized user
Statistics
Statistics on atherosclerosis are very disappointing. After 30-35 years, 75% of men and 38% of women suffer from atherosclerosis. At the age of 55-60 years, these figures are close to 100%. However, mortality from atherosclerosis averages 58% (mainly from acute heart attacks and strokes), although in some countries it reaches 69%. It is clear that not every person suffering from atherosclerosis dies from it before ending his life from cancer, diabetes mellitus or another disease of civilization. Many stroke victims remain confined to a bed or wheelchair for the rest of their lives. Atherosclerosis develops gradually, on average 15-20 years before the appearance of the first clinical symptoms. Today, in a number of cases, cardiologists note the onset of atherosclerosis already in adolescence, which was considered an incredible fact 100 years ago. By the way, the mortality rate from this disease then was no more than 5-6%. And in the times of Vedic civilization, it was just a sign of old age.
Atherosclerosis is most developed in technocratic countries, especially in the USA, Germany, Sweden, England, Finland and Denmark. Recently, they have quickly begun to catch up with the large cities of Russia and Ukraine. In Moscow, St. Petersburg, Yekaterinburg, Kyiv and Dnepropetrovsk, for example, the mortality rate from acute heart attacks and strokes has now reached 65%. Specialized cardiology programs to combat cardiovascular diseases in the United States, launched about 25 years ago, have reduced mortality from atherosclerosis from 69% to 45%. Mortality from this pathology is lowest in Japan, India, Nepal, Burma and some Latin American countries.
Pathogenesis
The pathogenesis of atherosclerosis is called atherogenesis. This happens in several stages. The development of atherosclerotic lesions is a combination of processes of absorption and release of lipoproteins and leukocytes into the intima, proliferation and death of cells, formation and restructuring of the intercellular substance, as well as vascular growth and vascular calcification. These processes are driven by multiple signals, often in different directions. There is increasing evidence of a complex pathogenetic relationship between changes in the functions of vascular wall cells and migrating leukocytes and risk factors for atherosclerosis.
Accumulation and modification of lipoproteins. As a rule, the arterial intima is formed by a single-celled endothelial layer, under which there are smooth muscle cells embedded in the intercellular substance. The first manifestations of the disease are so-called lipid spots. Their appearance is associated with local deposits of lipoproteins in the intima. Not all lipoproteins have atherogenic properties, but only low-density lipoproteins (LDL) and very low-density lipoproteins (VLDP). Initially, they accumulate in the intima mainly by binding to intercellular components - proteoglycans.
Where lipid patches form, heparan sulfates predominate over the other two glycosaminoglycans, keratan sulfates and chondroitin sulfates. In the intima, lipoproteins, especially those associated with proteoglycans, can react chemically. Two main roles are played: oxidation and non-enzymatic glycosylation. Unlike plasma, intima contains few antioxidants. A mixture of oxidized lipoproteins is formed, as a result of which both lipid and protein components are oxidized.
In the process of lipid oxidation, hydroperoxides, lysophospholipids, oxysterolipids and aldehydes are formed (in the process of fatty acid peroxidation). Oxidation of apoproteins leads to the rupture of peptide bonds and the connection of amino acid side chains (mainly the lysine amino group) with the products of the breakdown of fatty acids (4-hydroxynonenal and malondialdehyde). Persistent hyperglycemia in diabetes mellitus promotes non-enzymatic glycosylation of apoproteins and intimal proteins, which also impairs their functions and accelerates atherogenesis.
Migration of leukocytes and formation of xanthomas (foam cells) Calcification of the vessel wall. The migration of leukocytes, mainly monocytes and lymphocytes, is the second stage in the development of lipid staining. Their migration into the intima is ensured by endothelial receptors - adhesion molecules. The molecules VCAM-1 and ICAM-1 (from the immunoglobulin superfamily) and P-selectin deserve special attention.
