Causes of chest heaviness
Physiological factors
As a rule, a person experiences an unpleasant heaviness in the chest when there is severe fear or anxiety. There is a feeling that everything is shrinking inside, nagging or aching pain appears. Symptoms are accompanied by interruptions in work or a feeling of cardiac arrest. Discomfort in the chest is sometimes perceived as the onset of a heart attack, but the condition returns to normal immediately after the person calms down and the traumatic factor disappears.
Depression
Heaviness with aching pain in the chest, which is most pronounced in the first hours after waking up, is pathognomonic for masked depression. Patients are concerned about discomfort in the precordial area, sometimes the condition is aggravated by pressing or squeezing pain. Characterized by the absence of mood changes typical for depression, patients are confident that they have a cardiac disease.
Diseases of the cardiovascular system
Heaviness and discomfort in the chest projection are often associated with cardiac problems. In such cases, symptoms are more typical for middle-aged and elderly people. Unpleasant sensations are often combined with tingling or pain in the heart area, shortness of breath during exercise, and swelling of the lower extremities. Heaviness in the chest is a manifestation of heart lesions such as:
- IHD.
Stable angina is characterized by periodic episodes of chest tightness and squeezing pain. Severity develops at the beginning of paroxysm, provoked by physical activity or stress. Sometimes the symptom continues to bother the patient even in the periods between attacks of angina. - Myocarditis.
The pathology manifests itself suddenly and is more common in young patients. A person complains of heaviness with moderate aching chest pain, accompanied by shortness of breath and fever. Sometimes there are interruptions in the heart rhythm. - Pericarditis.
With exudative inflammation of the pericardium, patients feel increasing heaviness, tightness in the chest, and progressive shortness of breath. Changing body position does not affect the intensity of symptoms. Swelling of the neck veins and puffiness of the face are usually noticeable. - Cardiomyopathy.
Non-inflammatory heart disease is characterized by constant or periodic heaviness in the chest, which bothers a person for several months or even years. The manifestations are moderate and do not interfere with normal life, so patients consult a doctor only if the problem worsens and heart failure develops. - Cardiac tamponade.
Patients experience sudden heaviness in the chest, inability to breathe deeply, severe weakness and cold sweat. The condition is life-threatening and, without medical attention, ends in collapse or acute heart failure. - Post-infarction syndrome.
The disease is characterized by the appearance of pressing pain and heaviness in the chest 2-4 weeks after myocardial infarction. Patients notice a deterioration in their health, an increase in shortness of breath and weakness, and discomfort in the chest cavity. Often the clinical picture is supplemented by fever.
Heaviness in the chest
Respiratory diseases
Damage to the bronchopulmonary system is another common cause of heaviness, pressing and squeezing sensations in different parts of the chest. The symptom most often occurs as part of typical inflammatory processes: acute and chronic bronchitis, pneumonia. Discomfort increases during coughing attacks or attempts to take a deep breath. Heaviness in the chest is accompanied by fever, weakness, and the release of mucous or purulent sputum.
In chronic processes - tuberculosis, pneumoconiosis - patients complain of periodic tightness in the chest area, incomprehensible discomfort or aching sensations. Manifestations occur without any visible provoking factor and persist for many months. When the pathology worsens, the heaviness in the chest is replaced by a dull pain.
Attacks of heaviness and a feeling of chest compression are observed during exacerbation of bronchial asthma. Unpleasant symptoms develop as harbingers of a paroxysm of suffocation and are accompanied by nasal congestion, itching, and coughing. During the interictal period, patients with moderate and severe asthma experience heaviness in the chest.
Mediastinal lesion
Heaviness and periodic pain in the chest occur with chronic mediastinitis. Symptoms are mild, periodically they intensify and are supplemented by fever. Patients complain of pressing or dull pain without clear localization, discomfort when taking a deep breath and coughing. Similar manifestations occur with mediastinal neoplasms: thymoma, lymphoma, cysts.
Rare causes
- Poisoning
: citrate intoxication, hydrogen sulfide poisoning. - Digestive diseases
: GERD, achalasia cardia, dilatation of the esophagus. - Emergency conditions
: anaphylactic shock, heat stroke, toxic pulmonary edema.
Heart disease: symptoms
Heart disease includes conditions such as coronary artery disease, heart attack, heart failure and congenital heart disease. Heart disease is the leading cause of death in the world's population. To prevent the disease, it is recommended to quit smoking, lower cholesterol, control high blood pressure, maintain a normal weight, and do physical exercise.
Although many heart conditions have similar symptoms, each heart disease (coronary artery disease, heart attack) has its own specific symptoms. Symptoms depend on the type and severity of your heart condition. Learn to recognize your symptoms and the situations that lead to them. Tell your doctor if you develop new symptoms, become more frequent, or become more severe.
