1.Cysts of the brain
Brain cysts
– common benign neoplasms, which are a rounded cavity filled with liquid contents. The reasons why cysts occur can be very diverse.
A considerable part of cysts are congenital, some are formed as a result of previous injuries, sometimes even in the distant past. Such brain tumors can also be the result of inflammatory processes, hemorrhages, circulatory disorders and dystrophic-degenerative changes in the brain.
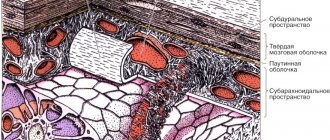
Cysts are localized between the membranes of the brain (arachnoid) and directly in the tissues of the brain, in its depths.
A must read! Help with treatment and hospitalization!
"Scary" names
What is a cyst? A cyst (its other name is “cerebrospinal fluid cyst”) is a cavity filled with liquid, having a capsule that isolates it from other liquor-containing spaces.
Most often, parents of children who have been diagnosed with a retrocerebellar cyst
. And although this phrase frightens and even makes parents panic, it must be said that with these words radiologists describe a variant of the norm. Most often, this is not a cyst at all (that is, not an isolated cavity filled with fluid), and it does not require surgical treatment.
Children under two years of age diagnosed with a retrocerebellar cyst should be shown to a neurosurgeon to avoid the development of hydrocephalus.
Another normal variant is a pineal gland cyst.
. Perhaps the most common incidental finding on MRI. Does not require surgical treatment.
Epidermoid or dermoid cyst
– this is not a real cyst. It is filled not with liquid, but with skin appendages - follicles, sebaceous glands, hair, cartilage tissue, etc. In its structure, it is more similar to a tumor and requires the same treatment as for a tumor - removal.
Porencephalic cyst
usually occurs in the place where part of the brain has died as a result of hypoxia or hemorrhage; this place is filled with fluid. In itself, such a cyst does not interfere with development and does not require mandatory surgical treatment.
Pseudocyst
- looks like a cyst, but not a cyst, a cavity that is not limited by anything, it has communication with other parts of the skull. Does not require surgical treatment.
Septum pellucida cyst
in the vast majority of cases it is a variant of the norm, but if it is large in size, it can lead to impaired cerebrospinal fluid circulation, which requires surgical treatment.
For children in whom the cerebrospinal fluid cyst rapidly enlarges, causes increased intracranial pressure, neurological symptoms or seizures, surgical treatment is indicated.
If your child has a photo taken and a cyst is found, don’t panic! Having received a description of the x-ray image, first of all, pay attention to the conclusion. If the report says: “There are no pathological abnormalities,” most likely you will not need any surgical intervention. Even if you see the word “cyst” somewhere, most likely the radiologist needed it to describe a normal condition. Just in case, check with him whether you need a consultation with a neurosurgeon.
2.Types of brain cysts
Cysts can be formed by various types of cellular structures, and depending on this they are divided into the following types:
- arachnoid;
- pineal;
- colloidal;
- dermoid;
- epidermoid (cholesteatomas).
With the exception of arachnoid cysts, which were already mentioned above, all others are classified as intracerebral.
Epidermoid and dermoid cysts
consist of epithelial cells that, due to certain processes, ended up in the wrong place, but got inside other tissue masses. This may be a consequence of embryogenesis disorders (congenital cysts), or the result of injuries when epidermal cells enter tissues located deep in the brain (acquired cysts).
Dermoid cysts
characterized by the presence of various dermal inclusions - fat and sweat glands, hair follicles, etc.
Most of these cysts are found in the following parts of the brain:
- pontocerebellar ganglion (MCG);
- chiasmal-sellar region (CHS);
- ventricular cavity;
- cerebellum;
- brain stem.
Visit our Neurosurgery page
Arachnoid cysts (AC) are congenital, predominantly extracerebral formations, the walls of which are the arachnoid membrane, and the contents are cerebrospinal fluid (CSF). In children, arachnoid cysts, according to various sources, account for about 10% of all volumetric formations of the brain and in 7.4% of cases are found in children with hydrocephalus. The division of arachnoid cysts into two large groups is pathogenetically justified: 1. Cysts of the cerebral hemispheres: - lateral (Sylvian) fissure; - convexital surface of the brain; - parasagittal interhemispheric fissures).
