Hypertension is a pathology accompanied by a persistent increase in blood pressure above 130/90. It entails changes in the functioning of internal organs, as well as disruption of a person’s well-being. This disease is progressive.
Causes of hypertension
The main reason is a decrease in the lumen of small vessels, impeding blood flow. The pressure on the walls of blood vessels increases, and blood pressure increases, because the heart muscle needs more effort to push blood through the bloodstream.
The following risk factors for developing the disease are identified:
- the age of the person (women over 65 years old, men over 55 years old);
- cholesterol level (above 6.5 mmol/liter);
- heredity (presence of cardiovascular diseases in relatives);
- smoking;
- obesity;
- diabetes;
- sedentary lifestyle of an elderly person.
Symptoms of hypertension
Common symptoms of hypertension are:
- tinnitus;
- headache;
- facial redness;
- dizziness;
- cardiopalmus;
- memory impairment;
- profuse sweating;
- attacks of pulsation in the head;
- chills;
- puffiness around the eyes;
- attacks of irritability, anxiety;
- “flies” flashing before the eyes;
- constant fatigue, decreased performance, a feeling of systematic lack of sleep;
- numbness and swelling of the toes and hands.
The increase in blood pressure occurs intermittently and goes away after calming or resting. If you do not begin to correct the disease, the symptoms progress and become permanent, after which they are joined by the following:
- impaired coordination of movements;
- blurred vision;
- decreased intelligence and memory;
- changes in gait;
- weakness in arms or legs;
- decreased overall sensitivity;
- problems with the functioning of blood vessels, kidneys, and brain.
Hypertension, in addition to the main symptoms (high blood pressure, etc.), has a number of clinical signs that are individual at different stages of the disease in an elderly person.
Symptoms of stage 1 hypertension include:
- low rises in blood pressure (up to 160-180 at 95-105 mmHg);
- episodes of tinnitus, headaches, difficulty concentrating and sleeping;
- fluctuations in blood pressure (it does not return to normal on its own);
- nosebleeds.
If hypertension is suspected, the doctor does not detect at this stage any abnormalities in kidney function or changes during ECG and ultrasound of the heart.
Symptoms of stage 2 hypertension:
- a steady increase in blood pressure (up to 180-200 per 105-115 mm Hg);
- headache;
- fundus changes;
- pain in the heart area;
- periodic occurrence of hypertensive crises;
- signs of brain damage with strokes and ischemia;
- kidney damage;
- signs of damage to the heart muscle in the form of ischemia and hypertrophy;
In the third stage of the disease, the following symptoms are observed:
- high blood pressure (220-230 per 130-150 mmHg);
- circulatory failure;
- signs of encephalopathy;
- microinfarctions, angina pectoris, microstrokes, arrhythmias;
- eye lesions with severe angiopathy and blindness;
- decreased filtration rate and blood flow of the kidneys.
A decrease in blood pressure to a normal level does not occur on its own (only under the influence of strong drugs).
Diagnostics
The diagnosis of hypertension is based on monitoring blood pressure at home (during exercise and at rest). You can monitor your blood pressure using automatic or manual pressure gauges.
When diagnosing hypertension in the clinic, the following is carried out:
- detailed questioning of the patient, accurate recording of all risk factors, the doctor identifies predispositions to the disease;
- clinical examination (the doctor measures the person’s pulse and blood pressure);
- daily monitoring of blood pressure (prescribed if necessary);
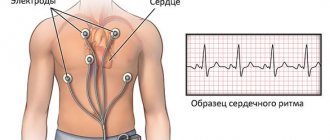
- conducting Holter monitoring, performing an electrocardiogram;
- determining the stability of blood pressure levels, minimum and maximum numbers, the effects of medications, etc.;
- consultations with a nephrologist, neurologist, endocrinologist;
- laboratory diagnostics (general analysis and biochemistry of blood and urine, levels of sodium and calcium, phosphates and uric acid, plasma potassium, etc.);
- chest x-ray;
- Ultrasound of the kidneys, heart;
- diagnostics using bicycle ergometry, load tests (if necessary).
An excursion into the anatomy and physiology of the cardiovascular system
The heart is the main pump that pumps blood into the vessels. She runs through the vessels to every organ of our body to water and feed it. Every living thing must drink and eat, on time and in sufficient quantity . Otherwise it dies.
There are four chambers inside the heart: two atria and two ventricles. They are separated from each other by partitions and valves.
The heart either contracts, and this is called systole, or relaxes, and this is called diastole.
During systole, the volume of the chambers decreases and blood is released into the vessels.
Systolic pressure is the pressure that blood exerts on the walls of blood vessels during heart contraction.
During diastole, the chambers expand again and fill with blood.
Diastolic pressure is the pressure that blood exerts on the walls of blood vessels when the heart relaxes.
The heart valves open when necessary, and close when necessary, so that blood flows only in the right direction.
Arteries are vessels through which blood flows from the heart. Their walls have a well-developed muscle layer, thanks to which the arteries contract and relax, forcing the blood to move.
There are also elastic fibers in the walls of the arteries, so they can stretch when pressure increases and then return to their original state.
The tone of the walls of blood vessels, their ability to stretch and contract depending on small pressure surges, which are completely natural during the day, depend on muscle and elastic fibers.
Veins are vessels through which blood flows to the heart after it has “fed” the body and taken with it “dirty dishes,” that is, cell waste products.
The blood pressure in them is much lower. Apparently, the “dishes” are dragging.
Capillaries are the smallest vessels that can penetrate into every cell. The speed of blood flow there is minimal.
Treatment of the disease
Treatment of hypertension is complex and depends on the stage, severity, causes, gender and age of the person and other factors. The disease cannot be completely cured, but the patient’s condition can be significantly improved and the onset of life-threatening complications can be delayed for a long time. Treatment can be non-drug and medicinal.