Coronary heart disease
The main symptom is angina. With angina, discomfort, a feeling of heaviness, pressure, aching pain, burning, compression, and a feeling of pain in the chest area are noted. It can be confused with indigestion or heartburn. Typically, angina symptoms are localized in the chest, but they can also spread to the shoulders, arms, neck, throat, jaw or back.
Other symptoms that may occur with coronary heart disease include:
- Dyspnea
- Irregular heartbeat or shuffling sensation in the chest
- Rapid heartbeat
- Feeling weak or dizzy
- Nausea
- Sweating
Heart attack (myocardial infarction):
- Feeling of discomfort, pressure, heaviness, pain in the chest, arm, or under the breastbone
- Discomfort radiating to the back, jaw, throat or arm
- Feeling of heaviness in the stomach, indigestion, feeling of suffocation (like heartburn)
- Sweating, nausea, vomiting, dizziness
- Complete weakness, anxiety, shortness of breath
- Fast or irregular heartbeat
In a heart attack, symptoms usually last 30 minutes or longer and are not relieved by rest or oral medications (medicines taken by mouth). Initial symptoms may appear as mild discomfort, which over time progresses to severe pain.
In some people, a heart attack has no symptoms (“silent” myocardial infarction). Silent myocardial infarction can happen to anyone, but diabetics are more susceptible to it.
If you think you are having a heart attack, DON'T DELAY. Call the emergency number. The faster the treatment, the less damage is done to your heart.
Arrhythmia
With arrhythmia, symptoms may be as follows:
- Erratic heartbeat, feeling of “shuffling, shaking,” feeling like your heart is “running away”)
- Rolling in the chest
- Dizziness, fainting
- Loss of consciousness
- Dyspnea
- Discomfort in the chest area
- Weakness, fatigue
Atrial fibrillation
Atrial fibrillation is a type of arrhythmia. Most people experience one or more of these symptoms:
- Palpitation of the heart (sudden sensation of rocking, trembling, “acceleration” of the heart)
- Lack of energy, fatigue
- Dizziness (fainting)
- Discomfort in the chest area (pain, pressure)
- Dyspnea (difficulty breathing during normal activities)
- Some patients with atrial fibrillation have no symptoms. Sometimes these episodes can be short-lived
Heart valve disease
Symptoms of heart valve disease may include:
- Shortness of breath and/or inability to catch your breath. You may feel it when you are active (doing normal activities) or when you are lying prone in bed.
- Weakness or dizziness
- Discomfort in the chest area. You may feel pressure or heaviness in your chest when active or when going out into the cold
- Palpitation (fast heart rate, irregular, racing heartbeat, or a feeling of “shuffling” in the chest)
If valve disease leads to heart failure, symptoms may include:
- Swelling of the ankles, feet, abdomen. Swelling can also occur inside the abdomen, leading to a feeling of bloating
- Rapid weight gain (weight gain of 2-3 pounds per day)
Symptoms do not always correspond to the severity of valve disease. Acute valve disease, which requires immediate treatment, may be asymptomatic. Or, conversely, in case of acute symptoms (for example, in the case of mitral valve prolapse), test results may show a mild form of valve disease.
Heart failure
The following symptoms occur in heart failure:
- Shortness of breath while active (usually) or at rest, especially when you are lying prone in bed
- Wet cough producing white sputum
- Rapid weight gain (weight gain of 2-3 pounds per day)
- Swelling of the ankles, legs and abdomen
- Dizziness
- Fatigue, weakness
- Fast or irregular heartbeat
- Nausea, palpitation, chest pain
As with valve disease, the symptoms of heart failure don't always relate to how weak your heart is. You may have many symptoms and only have slightly reduced heart function. Or, conversely, with a seriously affected heart, experience minor symptoms or feel nothing at all.
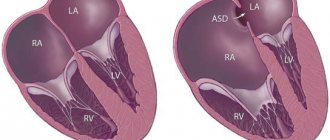
Congenital heart defect
Congenital heart defects can be diagnosed before birth, immediately after birth, during childhood, or during adulthood. It is possible to have a defect and not experience any symptoms. In their absence, the defect can sometimes be diagnosed due to a heart murmur on physical examination or if there is an abnormal ECG or chest x-ray.
In adults, if symptoms are still present, they may include:
- Dyspnea
- Limited ability to perform physical activities
- Symptoms of heart failure (see above) or valve disease (see above)
Congenital heart disease in infants and children:
- Cyanosis (bluish discoloration of the skin, fingernails, lips)
- Rapid breathing and refusal to feed
- Minor weight gain
- Recurrent lung infections
- Inability to perform physical activities
Damage to the heart muscle (cardiomyopathy)
Many people with heart muscle damage experience no (or minor) symptoms and live full lives. In other people, symptoms may develop, progress, and worsen as heart function declines.
