© Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
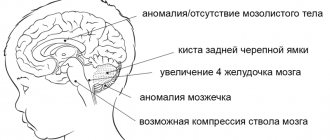
A subependymal cyst is a structural change in the medulla in the area of the walls of the lateral ventricles, which has the form of a hollow formation with liquid contents. Such cysts can be combined with choroid plexus cysts, cause severe neurological symptoms or be asymptomatic.
Typically, cystic changes in the brain are congenital in nature, formed during intrauterine development or during childbirth, so they are found in the practice of neonatologists and pediatricians. Representing a benign formation, they are nevertheless capable of significantly affecting the psychomotor development of the baby, and therefore require timely diagnosis and follow-up.
Parents faced with the problem of a subependymal cyst often do not know how to behave with their child and what to do, and pediatric neurologists are in no hurry to reassure, especially in the case of severe hypoxic changes or intrauterine infection. This is due, first of all, to the variability of the course of the pathology, when it is impossible to predict anything in advance.
However, even if the doctor does not provide comprehensive information, and the baby is discharged from the maternity hospital home under the supervision of a local pediatrician and neurologist, there is no need to panic. In some cases, a subependymal cyst resolves on its own during the first year of life or remains forever without having a significant impact on the child’s development.
Why do subependymal cysts appear?
The occurrence of a subependial cyst of the brain is usually associated with factors such as:
- Infection with herpes, cytomegaly, rubella, etc. viruses during intrauterine development;
- Birth injuries with hemorrhage or necrosis of the subependymal germinal matrix;
- Severe hypoxia during pregnancy or childbirth with severe circulatory disorders in the brain, mainly around the lateral ventricles.
One of the important circumstances contributing to the appearance of a subependymal cyst of the brain is infection with herpes and cytomegaly. Every tenth baby who is exposed to the virus in utero or at the time of birth has certain manifestations of the nervous system. Generalized infection is accompanied by high mortality, reaching 90%, and at least half of surviving infants have profound psychoneurological problems.
The appearance of subependymal cavities during a viral infection is associated with the direct damaging effect of the “aggressor” on the so-called germinal matrix - the nervous tissue around the lateral ventricles. The virus provokes neuronal necrosis, which resolves over the next month with the formation of cavities. The resorption of necrotic masses occurs the slower, the larger the source of damage, and in severe cases it can take several months.
The detection of formed cysts in newborn babies indicates episodes of ischemia and necrosis from the action of the virus during embryonic development, usually at the end of the second and beginning of the third trimester of gestation.
Another possible cause of the appearance of a subependymal cyst is considered to be hypoxic-ischemic damage with leukomalacia, that is, softening and necrosis, the outcome of which will be the appearance of a cavity. Premature babies and those born with very low weight (one and a half to two kilograms) are especially susceptible to this pathology.
Lack of oxygen during the intrauterine formation of the brain or during childbirth has a very detrimental effect on nerve cells, especially in the tissue surrounding the lateral ventricles due to insufficient blood supply to this area due to the small development of collaterals. Free radical processes, the release of large amounts of acidic metabolic products, and local thrombus formation lead to necrotization and cyst formation around the ventricles.
Subependymal cysts formed after leukomalacia are often multiple, 2-3 mm in diameter, surrounded by denser nervous tissue due to the proliferation of microglia. As they subside during the first months of life, irreversible atrophic changes and the formation of neuroglial nodules occur in the baby’s brain.
Birth injuries and cerebral hemorrhages against the background of hemodynamic and coagulation disorders can also lead to cyst formation. Hematomas can form in any part of the brain, including under the ependyma of the ventricles and in the ventricles themselves. Resorption of the spilled blood ends with the appearance of a cavity, which, if appropriately localized, will be called a subependymal cyst.
Concept
All cysts have a similar structure - they are cavities in which fluid is located - and can form in different parts of the body.
A subependymal cyst forms in the brain under the influence of one or more unfavorable factors.
Small cystic formations do not cause significant negative consequences and resolve on their own over time , but large cysts that are poorly located require increased medical supervision.
What are the consequences of cephalohematoma in newborns? Find out about this from our article.
