The human heart is an amazing organ, thanks to which the normal functioning of all organs and systems is possible. Contraction of the heart muscle is ensured by electrical impulses that pass through special pathways. If there are additional pathways for these impulses, certain changes occur that can be monitored using an electrocardiogram (ECG). With changes in the ventricular complex we are talking about the phenomenon of WPW (premature excitation of the ventricles). For minor disorders, characterized only by a change in the speed of impulses between the ventricles and the atrium, CLC syndrome is diagnosed.
What is the disease
Clerk-Levy-Christesco syndrome or CLC is a congenital pathology of the heart structure, one of the types of premature ventricular excitation syndrome. The anomaly is due to the presence of a James beam. Thanks to this bundle, the atrioventricular node is connected to one of the atria. This feature is accompanied by the transmission of a premature impulse to the ventricles.
Pathology can be diagnosed using an ECG. Often, CLC syndrome occurs accidentally in completely healthy people, and the patient does not have any symptoms. There are known cases of this disease being detected in children.
Even in the absence of symptoms, one should not assume that the pathology is harmless. Ventricular preexcitation syndrome can cause arrhythmia. The condition is accompanied by increased heart rate (sometimes over 200 beats per minute). This is especially felt in older people; young patients tolerate arrhythmia more easily.
Causes
Most cardiologists treat the syndrome as a congenital anomaly. It can appear at any age. More often in young people with mitral valve prolapse and cardiomyopathies.
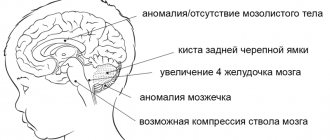
Premature arousal is combined with a rare congenital defect - Ebstein's anomaly
It includes:
- valve insufficiency between the right cavities of the heart;
- non-closed foramen ovale (between the atria);
- reduced cavity of the right ventricle.
The opinion is expressed that the embryonic stage of the formation of abnormal excitation pathways is associated with a general disorder of the development of connective tissue in the fetus.
The hereditary transmission of the syndrome has been proven based on the results of a family examination. Any disease or physical stress can be a provocation for manifestation.
Features of the pathology
Pre-excitation of the cardiac ventricles can be asymptomatic, in which case we are talking about the “pre-excitation phenomenon”. When signs of pathology appear in a patient, the disease is classified as “pre-excitation syndrome.”
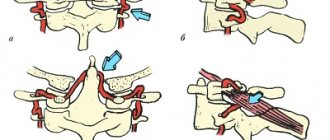
There are several types of disease:
- Breschenmash (atriofascicular) - here the right atrium is connected to the trunk of the His bundle;
- Maheima (nodoventricular) - in this case, the right side of the interventricular septum is connected to the atrioventricular node;
- Kent (atrioventricular) - here the atria and ventricles are connected bypassing the atrioventricular node;
- James (atrionodal) - impulses pass between the lower part of the atrioventricular and sinoatrial node.
Important! Sometimes there are several paths of abnormal conduction of impulses. The number of such patients is no more than 10% of all cases of the disease.
CLC syndrome is clearly monitored by performing an electrocardiogram
Is it possible to develop complications when PQ is shortened?
The phenomenon of shortened PQ cannot lead to any complications. Due to the fact that the manifestation of PQ syndrome is an attack of tachyarrhythmia, there will be corresponding complications. These include the occurrence of sudden cardiac death, fatal arrhythmias (ventricular fibrillation), thromboembolism of the cerebral and pulmonary arteries, the development of myocardial infarction, arrhythmogenic shock and acute heart failure. Of course, not every patient develops such complications, but everyone needs to remember them. Prevention of complications is timely seeking medical help, as well as timely surgery if indications for it are discovered by a doctor.
What Causes CLC?
In order to understand how CLC syndrome occurs, you should remember the anatomy. For the normal filling of the ventricles of the heart with blood and their contraction after contraction of the atria, there is a special filter located between them in the structure of the organ. This filter is called the atrioventricular node. When an impulse is transmitted to this node, the excitation passes slowly, after which it is transmitted to the ventricles. Thanks to this process, blood enters the aorta and pulmonary trunk.
With some congenital pathologies, a person may have bypass pathways for conducting cardiac impulses. Often the James beam and some other channels act in this way. In this case, the ECG shows minor deviations from the norm or severe disturbances, for example, with serious deformation of the ventricles. The syndrome of premature excitation of the ventricles in medical practice is called WPW.