Symptoms can appear at any age and include:
- Chest pain or pressure (usually occurs with exercise or activity, but may also occur at rest or after eating)
- Symptoms of heart failure (see above)
- Swelling of the lower extremities
- Fatigue
- Fainting
- Palpitations (rocking in the chest due to abnormal heart rhythms)
- Some people also have arrhythmias. They may cause sudden death in a small number of patients with cardiomyopathy.
Pericarditis
Symptoms of pericarditis include:
- Chest pain that is different from angina (pain due to coronary heart disease). It can be acute and localized in the central part of the chest. The pain may radiate to the neck and in some cases to the arms and back. Symptoms worsen when lying down, taking deep breaths, coughing, or swallowing. Relief occurs when sitting upright
- Slight increase in temperature
- Accelerated heart rate
Since many of the symptoms of a particular heart disease are similar to each other, a visit to the doctor is of primary importance in order to make an accurate diagnosis and prescribe immediate treatment.
Diagnostics and research
When do risk factors turn into heart disease? The following tests are used to diagnose this type of disease.
The first step is to see a doctor. He may prescribe the following for you:
- ECG
- Chest X-ray
- Load test
- Tint table test (used to diagnose fainting)
- Echocardiogram
- Coronary angiogram (in other words, cardiac catheterization)
- Electrophysiological testing
- CT scan of the heart
- Myocardial biopsy
- MRI of the heart
- Pericardial puncture
Diagnostics
A comprehensive examination begins with a general practitioner or family doctor. The specialist conducts a physical examination and identifies the leading pathological syndrome, and if necessary, sends the patient for consultation with specialized specialists (pulmonologist, cardiologist). To establish a diagnosis, the results of instrumental and laboratory tests are necessary, of which the following are most often prescribed:
- X-ray of the OGK.
Radiation diagnostics helps to differentiate cardiac and pulmonary pathology. Damage to the respiratory system is manifested by focal infiltrates, rounded shadows, and increased vascular pattern. Signs of cardiac problems are changes in the size and configuration of the heart shadow, congestion in the lungs. - Electrocardiography.
An ECG evaluates the electrical activity of the myocardium. The cardiogram reveals a decrease in the voltage of the waves or their inversion, deviation of the heart axis, and signs of disturbances in the myocardial conduction system. Daily ECG monitoring and bicycle ergometer test are of great diagnostic value. - Echocardiography.
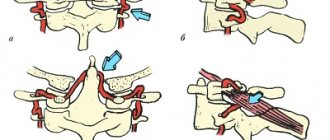
Ultrasound diagnostics shows structural and functional abnormalities in the activity of the heart. The method is necessary for diagnosing pericarditis (effusion in the heart sac), cardiomyopathy (expansion of cavities or thickening of the walls of the organ). EchoCG allows you to measure the contractile function of the left ventricular myocardium. - Invasive methods.
In case of pathological processes in the pericardium, a diagnostic puncture is performed for bacteriological and cytological examination of the exudate. In case of coronary artery disease, coronary angiography is performed to assess the extent of vascular damage. The functional state of the myocardium is determined by perfusion scintigraphy. - Laboratory diagnostics.
Analyzes are of auxiliary value. In case of cardiac pathology, an extended biochemical study is indicated with determination of the lipid spectrum and acute phase parameters, measurement of myocardial markers. Diagnosis of pulmonary diseases requires microscopy and sputum culture.
Echocardiography
Treatment
Help before diagnosis
Heaviness in the chest occurs when various organs and systems are affected, so self-medication at home is unacceptable and is fraught with the progression of the underlying disease and the development of complications. Patients experiencing chest discomfort are advised not to delay contacting a therapist. If squeezing pain is felt in the chest, the person experiences suffocation, febrile fever, and requires emergency medical attention.
Conservative therapy
Treatment measures are selected after identifying the causes of the condition. Heaviness in the chest does not require special symptomatic therapy and disappears after eliminating the underlying pathology. All patients are prescribed a gentle motor regimen, maximum limitation of stress and traumatic factors. Medicinal effects include drugs from the following pharmacological groups:
- Antianginal agents
. Used in combinations for long-term therapy of coronary heart disease. They are supplemented with antiplatelet agents to prevent myocardial infarction and thrombosis. Nitrates are recommended to relieve angina attacks. - Anti-inflammatory drugs
. Nonsteroidal anti-inflammatory drugs are indicated for myocarditis and pericarditis, acute respiratory diseases. They act pathogenetically and also relieve discomfort and pain. If nonsteroidal drugs are ineffective, corticosteroids are taken. - Antibiotics
. Antimicrobial drugs are prescribed for pneumonia, pleurisy, purulent bronchitis as etiotropic treatment. Penicillin antibiotics are effective for inflammatory lesions of the heart due to rheumatism. To treat tuberculosis, 3-4 specific drugs are combined. - Antiallergic drugs
. Leukotriene receptor antagonists and mast cell membrane stabilizers are used for basic therapy of bronchial asthma. Classic antihistamines are used as pathogenetic therapy for many inflammatory processes with an allergic component. - Metabolic drugs
. To improve the delivery and utilization of oxygen in the myocardium under conditions of ischemia, it is necessary to take cytoprotectors. Therapy is enhanced with ascorbic acid and B vitamins, which accelerate metabolic processes in the body.