Manifestations of subependymal cysts
Subependymal cystic cavities, detected by ultrasound, have clear contours, spherical or slit-like shape, their sizes range from a few millimeters to a centimeter or more. Sometimes cystic transformation resembles a honeycomb due to the multiplicity of lesions. Experts associate the different structures of cysts with their detection at different stages of pathological development, when some of the cavities are relatively fresh, while others are already undergoing the process of resorption and “healing.”
subependymal cyst on ultrasound
Subependymal cysts can be located symmetrically, only on the right or left, in the area of the middle sections or horns of the lateral ventricles. The stronger the hypoxia experienced, the greater the volume of brain tissue that will be damaged. If the baby has a hemorrhage, then a single cavity filled with clear cerebrospinal fluid may subsequently be detected.
During the first year of life, the subependymal cyst shows a tendency to decrease in size and even completely disappear, while it is possible to both maintain the normal size of the sections of the lateral ventricles and increase the volume of their bodies or anterior horns. In rare cases, it is possible to observe the growth of a cystic formation, which can provoke compression of surrounding tissues and disruption of liquor dynamics.
The symptoms of a subependymal cyst on the left or right are variable, they can be either absent or quite severe, which is determined by the size, number and location of the cavities, as well as their combination with other lesions of the brain tissue.
Small cysts or a single small cavity may not manifest themselves in any way, not change the baby’s development and not cause any concern. In most cases this is what happens. Concerned parents can read a variety of information, usually from Internet resources, in which the symptoms will include both visual and motor disturbances, however, the small cavities located under the ependyma (lining) of the ventricles are unlikely to somehow affect the corresponding brain structures, therefore, such judgments should be treated critically, without panicking and trusting only the opinion of a pediatric neurologist.
With large, multiple or growing subependymal cysts that appear against the background of large hematomas, dysfunction of the corresponding parts of the nervous tissue with neurological symptoms is possible, but such events develop extremely rarely and are usually based on a combined lesion of the central nervous system. Possible signs of trouble are:
- Sleep disorders, causeless crying, anxiety;
- Anxiety, hyperexcitability of the baby or, conversely, lethargy and lethargy;
- Tendency to muscle hypertonicity, in severe cases - hypotension and hyporeflexia;
- Poor weight gain, weak sucking reflex;
- Visual and hearing impairments;
- Tremor of arms, legs, chin;
- Severe and frequent regurgitation;
- Pulsation and bulging of the fontanel due to intracranial hypertension;
- Convulsive syndrome.
These symptoms can be expressed to varying degrees. As cysts are reabsorbed, they often weaken and even disappear by the end of the first year of life, but in severe cases, delays in mental and motor development, stunted growth of the child, and problems with speech and learning become noticeable.
A subependymal cyst, which appears against the background of leukomalacia of the periventricular nervous tissue, can have cerebral palsy, convulsive syndrome, and mental retardation as the most severe consequences.
Problems with child development are most often recorded with brain damage combined with other signs of a generalized infection. In these cases, malformations of other organs, viral pneumonia and even sepsis are often diagnosed after childbirth.
The prognosis when subependymal cysts are detected is often uncertain, which is why doctors do not rush to premature conclusions. Both normal brain development and serious neurological deficits with combined pathology are possible. Children often exhibit polymorphic symptoms, ranging from severe depression of the central nervous system to hyperexcitability.
In some cases, normally developing infants exhibit some signs of immaturity of the nervous system in the form of transient and short-term tremor of the chin or limbs, restlessness, and regurgitation. It is difficult to associate these symptoms with small subependymal cysts, but children are under the close attention of specialists.
Consequences and prognosis of the disease
The formation of small cysts does not have a serious impact on the quality of life, psychological and mental development of the child. Problems appear if it increases in volume. This may be affected by the presence of infections and hypoxia.
As the cyst enlarges, symptoms such as irritability, bronchopulmonary diseases, heart defects, developmental delays, and anemia begin to appear.
The first year of a child’s development does not show any serious deviations. Parents begin to notice violations at 2-3 years of age. The child has hyperexcitability, delayed speech development, and poor coordination. More serious manifestations include coma and death.
Diagnostics
Diagnosis of a subependymal cyst in a newborn baby is made using ultrasound in the first days after birth. An open large fontanelle allows you to clearly visualize structural changes without harming the baby. After the fontanel is closed, an MRI is prescribed. Examinations are carried out regularly throughout the first year of life to monitor the dynamics of cysts.
