Rules for measuring blood pressure in children
It is preferable to measure blood pressure at home with an automatic or semi-automatic tonometer, the use of which will greatly facilitate the procedure and eliminate the influence of the human factor. It is important to select the correct cuff as measuring with an adult cuff will give incorrect results. The dimensions of the cuff depend on the age of the child and are: for infants - 3.5x7 cm; from 1 to 2 years – 4.5×9 cm; from 2 to 4 years – 5.5×11 cm; from 4 to 7 years – 6.5×13 cm; from 7 to 10 years – 8.5×15 cm; from 10 and older - an adult cuff is suitable.
It is best to measure blood pressure in the morning, 15-20 minutes after waking up or resting. The child should take a comfortable position (lying or sitting), be calm and relaxed. The hand on which the measurement will be taken should be at heart level and free of clothing. Next, a cuff is attached to the arm 2-3 centimeters above the elbow, and depending on the type of device, measurements begin. If this is an automatic tonometer, then just press the power button and air will automatically be pumped into the cuff and after a few seconds the result will appear on the device display. In a semi-automatic tonometer, air is pumped and released using a bulb. For a more reliable result, you should measure the pressure 3 times with an interval of 2-4 minutes and calculate the average value.
Rational approaches to the diagnosis and treatment of arterial hypertension in children and adolescents
Arterial hypertension (AH) in children and adolescents is not uncommon and is a common disease that occurs during the formation of neurogenic and humoral mechanisms regulating the cardiovascular system and blood pressure.
This is confirmed by epidemiological studies conducted abroad and in Russia using the method of random selection with a sufficient number of subjects and unified standardized methods for measuring blood pressure (BP), which made it possible to obtain objective data on the prevalence of hypertension in children and adolescents, which ranges from 2.4 to 18% .
The problem of diagnosing and treating hypertension in the adult population is widely and thoroughly presented in foreign and domestic literature and is discussed at conferences, congresses and forums. Today, almost every doctor in an adult clinic and hospital begins examining patients by measuring blood pressure. The diagnostic strategy and treatment tactics for childhood hypertension are currently attracting the attention of many domestic and foreign scientists. Recommendations for the diagnosis, treatment and prevention of hypertension in children and adolescents, developed by experts from the All-Russian Scientific Society of Cardiologists (VNOK) and the Association of Pediatric Cardiologists of Russia, which were approved at the Russian Congress of Cardiologists in October 2003, have been published.
Prevalence and Pharmacotherapy of Arterial Hypertension in Children conducted in 2005 , made it possible for the first time to assess the real knowledge of pediatricians on the issues of diagnosis and treatment tactics for hypertension in children. It turned out that the level of knowledge of pediatricians in the field of diagnosing hypertension in children and adolescents is at a low level: only 36.7% of doctors correctly measure blood pressure in children, following the methodology and frequency of blood pressure measurement and using age-specific cuffs. Most doctors (51.6%) are not familiar with the methodology for assessing blood pressure results in accordance with gender, age and height.
the main reasons for the low diagnosis of hypertension in childhood to be: the lack of methodological recommendations (46.5%), the lack of percentile tables (37.1%) and the “isolation of methodological recommendations from practice” (8.6%).
Despite the fact that the majority (77.8%) of pediatricians recognize the possibility of the development of hypertension in childhood, the existing practice of identifying high blood pressure among children of various age groups is the subject of discussion, because the method of measuring blood pressure is the leading component of diagnosing this pathology. Unlike adults, children do not have a single normal pressure; blood pressure values are determined by age, gender and height and are established using percentile tables.
In pediatrics, there is no approved classification of hypertension , but there is a classification of levels of elevated blood pressure in children of different ages. This classification, proposed by the Second Working Group on the Control of Blood Pressure in Children in 1987, has been adopted by WHO and is a guideline that helps in the diagnosis of hypertension. This classification is used in the Recommendations for the diagnosis, prevention and treatment of hypertension in children and adolescents, developed by VNOK and the Association of Pediatric Cardiologists (2003)
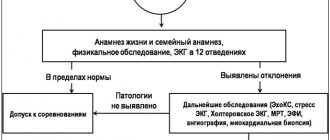
Diagnosis of hypertension in children and adolescents begins with establishing the fact of increased blood pressure, which is revealed in the process of systematic measurement.
