An ECG is a quick way to accurately check your heart's function. This study is prescribed not only to adults, but also to children at different ages. Doing an electrocardiogram is absolutely safe and the study can be carried out as often as the situation requires; there will be no negative impact on the child’s body. When choosing where to have a child’s heart cardiogram done, you should give preference to proven clinics with modern equipment and take into account that pediatric EGC has some differences from the adult procedure. It is especially important in a difficult epidemiological situation to be able to conduct this type of functional diagnostics at home.
What is an ECG?
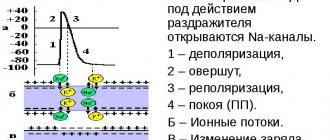
An ECG (electrocardiogram) is a simple and reliable way to study the functioning of the heart. During the procedure, the cardiograph records the electrical potentials that appear during the work of the heart muscle. All information is sent to the doctor in the form of a graph on a paper tape. The procedure is absolutely painless, ECG can be performed on children at any age. The study helps diagnose many dangerous cardiovascular diseases. An ECG of a child’s heart can detect diseases such as:
- hypertrophy (enlargement) of any parts of the heart;
- congenital or acquired heart defects, myocarditis;
- angina pectoris;
- myocardial infarction;
- blockage of the pulmonary artery by blood clots (thromboembolism);
- metabolic changes in the myocardium.
Children's ECG has several features. This is due to a number of reasons.
Explanation of the examination
The essence of electrocardiography is to determine the electrical potentials of cardiomyocytes detected by sensors. Electrical impulses are converted into a graphic image. Using an ECG, you can analyze the features of the anatomical position of the heart, identify heart rhythm disturbances, suggest the presence of enlargement of the heart chambers, and assess the quality of myocardial nutrition. An experienced doctor will decipher the results and issue a detailed conclusion, which is accompanied by a graphic image (electrocardiogram film).
Why does the ECG of a child’s heart have features?
Each age period has its own characteristics that must be taken into account when carrying out various procedures, including ECG. This is due to:
- anatomical location of the heart in the chest;
- different ratios of muscle mass of the right and left ventricles;
- changes in the rate of excitation in the myocardium;
- different frequency of contraction of the heart muscle;
- influences of a vegetative-endocrine nature.
Throughout the entire process of growing up and growing a child, the morphological structure of the heart and blood vessels constantly changes. This must be taken into account when performing an ECG in children.
The article presents modern principles of clinical interpretation of ECG in young athletes, the basis of which is the division of all detectable ECG phenomena into frequent and typical, as well as rare and atypical for athletes. The main elements of a clinical diagnostic search carried out when identifying ECG phenomena in a young athlete that go beyond the norm are considered.
Electrocardiography for the young athlete: a variant rule or pathology?
The paper presents the principles of modern clinical interpretation of ECG in young athletes, based on division of all detected ECG phenomena on frequent and typical, as well as rare and unusual for athletes.
It is obvious that today children's and youth sports are becoming widespread. Thus, according to the draft “Concept for the development of children’s and youth sports for 2009-2015” of the Federal Agency for Physical Culture and Sports, in the sports reserve training system already in 2006 there were about 4,500 sports-oriented institutions (which is more than a thousand more than their number in 1997), in which about 3.2 million people were involved in 104 sports; in general, more than 19% of children and adolescents aged 6-15 years regularly engage in sports [1].
Modern sport (and especially classes in sports reserve programs) places special demands on the functional systems of the body of a child and adolescent. The need for a young athlete to undergo clinical and instrumental examinations prior to the start of sports, as well as during his sports activities, is obvious and formally enshrined in Order No. 613n of the Russian Ministry of Health and Social Development of 2010 [2]. From a clinical cardiology perspective, such monitoring (as well as in-depth cardiac examinations) serves two purposes. The first is the identification of athletes with undiagnosed cardiovascular diseases with a latent and asymptomatic course, increasing the risk of life-threatening conditions and forming the basis of sudden death syndrome in athletes, which, being extremely rare, is nevertheless almost twice as common in athletes than in “non-sports” » populations [3]. The second goal is to identify pathological changes in the cardiovascular system of a young athlete, formed de novo, and which are designated by the collective term “myocardial dystrophy due to chronic physical overstrain” (Dembo A.G., 1960) or “stress cardiomyopathy of an athlete” (Zemtsovsky E. .V., 2002).