2. Mid-basal cysts: - suprasellar; - intrasellar; - tentorial notch; — posterior cranial fossa (upper and lower retrocerebellar, cysts of the cerebellopontine angle).
The group of mid-basal cysts can also include mid-stem cysts (retrocerebellar), since they are identical in their pathogenetic mechanisms.
The most common locations of arachnoid cysts are the Sylvian fissure (lateral fissure), interhemispheric fissure and suprasellar cistern. However, they can occur anywhere where the arachnoid membrane is located. Morphologically, the inner and outer walls of the cyst consist of thin layers of arachnoid cells and are often connected to the unchanged arachnoid membrane. Cysts can be congenital (primary) or acquired (secondary). Unless there is a history of trauma or inflammation, the cysts are considered congenital. Currently, there are several theories about the occurrence of arachnoid cysts. The first is the “intraarachnoid cyst theory,” in which cyst formation is the result of splitting and duplication of the arachnoid membrane. The second is the “subarachnoid cyst theory,” which explains the occurrence of middle cranial fossa cysts as a result of agenesis of the temporal lobe. The formation of arachnoid cysts occurs at the stages of embryogenesis during the formation of the membranes of the brain. Under pathological conditions, mainly with subarachnoid hemorrhage caused by hypoxia, infection, intoxication, etc., it becomes possible to form microcavities in the arachnoid membrane, which subsequently increase in size, turning into arachnoid cysts.
Most arachnoid cysts remain undiagnosed during life. The patient’s condition can remain compensated for a very long time, and the course of the disease is asymptomatic. The first manifestations can be noticed in adulthood. The timing of referral of children with congenital arachnoid cysts to neurosurgical departments, as a rule, depends on the location and size of the cysts. It is known that cysts of the tentorial notch cause more severe neurological symptoms. Common symptoms, which, however, manifest themselves to varying degrees in cysts of different localizations, include: - volumetric effect on the surrounding structures of the brain; — presence of an asymptomatic period; - no signs of inflammation in the membranes of the brain.
Positive meningeal symptoms are usually observed only when the disease is complicated by subarachnoid or intracystic hemorrhage. Hyperthermia and inflammatory changes in the blood are not typical for arachnoid cysts. — the severity of compensatory mechanisms and the absence of gross neurological manifestations in the presence of significant morphological changes, which is especially typical for hemispheric cysts. The clinical picture of arachnoid cysts is determined in most cases by three symptom complexes: hypertensive-hydrocephalic, focal neurological symptoms and damage to the brain stem. Signs of damage to the brainstem only in cysts of the cerebral hemispheres should be regarded as dislocation; in cysts of mid-basal localization, they can also be caused by the direct effect of the cyst on the brainstem. The uniqueness of the clinical picture of cysts in individual locations is determined by the duration of the asymptomatic period, the severity and characteristic coloring of the three leading neurological syndromes. It is believed that children with intracranial arachnoid cysts that have a mass effect should be operated on, because the volumetric effect of the cyst can lead to a delay in the development and formation of the brain, and rupture of the cyst is usually accompanied by intracystic and subdural bleeding. These complications justify the risk of surgical intervention. A direct indication for surgical treatment is progressive hydrocephalus that occurs when a cyst blocks the cerebrospinal fluid circulation pathways.
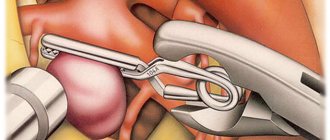
Currently, effective methods of surgical treatment of arachnoid cysts, including in the Department of Neurosurgery of the Russian Children's Clinical Hospital, are: perforation of the walls of the cyst with excision of its walls using the microsurgical method (through a small trefination window), as well as the neuroendoscopic method. CSF shunt operations are used extremely rarely.