Ultrasound of the brain
If a herpetic or cytomegalovirus infection is present or suspected, additional tests are performed to verify the diagnosis and decide on further treatment tactics - immunological diagnostics.
The complexity and high cost of immunological research do not allow them to be carried out even in large cities, and in small towns they are completely unavailable. In addition, an immunologically confirmed diagnosis of a viral infection does not provide information about the nature of brain damage, so it is most rational to perform echoencephalography, which shows the degree and nature of brain damage, but at the same time is safe for newborns.
Qualitative approach to therapy
Treatment of a cerebral cyst is aimed at preventing its growth. To do this, you need to find and eliminate the main cause that provokes oxygen starvation. During certain life stages of a child's growth, medical care will vary.
First aid
After birth, a neonatologist performs resuscitation care.
Removes fluid from the respiratory tract, stimulates artificial respiration; in severe cases, an oxygen mask is used to supply pure oxygen.
The first three days after birth...
A neurologist conducts a daily examination and prescribes a restorative course of medication and rehabilitation therapy. Massage, physical therapy and sedatives are prescribed.
In childhood, the doctor observes the dynamics of the child’s development rate.
Medicines are used to stimulate speech functions and normalize the psycho-emotional state. At this stage, you may need the help of specialists such as a speech therapist and a psychologist.
...and beyond
When a child reaches adolescence, vitamin medications are prescribed to stimulate brain function and normalize metabolism. It is also necessary to take hormone replacement medications.
All physiotherapeutic and medicinal methods are prescribed only after the results of the examination and identification of deviations in the child’s development.
Causes of cerebral pseudocysts
Scientists were unable to establish the etiological factors of cystic intracerebral cavities. Verification of provoking mechanisms of development in children has been established by practice. Pathology is most often formed due to problems passing through the birth canal. Prenatal ultrasound does not indicate pseudocysts.
True cysts can be detected up to 28 weeks. Then they regress on their own.
Problems arise in children due to cerebral hemorrhage, hypoxic conditions, and cerebral circulatory pathology.
Subepindymal pseudocysts in newborns and infants are associated with the birth process, but are not congenital. Complications arise due to concomitant hemorrhages.
Pseudocyst of the choroid plexus of the right lateral ventricle
The development of cystic cavities of the choroid plexus is observed at 13-18 weeks. By this time, a mesh structure is formed inside the choroid. After filling the formation with liquid, cavities with the presence of cerebrospinal fluid are visible on ultrasound. By the twenty-eighth week of pregnancy, the cysts disappear on their own. Pseudoformations of the right ventricular plexus after birth are found during complicated pregnancy:
- Hypoxia of fetal brain tissue;
- Infections (herpes, chlamydia, cryptococcal).
The choroid plexuses in the fetus form in the sixth week. In the absence of nerve cells, fluid formation abnormalities may occur. Drops of cerebrospinal fluid after contact with the structures of the choroid plexuses lead to the formation of additional cystic cavities.
Pseudoformations of the left and right sides are equally likely to develop. Most of it resolves by 28 weeks. The pathology is formed at the beginning of intensive fetal development, when there are temporary disturbances in embryogenesis. By birth, brain function is normalized. If the formations persist after birth, the nosology usually disappears within a year.
The danger comes from the combination of pseudocysts with other brain changes:
- Diaphragmatic hernia;
- Trisomy 18 chromosomes;
- Diaphragmatic hematoma;
- Micrognathia;
- Omphalocele;
- Hydrocephalus;
- Cystic hygroma;
- Neural tube defects;
- Hammer feet.
In the presence of combined disorders, amniocentesis is performed - this is the removal of amniotic fluid for subsequent study of chromosomes. Pseudocysts with additional stigmas of disembryogenesis develop in a number of hereditary diseases (Down, Edward).
Amniocentesis is considered safe for the child, but the procedure is invasive, so it is performed according to indications.
A comprehensive examination involves the use of additional neuroimaging methods:
- Neurosonography;
- Magnetic resonance imaging (MRI);
- Computed tomography (CT).
Ultrasound examination is possible in full-term infants, when the fontanelles are covered with thin bone tissue. In newborns, the lumens are open to ultrasound rays. MR and CT angiography methods are used to examine cerebral vessels after intravenous administration of a contrast agent.