Currently, there are algorithms for cardiac screening of athletes developed abroad and in Russia [4, 5]. In particular, the closest to practical use is a 12-item questionnaire developed by the American Heart Association, which makes it possible to identify a group of athletes requiring in-depth examination (Table 1) [6]. It is important to note that the authors recommend that the young athlete be interviewed in the presence of his parents. In international practice, the questionnaire developed by the European Society of Cardiology (the so-called “Lausanne Guidelines”) is also widely used [7].
Table 1.
Panel of examinations for preliminary screening of athletes [6]
| Family history 1. Premature death (sudden or unexpected) before 50 years of age due to cardiovascular disease in a close relative; 2. Heart disease in close relatives of young age (up to 50 years); 3. The presence of the following cardiovascular diseases in close relatives: hypertrophic or dilated cardiomyopathy, arrhythmogenic dysplasia/cardiomyopathies of the pancreas, Marfan syndrome, long or short QT syndromes, Brugada syndrome, catecholaminergic ventricular tachycardia, Leva-Lenegra disease, life-threatening cardiac arrhythmias. |
| Complaints and anamnesis1 4. Previously detected heart murmur; 5. Arterial hypertension; 6. Unexplained fainting/presyncope, palpitations2; 7. Severe/unexplained shortness of breath on exertion; 8. Chest pain/discomfort during physical activity. |
| Examination results and physical examination data 9. Heart murmur (lying/standing)3; 10. Pulsation in the peripheral arteries (to exclude coarctation of the aorta); 11. External signs of Marfan syndrome; 12. Blood pressure measurement in the upper extremities (sitting)4; |
| 1 (when examining young athletes, it is recommended that parents be present when collecting anamnesis and complaints); 2 it is necessary to exclude the neurocardiogenic nature of fainting (vasovagal fainting), special attention should be paid to fainting that occurs during physical activity; 3 auscultation should be performed both lying down and standing (or using the Valsalva maneuver), especially if dynamic obstruction of the LV outflow tract is suspected; 4 preference is given to measurements on both upper limbs. |
An important method for diagnosing pathology of an athlete’s cardiovascular system is electrocardiography (ECG). The European Society of Cardiology, as well as the International Olympic Committee [8], recommend an algorithm for cardiac screening of young athletes, a mandatory part of which is an ECG (Fig. 1). However, the advisability of conducting an ECG for all athletes as a screening remains a subject of debate. The American Heart Association does not recommend ECG testing for all athletes, indicating that in athletes this method has low sensitivity and specificity, leads to a large number of false-positive results and unnecessary testing, and significantly increases the final cost of identifying a potentially life-threatening disease [6].
Figure 1. Algorithm for cardiac screening of young athletes [3]
An important step in understanding the norm, variant of the norm and pathology in the athlete’s ECG was the recommendations proposed in 2010 by Corrado D., Pelliccia A., Heidbuchel H. and co-authors [9]. The main purpose of these recommendations is to obtain a reliable boundary between physiological and potentially malignant changes in the athlete's ECG. For this purpose, all ECG phenomena were divided into two groups: the first - related to sports and occurring frequently, the second - not related to sports and occurring rarely (Table 2).
Electrocardiographic changes of the first group are interpreted as physiological, and in the absence of additional clinical and anamnestic data (Table 1), in most cases, do not require a diagnostic search, since they are associated with adaptive anatomical and physiological remodeling of the athlete’s myocardium.
Table 2.
Classification of ECG phenomena in athletes [9]
| Electrocardiographic phenomena | |
| Frequent, due to the training process | Infrequent, not related to training process |
| |
When identifying ECG phenomena of the first group, it is necessary to take into account that different sports are differently associated with such findings. They are more typical for sports that train endurance (long-distance running, rowing, cycling, skiing) than for strength and speed sports (weightlifting, arm wrestling, sprinting) [10].
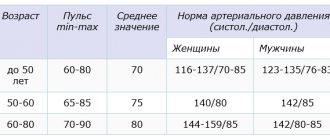
Interpretation of detected ECG phenomena requires their clinical understanding. Thus, when assessing the possible connection between an athlete’s bradycardia and sick sinus syndrome, in addition to the age standards developed by the Federal Medical and Biological Agency [11] (Table 3), it is necessary to focus on such clinical data as complaints of dizziness and fainting, an inadequately low increase in frequency pulse during physical activity, results of functional and medicinal tests, persistence of bradycardia after giving up sports.
Table 3.