3. Symptoms of a brain cyst
Small cysts are asymptomatic and can be accidentally detected during examination. When the tumor reaches a large size, the symptoms that appear depend on its location. Among the most characteristic symptoms are:
- headache, dizziness;
- feeling of fullness in the head;
- auditory and visual impairments;
- convulsions, paralysis of limbs;
- epileptic seizures;
- impaired coordination of movements;
- fainting, hallucinations;
- sleep disorders.
About our clinic Chistye Prudy metro station Medintercom page!
2. Symptoms of a tumor cyst
Clinically, these neoplasms begin to manifest themselves when pressure comes on the surrounding brain tissue due to the increased size of the cyst. These symptoms are characteristic not only of cysts, but also of other types of benign tumors:
- auditory, visual and olfactory disorders;
- movement coordination disorders;
- inability to concentrate;
- difficulties with memory and speech;
- dizziness, nausea, vomiting;
- partial or complete paresis of the facial muscles;
- loss of sensation in the limbs, convulsions.
Visit our Neurosurgery page
4.Basic treatment methods
As a rule, cysts that do not show a tendency to grow do not require treatment at all. Otherwise, treatment of neoplasms is carried out surgically. It could be:
- transcranial surgery, which provides high efficiency of cystectomy, but is traumatic for the patient;
- shunting the cyst to evacuate the liquid contents, after which its walls collapse;
- gentle endoscopic surgery using special equipment.
Treatment
In neurology departments, when treating colloid cysts of the third ventricle, doctors adhere to the following tactics: small formations without symptoms of the disease are not treated, the patient is sent for an annual MRI or CT scan, which evaluates the size of the formation and its tendency to grow.
For large tumors with clinical manifestations or with progressive enlargement of the cyst, consultation with a neurosurgeon is indicated to decide on surgical treatment. During surgery, the cyst is completely removed, the cerebrospinal fluid ducts are cleared, and thereby the syndrome of increased intracranial pressure is eliminated. The following surgical techniques are used: craniotomy and endoscopic removal. Craniotomy is an opening of the skull and open brain surgery; it allows you to completely remove the tumor, examine the cavity of the third ventricle, and restore the cerebrospinal fluid tract. Its disadvantages are greater trauma and cosmetic defects after surgery. Endoscopic removal of a colloid cyst is carried out through a small hole in the bones of the skull using a special apparatus, which allows both to examine the cavity of the third ventricle and to remove the tumor. After surgery to remove the cystic formation and restore the flow of cerebrospinal fluid using modern methods, an almost complete recovery of patients is noted. In rare cases, the pathological process recurs, and then a repeat operation becomes necessary. To prevent the onset of colloid cyst growth in adults, it is necessary to lead a healthy lifestyle.
4. Stereotactic aspiration of tumor cysts
The essence of this gentle technique is to insert a small-diameter probe into the cyst through a small hole in the skull in order to pump out excess liquid contents from its cavity. This procedure occurs either using the neuronavigation
, or using a special
navigation frame
. In both cases, the operating neurosurgeon has the opportunity to extremely accurately hit the desired area with the instrument. When using neuronavigation, a three-dimensional image of the surgical field is displayed on the monitor, which increases the efficiency of the surgeon’s actions. The manipulation is carried out with high precision, taking into account the anatomical and physiological characteristics of the patient and does not cause damage to surrounding tissues. A disadvantage of stereotactic aspiration can be considered the lack of opportunity for the surgeon to conduct a thorough inspection of the operating area and control the risk of possible bleeding. But this does not at all detract from the advantages of minimally invasive surgery compared to traditional surgery.
MRI with contrast
In most cases, magnetic resonance imaging of the brain is performed with contrast, especially if any neoplasm is suspected. This makes it possible to examine the tumor in detail and distinguish a benign tumor from a malignant one.
The contrast agent clearly highlights the vessels, which allows you to see any tissue pathologies. Don't worry, contrast agents are safe for the human body. Most patients tolerate this procedure well. You must first consult a doctor and exclude all possible contraindications.
Atheroma
21710 December 23
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Atheroma: causes, symptoms, diagnosis and treatment methods.