The synthesis of adhesion molecules can increase the number of cytokines. For example, interleukin-1 (IL-1) and tumor necrosis factor (FNO?) induce or enhance endothelial cell synthesis of VCAM-1 and ICAM-1. In turn, the release of cytokines by the cells of the vessel wall is stimulated by modified lipoproteins. A vicious circle has formed. It plays the role and nature of blood flow. In most areas of the invariant artery, laminar flow of blood and the resulting forces reduce the expression (manifestation) of adhesion molecules on the surface of endothelial cells. Laminar blood flow also promotes the formation of NO oxides in the endothelium.
In addition to its vasodilatory effect, NO at low concentrations maintained by the endothelium has an anti-inflammatory effect, for example, by reducing the synthesis of VCAM-1. But at branch points, laminar flow is often disrupted, and atherosclerotic plaques are usually found there.
After adhesion, leukocytes pass through the endothelium and enter the intima. Lipoproteins can directly enhance migration: oxidized LDL promotes leukocyte chemotaxis. Monocytes are involved in further lipid staining. In the intima, monocytes transform into macrophages, which form lipoprotein-induced xanthoma-filled (foam) cells due to lipoprotein receptor-mediated endocytosis. It was previously thought that the known LDL receptors were involved in endocytosis, but when these receptors are defective, both experimental animals and patients (eg, familial hypercholesterolemia) still exhibit numerous xanthomas and atherosclerotic plaques filled with cells filled with xanthomas.
In addition, exogenous cholesterol inhibits the synthesis of these receptors, and in hypercholesterolemia there are only a few of them. Currently, the role of macrophages (which primarily bind modified lipoproteins) and other receptors for oxidized LDL and small atherogenic LDL is assumed. Some xanthoma cells, which have taken up lipoproteins from the intercellular substance, emerge from the artery wall and thus prevent the accumulation of lipids in the artery. When lipoproteins are intuitively injected into intuitively superior release by macrophages (or other means), lipids accumulate and form atherosclerotic plaques. In a growing plaque, some xanthoma cells undergo apoptosis or necrosis. As a result, a cavity is formed in the center of the plaque, filled with lipid-rich masses, which is characteristic of the later stages of atherogenesis.
Pro- and anti-atherogenic factors. Upon ingestion of modified lipoproteins, macrophages secrete cytokines and growth factors that promote plaque formation. Only cytokines and growth factors stimulate the division of smooth muscle cells and the synthesis of intercellular substance, which accumulates in the plaque. Other cytokines, especially interferon, from activated T lymphocytes, interfere with smooth muscle cell division and collagen synthesis. Factors such as IL-1 and FNO induce the formation of platelet-derived growth factor and fibroblast growth factor in the intima, which play a role in the future fate of plaques.
Therefore, there is a complex interaction of factors that both accelerate and suppress atherogenesis. The role of non-protein intermediaries is also important. Activated macrophages and vascular wall cells (endothelial and smooth muscle cells) produce free oxygen radicals, which stimulate the proliferation of smooth muscle cells, improve the synthesis of cytokines and bind NO. On the other hand, activated macrophages are capable of producing induced NO synthesis.
This highly active enzyme produces NO in high, potentially toxic concentrations—in contrast to the low concentrations of NO produced by the enzyme's constituent form, endothelial NO synthase. In addition to macrophages, high-density lipoproteins (HDL) are also involved in the removal of cholesterol from the affected intima and are responsible for the so-called reverse cholesterol transport. A clear inverse relationship has been demonstrated between HDL cholesterol concentrations and the risk of CBS formation. Women of childbearing age have higher concentrations of HDL cholesterol than their male counterparts, and this is the main reason why women are less likely to suffer from atherosclerosis. The experiment shows that PAPs are able to remove cholesterol from xanthoma cells.
Involvement of smooth muscle cells. An atherosclerotic plaque develops from a lipid stain, but not all spots become plaques. If lipid spots are characterized by the accumulation of xanthoma cells, then in plaques there is fibrosis. The intercellular substance in the plaque is mainly synthesized by smooth muscle cells, the migration and proliferation of which is probably a critical moment in the formation of a fibrous plaque at the site of accumulation of xanthoma cells. Migration of smooth muscle cells into the lipid region, their proliferation and synthesis of intercellular substances are caused by cytokines and growth factors released under the influence of modified lipoproteins and other substances by macrophages and cells of the vascular wall.