As the results of the RIFAGD study showed, in everyday practice, systematic measurement of blood pressure is carried out by doctors mainly in school-age children (85.2%), and in the older age group more often (51.6%) than in younger school-age children (33.6%). %), which is apparently due to regular in-depth examinations of teenage schoolchildren conducted by specialists in schools.
To measure blood pressure, the officially approved method of S. Korotkov is used. Automatic or semi-automatic instruments are commonly used for this purpose: aneroid sphygmomanometers and oscillometric devices, which have been clinically tested for accuracy and meet ESH1 criteria, are equipped with a set of cuffs of different sizes, allowing measurements in different age groups.
In accordance with the Recommendations of the VNOK and the Association of Pediatric Cardiologists (2003), the length of the cuff should cover up to 80% of the circumference of the child’s shoulder, located 2-2.5 cm above the elbow. Typically, the shoulder circumference is measured with a tape measure, which allows you to determine the size of the cuff you need.
In real practice, only 36.7% of pediatricians use age-related cuffs for measuring blood pressure The vast majority of pediatricians use “adult” cuffs, the use of which distorts the results of blood pressure measurements (as a rule, they are underestimated), which does not allow an adequate assessment of the child’s true blood pressure. However, in the diagnosis of hypertension, it is important not only to be equipped with age-related cuffs, but also to know the methods for measuring blood pressure in children and adolescents, and especially to evaluate the results of blood pressure measurements.
Methodology for measuring blood pressure in children and adolescents
Blood pressure measurements should be taken after the child has rested for 5 minutes in a quiet, calm environment. The child should sit on a chair with a straight back, the patient's hand should be at heart level. Blood pressure should be measured no earlier than 1 hour after eating, drinking coffee, stopping physical activity, or being in the cold. The patient's shoulder should be free of clothing, the hand should lie comfortably on the table (when measuring blood pressure in a sitting position) or on the couch (when measuring blood pressure in a lying position), palm up. The person measuring blood pressure should explain the measurement procedure to the child in order to avoid a negative reaction from the patient, which could cause an increase in blood pressure. Throughout the entire procedure for measuring blood pressure, the child should not change position or talk.
Methodology for assessing blood pressure measurement results
Assessment of blood pressure levels in children and adolescents is conditional, because Until recently, normal blood pressure limits in the pediatric population have not been established, based on a sufficient number of studies. To determine the proper blood pressure value, it is necessary to first determine the child’s growth percentile, and then, taking into account age and gender, using percentile tables, determine the blood pressure level using the average of 3 consecutive blood pressure measurements with a time interval of 2-3 minutes.
For example, for a 9-year-old boy with a height of 142 cm, we determine using tables the percentile (hereinafter referred to as the percentile) of height, which corresponds to 90 percent. When measuring blood pressure , the average values of three measurements were obtained = 135/78 mm Hg. Next, we compare the obtained blood pressure measurement results with the data of percentile tables corresponding to gender (boy) and height percentile (90). The SBP level corresponding to 90 points of this child is 117 mm Hg, and DBP is 76 mm Hg. Comparing the results of measuring the blood pressure of this child, we can conclude that for the corresponding age, gender and height, there is an increase in the levels of SBP and DBP of more than 95 pp.
However, the obtained blood pressure measurement results do not allow us to make a diagnosis of hypertension. To confirm a persistent increase in blood pressure, it is important to carry out repeated blood pressure measurements in a familiar (home) environment and at an outpatient appointment with an interval of at least 24 hours. If possible, 24-hour blood pressure monitoring is performed to exclude “white coat” hypertension and labile hypertension.
The results of the RIFAGD study showed that almost half of pediatricians (51.2%) are not familiar with the methodology for assessing the results of blood pressure measurements in accordance with gender, age and height.
Treatment
The main goal of hypertension treatment is to achieve sustainable normalization of blood pressure, which reduces the risk of early cardiovascular disease and mortality. For children and adolescents, this means achieving the target blood pressure level, which should be less than 90 pp for the corresponding age, sex and height.
Treatment of hypertension begins with lifestyle changes. Adult patients are asked to quit smoking, reduce and even stop drinking alcohol, increase their physical activity, reduce their intake of salt, foods rich in saturated fat and cholesterol, and increase their consumption of fish, fruits and vegetables. For hypertension in children and adolescents, non-drug therapy (NT) is also of enormous importance, because it is the main treatment for patients with “high normal pressure” and for hypertension of any degree, in which it is prescribed simultaneously with medication.