Interpretation of changes in heart rate (bpm) in children 5-18 years old (protocol of TsSSSA FMBA of Russia)
| Age | Severe bradycardia | Moderate bradycardia | Norm | Moderate tachycardia | Severe tachycardia |
| 5-7 years | <70 | 71-79 | 80-105 | 106-129 | >130 |
| 8-11 years | <65 | 66-74 | 75-95 | 96-114 | >115 |
| 12-15 years | <50 | 51-69 | 70-90 | 91-109 | >110 |
| 16-18 years old | <50 | 51-64 | 65-80 | 81-109 | >110 |
| >18 years old | <45 | 46-59 | 60-80 | 81-109 | >110 |
I degree AV block, also often found in athletes, requires additional examination (cholesterol monitoring ECG, echocardioscopy, electrophysiological study) only in the presence of concomitant widening of the QRS complex, prolongation of the PQ interval by more than 300 ms, as well as deterioration of AV conduction during stress tests or hyperventilation tests. A similar tactic is chosen when a second-degree AV block of type Mobitz I is detected in a young athlete: the indication for an in-depth examination is only the presence of symptoms (dizziness, syncope) and deterioration of AV conduction during stress tests. Third-degree and second-degree AV blocks of the Mobitz type II are not a manifestation of adaptive changes in the heart of a young athlete; they require an in-depth examination and, as a rule, refusal to play sports [4].
Early ventricular repolarization syndrome is also a benign ECG phenomenon, typical of young athletes and reflecting increased activity of parasympathetic influences on the myocardium. Typical ECG signs of this syndrome are the presence of a junction point (pseudo-r wave) or junction wave (J wave) on the descending limb of the R wave and a horizontal or oblique rise of the ST segment by 1-6 mm with convexity downwards. Signs may vary in severity, morphology and distribution. According to some studies [12, 13], pathogenetic mechanisms similar to those in idiopathic ventricular fibrillation and Brugada syndrome are observed in SRGC, and therefore the unifying term “J wave” syndrome is sometimes proposed [14]. Based on this, if an athlete detects early repolarization syndrome in the inferior or lateral leads (especially with a pronounced change in the terminal part of the QRS), combined with syncope and episodes of cardiac arrest, the European Society of Cardiology recommends considering idiopathic ventricular fibrillation as a possible diagnosis.
A common ECG phenomenon found in athletes is the voltage criteria of left ventricular hypertrophy (Sokolov-Lyon criterion and Cornell index) with preservation of the normal electrical axis of the heart, ventricular and atrial electrical activity, without displacement of the ST segment and changes in T waves in the left leads. These criteria are not applicable in childhood and almost never indicate truly existing myocardial hypertrophy in an athlete. Thus, having studied the electrocardiography of 1005 high-class athletes, Pellicia A. et al. identified voltage criteria for hypertrophy in 60% of those examined, but subsequently none of the cases were confirmed by ultrasound examination data [10]. At the same time, non-voltage criteria for ventricular myocardial hypertrophy, such as left atrial hypertrophy, deviation of the electrical axis of the heart to the left, changes in the ST segment and T wave, increased internal deviation time, and pathological Q waves require ultrasound imaging to exclude structural heart diseases.
Also, atypical ECG changes in athletes include T wave inversion, taking into account ECG features in children, such as smoothed, biphasic or negative T waves in standard III and aVL leads, as well as in the right chest leads (V1-V3) in prepubertal age. Negative T waves are found in athletes much less frequently than was commonly believed [10, 15], and T wave inversion of more than 2 mm in adjacent leads may indicate structural heart disease. Negative T waves in the inferior leads (II, aVF) and lateral leads (I, aVL, V5-V6) may indicate the presence of diseases in the athlete such as hypertrophic cardiomyopathy, left ventricular non-compact myocardium syndrome, stable arterial hypertension, valvular heart defects and require in-depth examination.
Volva-Parkinson-White syndrome in athletes occurs with the same frequency as in the rest of the population and amounts to 0.1-0.3% [16]. This syndrome is a rare cause of life-threatening arrhythmias (atrial fibrillation and subsequent ventricular fibrillation) and accounts for no more than 2% of the causes of sudden death in athletes [17]. If there is a clinical picture of paroxysmal supraventricular tachycardia, episodes of atrial fibrillation/flutter and fainting states, the athlete is advised to conduct an electrophysiological study according to the standard protocol. Management tactics for adult and young athletes with asymptomatic Volva-Parkinson-White syndrome vary. Thus, adult athletes (especially those older than 20-25 years) are recommended to undergo a procedure of radiofrequency ablation of additional conduction pathways; in case of refusal of the athlete, all sports are allowed, with the exception of those associated with a high risk of syncope according to the classification of Mitchell JH et. al. [18, 19]. Athletes of childhood and adolescence need to conduct an electrophysiological study before starting sports to induce tachycardia attacks and determine the effective refractory period of additional conduction pathways. Given that atrial fibrillation is extremely rare before the age of 12 years, electrophysiological testing may be postponed with recommendations for an annual in-depth cardiac examination [4].