Broken heart syndrome (Takotsubo syndrome)
This syndrome first became widely known in 2006 after a discussion of this topic at the European Congress of Cardiology in Barcelona. However, many practitioners and patients still remain poorly aware of its existence. In recent years, modern medicine has been paying more and more attention to studying its causes, which are still unclear.
As a rule, the typical symptoms of broken heart syndrome are pain in the heart and difficulty breathing, which is completely identical to the symptoms of acute myocardial infarction and determines the drama of the situation and its relevance.
It is currently believed that broken heart syndrome, or stress-induced cardiomyopathy (also known as reversible apical dyskinesia), is caused by strong emotions and is characterized by a transient dysfunction of the left ventricle of the heart, which manifests itself as changes in the electrocardiogram and in the blood, characteristic of myocardial infarction.
Stress-induced cardiomyopathy was first described in 1991 in Japan and was even called takotsubo after the name of the octopus trap used by Japanese fishermen, since in this syndrome the shape of the left ventricle becomes similar to it. With this disorder, the heart of patients, or rather its left ventricle, takes on an unusual spherical shape. It’s as if it’s being squeezed by an invisible hoop. This symptom helps to distinguish this disorder from a heart attack and make the correct diagnosis.
The provoking factor for this disease is severe stress and intense emotional experiences. Almost immediately after this, patients experience severe heart pain and serious breathing problems, which is usually diagnosed as myocardial infarction, since the symptoms and electrocardiogram data do not raise any doubts. Retrosternal pain with this syndrome is longer lasting than with myocardial infarction.
The mechanisms of this disease are not completely clear. Its clear connection with stress and difficult emotions makes doctors think that its cause lies in the effect of catecholamines - stress hormones. Other mechanisms have also been studied - spasm of the coronary arteries, impaired blood microcirculation in the heart and neurological causes, but none of them have yet been confirmed.
The problem in diagnosing this disorder is that both the blood tests and electrocardiogram for broken heart syndrome are almost identical to the results of diagnostic tests for myocardial infarction. It is possible to distinguish it only through coronary angiography, which in this case demonstrates completely healthy arteries of the heart.
As evidenced by the review materials (the results of 14 of the most current studies of this syndrome) recently published in the European Heart Journal, approximately 2% of myocardial infarction cases are stress-induced cardiomyopathy. In more than half of cases, this disorder is preceded by severe stress and catecholamine levels are elevated in 74% of patients. Compared to the normal concentration of these hormones, in these patients it can be increased tens of times. It is likely that many factors are important in the development of stress cardiomyopathy - vasospasm, microcirculatory insufficiency and pathological catecholamine response. When observing large groups of patients, it is indicated that in some of them Takotsubo cardiomyopathy developed after emotional stress or, in other cases, after previous physical stress (status asthmaticus or sudden illness). In approximately one third of patients there was no stress factor. Observation of large groups of patients in Europe showed that Takotsubo cardiomyopathy has a slightly higher incidence in winter. This may be due to two possible pathophysiological reasons: spasm of the small branches of the coronary arteries, which predominates in cold weather, and viral infections, such as Parvovirus B19, which are more common in the winter season.
There are reports that pathomorphological changes in this type of cardiomyopathy are represented by focal myocytolysis; no associated microbiological agents are detected. In some cases, infiltration by small mononuclear cells was detected; these pathological findings suggest that stress cardiomyopathy is a variant of inflammatory heart disease rather than a coronary pathology. There are also reports of histological damage to the myocardium without coronary heart disease.
More than 90% of cases of this disease occur in women during menopause. The reason for this is unclear, but there are several hypotheses: the greater sensitivity of women to the effects of stress hormones and problems in the blood vessels and heart muscle, provoked by low levels of female sex hormones.
In case of stress-induced cardiomyopathy, emergency hospitalization of the patient in a hospital is necessary. With this syndrome, heart failure often occurs, which disappears without a trace after a few days.
The prognosis of the disease is usually very good. Despite the initial serious condition of patients, almost all of them make a full recovery within a few days or weeks without any complications. The mortality rate is only 1.1%. In very rare cases, there may be severe complications: atrial fibrillation in 4.2% and cardiogenic shock in 1.5% of cases.