Thus, platelet growth factor released by activated endothelial cells stimulates the migration of smooth muscle cells from the environment into the intima. Local growth factors cause the division of both intimal smooth muscle cells and cells coming from the media. One of the powerful stimulators of synthesis by these collagen cells is transforming growth factor p. In addition to paracrine (factors coming from neighboring cells), there is also autocrine (factors produced by the cell itself) regulation of smooth muscle cells. As a result of the changes occurring in them, the transition of the lipid spot into an atherosclerotic plaque, containing a large number of smooth muscle cells and intercellular substance, is accelerated. Like macrophages, these cells can undergo apoptosis, which is caused by cytokines that promote atherosclerosis.
Etiology
Therefore, there is no single theory about the origin of this disease.
The following options are available, as well as their combinations:
- theory of lipoprotein infiltration - the primary accumulation of lipoproteins in the vessel wall,
- theory of endothelial dysfunction - primary violation of the protective properties of the endothelium and its mediators
- Autoimmune - primary disorder of macrophage and leukocyte function, their infiltration of the vascular wall,
- monoclonal - the primary appearance of pathological clones of smooth muscle cells,
- viral - primary viral damage to the endothelium (herpes, cytomegalovirus, etc.),
- Peroxide is a major disruptor of the antioxidant system,
- genetically - a primary hereditary defect of the vascular wall,
- Chlamydia is the primary lesion of the vascular wall in chlamydia, mainly chlamydia pneumonia.
From all this, however, two main theories can be distinguished.
According to the first, atherosclerosis develops by deposition of lipids onto the vessel wall as a result of an increase in the absolute content of lipids in the blood or a violation of lipoprotein (LP) metabolism.
The second theory is based on the fact that damage to the vessel wall (mechanical, chemical or immunological) is necessary for the disease to occur and that lipid deposition, although important in the progression of damage, is secondary. The accumulation of cholesterol (CC) in areas with atherosclerotic lesions of the vascular wall was identified at the end of the last century, but this fact acquired special significance after the experiments of N. N. Anichkov and S. V. Anichkov and S. V. Anichkov. S. Khalatov, in which the addition of XS to the food of rabbits led to the formation of aortic lesions reminiscent of atherosclerotic lesions of human vessels.
Factors contributing to atherosclerosis:
- Inherited constitutional predisposition;
- Nutrition factor - unhealthy diet with excess fats and carbohydrates and lack of vitamin C;
- Psycho-emotional stress;
- High pressure;
- Metabolic factor (for diseases such as diabetes, obesity, decreased thyroid function);
- A vascular factor associated with a violation of the nervous regulation of blood vessels, their damage in various infectious and infectious-allergic diseases.
Permitted and prohibited foods for atherosclerosis
Now let's move on directly to the menu that can be recommended for people with atherosclerosis.
List of permitted products:
- Meat (in small quantities!): chicken and turkey fillet, rabbit, lean veal, skinless chicken, quail.
- Fish: all white fish (cod, flounder), herring, sardines, tuna, salmon (chum salmon, pink salmon, salmon).
- Fats: olive, sunflower, soybean, corn oil, nuts, seeds (sesame, flax, chia).
- Dairy and fermented milk products: skim milk, low-fat cheeses (pressed cottage cheese), kefir, yogurt, natural yogurt, low-fat cheese, ayran.
- Legumes: peas, beans, lentils, asparagus, soybeans.
- Vegetables and fruits: carrots, beets, tomatoes, cucumbers, onions, garlic, zucchini, peppers, eggplants, cabbage, boiled potatoes (or in their jackets).
- Cereals: buckwheat, oatmeal, brown rice, pasta and wholemeal bread.
- Baked goods: low fat puddings, jellies, sorbet.
- Drinks: green tea, natural fresh juices without sugar, compote or uzvar without sugar, still mineral water.