Clinical interpretation of the electrocardiogram of a young athlete implies a mandatory assessment of the duration of the QT interval in standard lead II or in precordial leads V3 or V5 (the longest interval is taken into account). However, it is necessary to keep in mind a number of difficulties in assessing the QT interval in athletes: the inaccuracy of the Bazett formula for calculating QTc with severe sinus arrhythmia (typical of athletes), as well as with bradycardia less than 40 beats per minute and tachycardia more than 120 beats per minute. The accuracy of the calculations is also influenced by the slightly wider QRS complex in athletes and the more frequent detection of the U wave. In the presence of a U wave, the end of the T wave should correspond to the “bottom” point between the T and U waves, and in the absence of the transition point of the T wave to the U -wave in this lead QT interval is not calculated [20]. The normative value of QTc is considered to be 440-450 ms, but today recommendations are being made to expand the normal limit to 470 ms for men and 480 ms for women [21, 22]. There is a tendency to find a longer QTc interval in athletes, but in general this indicator is within the same normative limits as in the general population.
If a prolonged QT interval is detected in a young athlete, it is necessary to exclude acquired, and in some cases, congenital variants of the syndrome. The most common causes of secondary QT prolongation are:
- taking medications that cause QT prolongation (a list is available on the Arizona Center of Education and Research Therapeutics website https://www.qtdrugs.org/);
- metabolic and electrolyte disturbances (for example, due to chronic dehydration of an athlete or a protein-free diet of an athlete);
- structural myocardial diseases.
The minimum set of examinations includes echocardioscopy and Holter monitoring, and genetic analysis is performed if indicated.
More rare is the short QT interval syndrome, in which absolute QT values of less than 310 ms and a corrected QT interval of less than 360 ms are detected for children. This rare form of channelopathies is also associated with a risk of fatal ventricular tachyarrhythmias.
Thus, the domestic and foreign recommendations given in the article for the clinical interpretation of the ECG of young athletes make it possible to avoid both overdiagnosis of benign adaptive changes in the cardiovascular system and underestimation of the importance of some potentially malignant ECG phenomena.
AND I. Lutfullin, A.I. Safina
Kazan State Medical Academy
Volga State Academy of Physical Culture, Sports and Tourism
Lutfullin Ildus Yaudatovich – Candidate of Medical Sciences, Assistant at the Department of Pediatrics and Neonatology
Literature:
1. Draft concept for the development of children's and youth sports for 2009-2015 of the Federal Agency for Physical Culture and Sports. - Electron. Dan. — Access mode sport.pskov.ru/downloads/Koncepciya_razvitiyaa_sporta.doc, free.
2. Order of the Ministry of Health and Social Development of Russia No. 613n. — Access mode https://www.rg.ru/2010/10/01/sport-dok.html, free.
3. Corrado D., Pelliccia A., Bjornstad HH et. al. Cardiovascular preparticipation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology // Eur. Heart J. - 2005. - Vol. 26, No. 516. — 524 rub.
4. All-Russian Scientific Society of Cardiologists. National recommendations for admission to sports and participation in competitions for athletes with deviations from the cardiovascular system // Rational pharmacotherapy in cardiology. - 2011. - T. 7, No. 6. - P. 2-60.
5. Maron BJ, Zipes DP 36th Bethesda Conference: eligibility recommendations for competitive athletes with cardiovascular abnormalities // J. Am. Coll. Cardiol. - 2005. - Vol. 45. - P. 2-64.
6. Maron BJ, Doerer JJ, Haas TS et. al. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. - 2009. - Vol. 119, No. 8. - R. 1085-92.
7. Bille K., Figueras D., Schamasch P. et. al. Sudden cardiac death in athletes: the Lausanne recommendations // Eur. J. Cardiovasc. Prev. Rehabil. - 2006. - Vol. 13. - P. 859-875.
8. Ljungqvist A., Jenoure PJ, Engebretsen L. et al. The International Olympic Committee (IOC) Consensus Statement on Periodic Health Evaluation of Elite Athletes // Clin. J.Sport. Med. - 2009. - Vol. 19. - P. 347-365.
9. Corrado D., Pelliccia A., Heidbuchel H. et. al. Recommendations for interpretation of 12-lead electrocardiogram in the athlete // Eur. Heart. J. - 2010. - Vol. 31, No. 2. - P. 243-59.