Definition
Atheroma is a cyst (pathological cavity) of the sebaceous gland, resulting from difficulty or complete cessation of the outflow of secretion (sebum) from the gland. The sebaceous glands are exocrine glands and are located on almost all parts of the skin, with the exception of the palms, soles and back of the feet. The secretion they produce is part of the water-lipid mantle of the skin. If the gland duct becomes clogged, then the secretion begins to accumulate in it, stretches it to form a cavity lined with the epidermis and containing secretion products of the sebaceous gland, cholesterol crystals, keratinized epidermal cells and detritus (decomposition products) - this is atheroma.
Atheromas occur in 5-10% of the population, mainly forming at the age of 20-30 years, with the same frequency in men and women.
Causes of atheroma
Atheroma occurs as a result of disruption of the sebaceous glands, which is manifested by increased production of sebum and blockage of the duct. A number of factors predispose to this: increased sweating, poor hygiene, narrow ducts of the sebaceous glands, individually determined high viscosity of sebum, chronic trauma to the skin, hormonal disorders, frostbite and burns. Hereditary factors also influence the development of atheroma.
The use of antiperspirants can contribute to blockage of the duct.
Classification of the disease
There are true and false cysts. True sebaceous cysts are a hereditary disease and are extremely rare. They develop as a result of a genetic defect that affects the formation of the gland. Typically, such cysts occur in newborns and are small in size. False cysts are actually atheromas that arise due to a violation of the outflow of sebaceous gland secretions.
Symptoms of atheroma
Atheromas most often occur in areas of the body where there are many sebaceous glands, for example, on the scalp, face, neck, and in the interscapular space.
Atheroma is a mobile formation of a round or slightly elongated shape, dense or elastic consistency, covered with unchanged skin. A characteristic sign of atheroma, which distinguishes it from other formations, is the presence of a point retraction of the skin (crater) in the area of the excretory duct of the gland and the adhesion of the skin to the cyst shell in the same place. Sometimes there is a hole in the middle of the atheroma through which its contents are released - cheesy masses with an unpleasant odor.
The size of atheroma can vary from a pea to a chicken egg and even more, reaching 10 cm. Atheroma always rises above the skin level, grows slowly, and is usually painless.
Diagnosis of atheroma
To make a diagnosis, the doctor performs a clinical examination; in some cases, an ultrasound examination may be required.
Prevention
An acquired cyst most often becomes a consequence of developing inflammatory, vascular, infectious and post-traumatic processes. Therefore, it is absolutely obvious that only correct and timely treatment of any pathologies, including resorption and neuroprotective therapy, can serve as a preventive measure for the development of formations in the brain.
The only measure to prevent congenital cysts is to protect the woman and fetus from exposure to provoking factors. Equally important are correct management of pregnancy and delivery.
What is an ovarian cyst
Cysts in the ovaries often occur in women against the background of a seemingly normal cycle. Since it is in the testicles that the follicle is formed, from which the egg is formed, which ruptures the follicular membrane and is released into the uterine cavity during ovulation, cysts are formed here. This happens when the follicle, while maturing, does not rupture. As a result, it fills with liquid. The second type of cyst is a cystic formation of the corpus luteum. This occurs when the egg has left the follicular membrane, but the corpus luteum has filled with fluid.
The reasons for the formation of cysts in the ovaries can be:
- changes in body weight due to hormonal fluctuations or unhealthy eating behavior;
- constant stress;
- excessive physical activity.
Cysts of this kind do not require medical intervention and go away on their own with a cycle. Prescribing hormonal therapy in this case is also not justified, since changes in hormonal levels can negatively affect subsequent cycles and ovulation.
If a functional ovarian cyst is detected, it is necessary to abstain from sexual activity and not lift any heavy objects, so as not to provoke a rupture. In addition, you should not engage in sports, especially if it is running or acrobatics.
Surgical intervention is justified only if the cyst does not go away on its own within 5-6 months, as well as in the case of its internal rupture and release of fluid into the uterine cavity.