The main methods of NT in childhood are measures to reduce excess body weight, physical activity, changes in diet and quality of nutrition. It has been proven that reducing the calorie content of food due to the consumption of animal fats and easily digestible carbohydrates leads to a decrease in body weight, especially in combination with an increase in physical activity carried out through dynamic loads - swimming, running, team sports.
According to our survey, the majority of respondents (74.6%) begin treatment for hypertension in children and adolescents with HT. 44.3% of pediatricians consider a salt-restricted diet to be the main component of NT. Unfortunately, none of the doctors who took part in the survey noted that the main component of HT is weight loss in children and adolescents, although it is known that weight gain is a predictor of hypertension in both adults and children. In the pediatric population, weight loss (as in adults) in obese children and adolescents often leads to a decrease in blood pressure without drug therapy.
The RIFAGD study revealed that the actual knowledge of pediatricians in the treatment of hypertension in children and adolescents does not meet existing standards: pediatricians underestimate the importance of NT and especially physical activity as an element of NT. Increased physical activity was indicated by only 0.1% of doctors, and physical therapy exercises by 2.5%.
Drug therapy
The timing and indications for prescribing MT for hypertension in childhood are strictly regulated. The absolute indications for prescribing MT in children with hypertension are: symptomatic hypertension, target organ damage (left ventricular hypertrophy, retinopathy, microalbuminuria), secondary hypertension, persistent hypertension against the background of ineffective MT.
for prescribing MT include persistent or nocturnal hypertension detected by 24-hour blood pressure monitoring; presence of cardiovascular risk factors (smoking, hyperlipidemia); hypertension due to obesity; hereditary hypertension.
In accordance with the Recommendations for the diagnosis, prevention and treatment of arterial hypertension in children and adolescents (2003), children with stage I hypertension are prescribed MT if NT is ineffective for 6-12 months. If II degree hypertension is detected in a child or adolescent, drug treatment is prescribed simultaneously with NT. If a teenager 16 years of age or older is in a high-risk group, drug therapy is prescribed simultaneously with NT, regardless of the degree of hypertension.
An indication for prescribing MT is also the identification of stable hypertension with a daytime or nighttime hypertension time index of more than 50%.
The basic principle of treating hypertension in both adults and children is a “step-by-step approach to treatment.” The essence of this approach is to gradually increase the dose of the antihypertensive drug until blood pressure is controlled or until adverse reactions occur. If blood pressure control is not achieved, then a drug from another pharmacological group is added, which is prescribed according to the same rules.
for the treatment of hypertension in adults: diuretics (DI), β-blockers (BAB), angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor antagonists (ARAs), calcium antagonists, α-blockers and imidazole receptor agonists, which do not have significant differences in their hypotensive effect, but differ from each other in tolerability and individual sensitivity of patients to them.
For the treatment of children and adolescents with hypertension, only 5 main groups can be used: diuretics, β-blockers, calcium antagonists, ACE inhibitors and angiotensin II receptor antagonists.
The results of the RIFAGD study showed that for the treatment of hypertension in children and adolescents, pediatricians more often choose drugs for the treatment of autonomic dysfunction (62%), and the share of antihypertensive drugs is only 38%. Among the medications used for the treatment of hypertension in children and adolescents, the following were named: ACE inhibitors (11.4%), diuretics (7.2%), beta blockers (8.3%), calcium antagonists (1.6%), drugs central action (clonidine) - 0.2%, myotropic antispasmodic - dibazole (1.5%) and combination drugs - papazole (6.7%), adelfan (0.6%).
The results of the study showed that pediatricians believe that the main group of drugs for the treatment of hypertension in children and adolescents are ACE inhibitors, the share of which among antihypertensive drugs was 39.9%. The data obtained correspond to the existing trends in the selection of antihypertensive drugs by internists and cardiologists in Russia, which is confirmed by the results of multicenter pharmacoepidemiological studies.
ACE inhibitors have a number of advantages that attract the attention of healthcare practitioners. They combine high efficiency, proven by numerous clinical studies, good tolerability, and also influence the mechanisms of progression of cardiovascular complications, reducing their frequency and increasing the life expectancy of patients with long-term use. It is important to have randomized clinical studies that have confirmed the effectiveness and safety of the use of certain drugs from the ACEI group (captopril, enalapril, fosinopril) in childhood.