10. Pelliccia A., Maron BJ, Culasso F., Di Paolo FM, Spataro A., Biffi A., Caselli G., Piovano P. Clinical significance of abnormal electrocardiographic patterns in trained athletes. Circulation. - 2000. - Vol. 102. - P. 278-284.
11. Makarov L.M., Komolyatova V.N. Standard ECG parameters in children. Functional diagnostics. - 2010. - No. 3. - P. 92-95.
12. Letsas KP, Sacher F., Probst V. et. al. Prevalence of early repolarization pattern in inferolateral leads in patients with Brugada syndrome // Heart Rhythm. - 2008. - Vol. 5, No. 12. - P. 1685-1689.
13. Shu J., Zhu T., Yang L. et. al. ST-segment elevation in the early repolarization syndrome, idiopathic ventricular fibrillation, and the Brugada syndrome: cellular and clinical linkage // J. Electrocardiol. - 2005. - Vol. 38, No. 4. - P. 26-32.
14. Ortega Carnicer J. Acute inferior myocardial infarction masking the J wave syndrome. Based on four observations // Med. Intensiva. - 2008. - Vol. 32, No. 1. - P. 48-53.
15. Sharma S., Whyte G., Elliott P., Padula M., Kaushal R., Mahon N., McKenna WJ Electrocardiographic changes in 1000 highly trained junior elite athletes // Br. J.Sports. Med. - 1999. - Vol. 33. - P. 319-324.
16. Surawicz B., Childers R., Deal BJ, Gettes LS AHA/ACCF/HRS Recommendations for the standardization and interpretation of the ECG: Part III: intraventricular conduction disturbances // J. Am. Coll. Cardiol. - 2009. - Vol. 53. - P. 976-981.
17. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006 // Circulation. - 2009. - Vol. 119, No. 8. - P. 1085-92.
18. Lutfullin I.Ya., Safina A.I. Modern arrhythmological criteria for admission to sports training and competitions for children and adolescents // Practical Medicine. - 2011. - No. 53. - P. 25-29.
19. Mitchell JH, Haskell W., Snell P., Van Camp SP Task Force 8: classification of sports // J. Am. Coll. Cardiol. - 2005. - Vol. 45, No. 8. - P. 1364-7.
20. Kapushchak O.V., Makarov L.M., Shkolnikova M.A. Dispersion of the QT interval in children 7-16 years old according to standard electrocardiography // Bulletin of Arrhythmology. - 1999. - No. 12. - P. 39-42.
21. Basavarajaiah S., Wilson M., Whyte G., Shah A., Behr E., Sharma S. Prevalence and significance of an isolated long QT interval in elite athletes // Eur. Heart. J. - 2007. - Vol. 28. - P. 2944-2949.
22. Rautaharju PM, Surawicz B., Gettes LS AHA/ACCF/HRS Recommendations for the standardization and interpretation of the ECG: Part IV: the ST segment, T and U waves, and the QT interval // J. Am. Coll. Cardiol. - 2009. - Vol. 53. - P. 982-991.
ECG in a newborn during the first two days of life
In the ECG of children, individual fluctuations are observed during the first two days. Immediately after birth, the heart rate is 157 per minute, and after cutting the umbilical cord - 142 per minute. In the first hours after birth, doctors note fluctuations in the RR interval from 0.44 to 0.54″, the heart rate is 123.0±1.8 per minute. To perform an ECG on an infant, it is important to swaddle him well. This is necessary to ensure that the recording of the electrocardiographic curve is correct. The child should be warm and motionless. Swaddling is abandoned only if the child is in serious condition and practically does not move. It is recommended to record an ECG 1.5-2 hours after feeding and before X-ray examinations and physical procedures.
Where can I get an ECG for a child in Moscow?
If your child has received a referral for an ECG, then this is not a reason to panic. The procedure is completely painless and will not take more than 10 minutes. Research is carried out using modern technology and gives very accurate results. ECG in children has many features. Our clinic specialists have extensive experience in reading cardiograms. The Medicine Clinic is accredited according to the most stringent American standards of medical care and is ready to provide you with:
- diagnostics using the latest equipment, which is used in the best clinics in Europe;
- service at the level of foreign medical centers;
- consultations and treatment from the best specialists in Europe and Russia.
In the modern Meditsina clinic, you can do a paid ECG for your child and order an interpretation from an experienced cardiologist. You will receive reliable information about your baby’s health condition and, if necessary, receive timely treatment.