Uninformative test
The test can be stopped due to severe shortness of breath, pain in the joints or legs until the patient reaches a submaximal heart rate when performing a low or medium power load (less than 150 watts), while clinical and electrocardiographic criteria for stopping the test are not noted. As a rule, patients in these cases do not achieve submaximal heart rate. The results of such tests are regarded as uninformative.
Exercise tolerance allows you to evaluate the effectiveness of treatment and rehabilitation measures.
During physical activity, blood pressure increases. At initial systolic blood pressure 160 mm Hg. Art. or more, the test should be abandoned if during the test the blood pressure rises to 230 mm Hg. Art., the test should be stopped. The test results are assessed according to generally accepted criteria; the type of circulatory response to stress is additionally assessed as hypertensive (inadequate increase in blood pressure at each level of load).
How does the disease progress?
Pathology can manifest itself at any age of the patient. For a long time, the disease can occur without obvious signs and symptoms. The CLC phenomenon is accompanied by a shortening of the PQ interval during an ECG. At the same time, the patient’s well-being is not impaired, the person leads a full-fledged lifestyle.
Signs of pathology often include attacks of tachycardia and some other manifestations
With CLC syndrome, many patients experience sudden attacks of strong heartbeat - paroxysmal tachycardia. The following symptoms are observed:
- the appearance of an attack of rapid heartbeat. Heart rate is up to 220 beats per minute. The onset of an attack is accompanied by a strong shock in the sternum or neck;
- dizziness;
- noise in ears;
- increased sweating;
- bloating;
- sometimes nausea occurs, accompanied by vomiting;
- copious amounts of urine at the beginning or end of an attack, sometimes involuntary urination.
Less commonly, the pathology is accompanied by atrial fibrillation, a rapid heartbeat of an irregular nature.
Why does short PQ syndrome occur?
As already indicated, the anatomical substrate of this syndrome in adults is a congenital feature, since additional conduction bundles are formed in the prenatal period
. People with such bundles differ from ordinary people only in that they have an additional tiny “thread” in the heart, which takes an active part in conducting the impulse. But how the heart behaves with this beam will be discovered as the person grows and matures. For example, in children, CLC syndrome may begin to manifest itself both in infancy and adolescence, that is, during the rapid growth of the body. Or it may not manifest itself at all, remaining only an electrocardiographic phenomenon throughout adult life until old age.
No one can name the reason why the syndrome begins to manifest itself as paroxysmal tachycardia. However, it is known that in patients with organic pathology of the myocardium (myocarditis, heart attack, hypertrophic cardiomyopathy, heart disease, etc.) attacks of tachycardia occur much more often and clinically occur with a more pronounced clinical picture and with a severe general condition of the patient.
But the provoking factors that can cause paroxysm can be listed:
- Physical activity that is significantly or not significantly greater than the patient’s usual physical activity,
- Psycho-emotional stress, stressful situation,
- Hypertensive crisis,
- Eating large amounts of food at one time, drinking very hot or very cold liquids,
- Visiting a bathhouse, sauna,
- Changes in external temperatures, for example, going out into severe frost from a very hot room,
- Increased intra-abdominal pressure, for example, during severe coughing, sneezing, defecation, pushing during childbirth, lifting heavy objects, etc.
First aid during an attack
Patients with CLC syndrome who frequently experience an attack of increased heart rate are advised to adhere to the following recommendations during an attack:
- Perform carotid sinus massage. Impact on this area between the division of the carotid artery into the external and external helps to normalize the heart rate.
- Gently press on the eyeballs.
- To alleviate the condition, you can lower your face into a container of cool water, holding your breath for 5 to 10 minutes.
- Take a deep breath, strain, hold your breath for a few seconds, exhale slowly.
- Sit down several times, tensing your whole body.
Important! If attacks occur frequently, do not delay visiting a doctor. Early diagnosis of pathology will help prevent complications and bring the disease under medical control.
Advantages of primary percutaneous coronary intervention over conventional surgery
The advantages of percutaneous coronary intervention (compared to bypass surgery) include:
- there is no need for general anesthesia, ventilation, switching to artificial circulation, or opening the sternum;
- no long recovery required;
- the effectiveness in normalizing blood flow is comparable - pain in the heart stops or appears less frequently;
- lower risk of cerebral blood flow disorders and postoperative pneumonia.