Non-drug therapy. It involves adjusting the patient’s lifestyle. Most patients do not attach much importance to it, considering it frivolous, but such treatment is the key to success.
First of all, it is necessary to review the diet of the sick person, reduce the intake of carbohydrates and fats, and increase the intake of proteins and vitamins. You should reduce your caloric intake, which will subsequently lead to a reduction in cholesterol and body weight. It is also necessary to normalize the drinking regime, reduce salt consumption to 5 g per day.
When treating hypertension in older people, spa therapy and climatotherapy are especially recommended. The doctor prescribes therapeutic exercises and physical education. Reducing anxiety levels and using psychotherapy methods are helpful.
Pharmacological treatment. Quite often, in the treatment of hypertension, the principle of “steps” is used when prescribing medications. Groups of drugs are prescribed in the required sequence, since drugs have different degrees of impact in the mechanism of increasing blood pressure. When a person achieves a stable decrease in blood pressure, the doctor transfers the patient to maintenance therapy.
- When treating grade 1 high blood pressure, one antihypertensive drug is usually prescribed, which is taken on an outpatient basis under the supervision of a specialist. Medicines are prescribed in courses lasting several weeks.
- When treating stage 2 hypertension or when monotherapy is ineffective, the doctor usually prescribes 2 drugs. Therapy is carried out in a hospital. If an elderly person experiences a stable decrease in blood pressure, the patient continues treatment at home.
- Treatment of stage 3 hypertension requires an individual approach. It is carried out in a hospital until the condition stabilizes. The doctor evaluates the results of the examinations and prescribes a special course of treatment for stage 3 hypertension.
Who is to blame for high blood pressure?
1. “Nerves.” We freaked out, the adrenal glands released adrenaline, the heart began to work harder, the blood vessels spasmed (narrowed), and the pressure increased.
In general, this mechanism was not invented by the Creator by chance. Imagine a situation when you are walking calmly down the street and suddenly you see a huge dog rushing straight towards you. What are you going to do? Stand as before? NO! You will either take something in your hands for protection, or you will “make your legs”, that is, give it a go.
To do this, you need to tense your muscles so that they are prepared to fight or flee, supply them with oxygen, and therefore speed up the heart. Otherwise you'll be screwed.
And now the situation is different. This is a difficult buyer for you. He exhausted your soul, demanding that you let go of “something from the pressure.”
You steadfastly resist the onslaught, explaining that these drugs are prescribed only by a doctor.
But he doesn’t calm down, he starts accusing you of unprofessionalism and so on and so forth. A wave of indignation, irritation, and maybe even a desire to crack him properly rises inside you.
Can you hit him? No.
How about yelling back? You can, of course, but it will cost you more. There will be complaints, calls to the authorities, this and that... So again, no.
And if this situation occurs day after day, then hypertension can become your companion for the rest of your life.
2. Increased levels of “bad” cholesterol (low-density lipoproteins) in the blood.
With age, the elasticity of blood vessels decreases. High blood pressure, which becomes a frequent visitor, begins to damage the walls of blood vessels. While the inner lining of the vessels is smooth, nothing sticks to it.
But as soon as damage appears in it, the same low-density lipoproteins that eventually form cholesterol plaques begin to stick to them.
They further narrow the blood vessels and further reduce their elasticity.
3. Love of salty foods. Salt attracts water, increasing the volume of circulating blood, and therefore pressure.
4. Overweight. Body weight increases, but the length of blood vessels and the size of the heart remain the same. Under these conditions, they have to work harder to “feed” and “drink” the extra 10-20 kg. At first they cope with this, but in the end, they throw out the white flag and begin to work through the stump deck.
5. Smoking. The harmful substances contained in tobacco smoke constrict blood vessels, increasing blood pressure, plus they damage their walls, and “bad” cholesterol begins to stick to them.
6. Alcohol. It is a mistake to think that it dilates blood vessels. Vasodilation is replaced by persistent spasm, and the pressure jumps again.
7. Physical inactivity. It reduces the elasticity of the vascular wall. When we move, the pressure in the vessels constantly changes, and the vascular wall either contracts or relaxes, in general, it trains. This does not happen with a sedentary lifestyle.
8. Well, and heredity. Where would we be without her?
Prevention
Methods for preventing the disease are primary and secondary.
Primary prevention is necessary for healthy people who are predisposed to pathology. You need to go in for sports, fitness, do morning exercises, swim. It is important to consider that the loads should be moderate or light. A person also needs to give up bad habits, limit the consumption of salt, carbohydrates and animal fats. The diet should be enriched with calcium and potassium (dairy products, nuts, dried fruits, etc.).
Secondary prevention is carried out in patients who have been diagnosed with hypertension. It includes monitoring blood pressure, regular visits to the doctor and non-drug therapy. It is recommended to conduct acupuncture sessions, massage, and take herbal remedies and antioxidants.
The ABC-Medicine clinic provides a full range of services for the diagnosis, prevention and treatment of hypertension. Call us at + and our consultants will answer all your questions in detail and make an appointment with a cardiologist.
Where to get tested for hypertension in Moscow?
At a multidisciplinary medical center you can always get examined for hypertension
. Our medical center is located between the Konkovo and Belyaevo metro stations (South-Western Administrative District of Moscow in the area of the Belyaevo, Konkovo, Teply Stan, Chertanovo, Yasenevo, Sevastopolskaya, New Cheryomushki metro stations " and "Trade Union"). Here you will find highly qualified personnel and the most modern diagnostic equipment. Our clients will be pleasantly surprised by our quite affordable prices.