But with PCI, it is more common for the stent to become blocked or the site of expansion to narrow again, which requires another operation. This complication occurs in every fifth patient after 6-9 months.
Expert opinion
Alena Ariko
Expert in Cardiology
The disadvantages of any method of surgical improvement of coronary circulation include a symptomatic effect. This means that in this way it is possible to remove an obstacle to the movement of blood and relieve pain in the heart, but it cannot cure atherosclerosis. Therefore, patients require long-term drug prevention of re-clogging of the arteries, drugs that reduce blood viscosity, and lifestyle changes.
Diagnostics
The main method for diagnosing CLC syndrome is an electrocardiogram. An ECG can detect the following disorders:
- reduction of PQ intervals;
- D-wave in the presence of an ascending part of the R-wave with a simultaneous decrease in the Q-wave;
- the appearance of an extended QRS set;
- deviation of the CT segment and T-wave in the opposite direction from the D-wave.
Much attention is paid to the spatial vector electrocardiogram. Using the method, it is possible to accurately determine the location of additional conductive channels of the heart.
Timely diagnosis of CLC syndrome allows you to take the pathology under medical control and prevent its complications
For a more detailed study, magnetocardiography is used. The method allows you to give a complete assessment of the activity of the heart muscle. This happens thanks to equipment that records the magnetic components in the electromotive force of the heart.
Instrumental research methods such as electrophysiological examination of the heart (EPI), endocardial and epicardial mapping can provide an accurate assessment of the activity of the heart muscle.
A little history
Typical signs were first described in 1913. For a long period of time, the cause of the pathology was considered to be a type of blockade of the His bundle and its branches.
The joint report of L. Wolf, D. Parkinson and P. White in 1930 laid the foundation for research into the pathogenesis of conditions with increased excitability and conductivity of the nerve impulse.
After 2 years, the theory of additional vascular bundles was presented, which were found on histological sections only in 1942 by F. Wood.
Active research on the electrophysiology of the heart muscle has made it possible to finally establish the localization of additional tracts and discover their diversity.
Features of pathology treatment
Patients diagnosed with asymptomatic pathology do not require special treatment. Attention is paid to patients who have a history of sudden death in their family. People involved in heavy physical work, athletes, divers, and pilots are also at risk.
If a patient experiences paroxysms of supraventricular tachycardia, therapy consists of prescribing medications to relieve the attack. In this case, the nature of the heart rhythm disturbance and the presence of concomitant diseases of the cardiovascular system must be taken into account.
To get rid of orthodromic reciprocal supraventricular tachycardia, blockades are used aimed at inhibiting the conduction of impulses in the atrioventricular node.
Drug therapy includes the following drugs:
- Adenosine;
- Verapamil.
Often, to reduce the manifestation of pathology, beta-blockers are prescribed, which have the ability to dilate the bronchi, arteries and veins. Drugs in this group activate the production of glycogenolysis by the liver and skeletal muscles and stimulate insulin secretion.
Amiodarone is a medication often prescribed for CLC syndrome.
In the absence of the desired therapeutic result, doctors use Novocainamide, which helps block impulses passing through the accessory atrioventricular canal. The medicine is relatively safe and has a good effect in the treatment of many cardiac pathologies.
In addition to those described above, the following medications are used:
- Amiodarone;
- Sotalol;
- Propafenone;
- Flecainide.
Important! The use of medications is permitted strictly as prescribed by the attending physician. Many of them have serious contraindications.
Non-drug treatment methods include transthoracic depolarization and atrial pacing. Surgical treatment of accessory pathways is used in special cases when conservative therapy does not produce a positive effect. The operation is performed using the open method in emergency cases when there is a serious threat to the health and life of the patient. The method involves destroying additional pathways of the heart.
A positive prognosis for patients with impaired conduction of cardiac impulses is possible with strict adherence to the doctor’s recommendations
Examination methods
To determine the presence or absence of additional bundles in the heart muscle, the most accessible method is electrocardiography. For an unstable type of syndrome, Holter monitoring is used, followed by interpretation.
In cardiac centers and specialized departments, the method of spatial vector electrocardiography is used. It allows you to identify additional pathways with high accuracy.
Magnetocardiography records in detail electrical impulses from different parts of the myocardium, helping to establish the exact localization of abnormal impulses and tracts.
The most reliable are electrophysiological methods performed during cardiac surgery. They are associated with the installation of electrodes inside cavities and in the epicardium.