When choosing drugs from the ACEI group, respondents from all centers indicated enalapril (63.7%) and captopril (36.3%), which corresponds to Russian and foreign recommendations. The GFOC and Pediatric Cardiology Association Recommendations (2003) recommend enalapril, captopril and, in adolescents, fosinopril. In addition to the above-mentioned drugs, foreign recommendations include benazepril, lisinopril and quinapril.
The group of angiotensin II receptor antagonists was named in only one center, and their share was 0.02%, which generally allows us to consider this group of antihypertensive drugs unclaimed. Foreign recommendations for the treatment of hypertension in children and adolescents recommend 2 drugs from the ARA group - losartan and irbesartan, the effectiveness of which has been proven in randomized clinical trials.
According to the results of the RIFAGD study, the beta blocker group turned out to be the second most frequently prescribed, the share of which among antihypertensive drugs was 28.8%. These drugs are more often prescribed by cardiologists (15.9%), less often by local doctors.
Previously, it was believed that beta blockers are the main antihypertensive drugs for the treatment of hypertension in children and adolescents , although drug manufacturers indicate in the annotations that childhood is a contraindication to their use.
Our study showed that pediatricians at all centers use beta blockers. Respondents indicated: atenolol - 37.8%, propranolol (Anaprilin, Obzidan) - 30.8%, metaprolol (Metocard, Egilok, Corvitol) - 24.9%, bisoprolol (Concor) - 6.5%, which in most cases (93.5%) are indicated in the Recommendations of the All-Russian Scientific Committee and the Association of Pediatric Cardiologists (2003).
In recent years, data have been obtained on the occurrence of muscle weakness when using beta blockers in the treatment of hypertension in adolescents involved in sports. In this regard, the recommendations for use included restrictions on the use of this pharmacological group in athletes. It has been proven that the use of non-selective beta blockers (atenolol, propranolol) increases the risk of hyperglycemia and hyperlipidemia, and therefore their use in the treatment of hypertension due to diabetes mellitus is not recommended.
According to the results of RIFAGD, the third group of antihypertensive drugs used by pediatricians were diuretics, the share of which was 24.9%, which generally reflects the trends in the choice of Russian internists and cardiologists.
Diuretics are the “oldest” antihypertensive drugs that have been used to treat hypertension since the late 50s of the twentieth century. Previously, they were used as second-line drugs in cases of ineffectiveness or intolerance to the drugs rauwolfia, hydralazine and methyldopa. Currently, data have been obtained from numerous studies that have shown that long-term use of DU leads to a reduction in cardiovascular complications and improves the prognosis in patients with hypertension.
Recommendations of the VII Report of the United States Joint National Committee on the Detection, Evaluation and Treatment of Hypertension (JNC VII, 2003) and recommendations of the WHO and the International Society of Hypertension (WHO/IAS, 2003), recommendations of the WHOC and the Association of Pediatric Cardiologists (2003). ) suggest starting treatment of hypertension with thiazide diuretics.
The main drug used for the treatment of hypertension in children and adolescents turned out to be a thiazide diuretic - hydrochlorothiazide (52.6%), which corresponds to the Recommendations of the GFOC and the Association of Pediatric Cardiologists (2003). In addition, thiazide-like diuretics are recommended as antihypertensive agents, in particular low-dose slow-acting indapamide, which is considered an effective and cheapest antihypertensive drug and can be used both for monotherapy and in combination with other drugs.
Along with drugs with proven antihypertensive effectiveness, about 25% of respondents indicated in the questionnaires combination drugs, the use of which is currently abandoned by therapists and cardiologists and which were not included in the Recommendations of the GFOC and the Association of Pediatric Cardiologists (2003). Among the named drugs were adelphan ezidrex (reserpine + dihydralazine + hydrochlorothiazide) - 0.6%, papazole (papaverine hydrochloride + dibazole) - 6.7%, dibazol - 1.5%. Combination drugs were indicated in descending order: school doctors - 27.3%, local pediatricians - 22.8%, doctors of other specialties - 21.6%, neurologists - 20%, doctors who did not indicate a specialty - 16.6% and cardiologists - 12.1%.
Conclusion
The conducted pharmacoepidemiological study “RIFAGD” made it possible for the first time to evaluate the real knowledge of pediatricians on the issues of diagnosis and treatment tactics for hypertension in children. The level of knowledge of pediatricians in diagnosing hypertension in children and adolescents is low:
- only 36.7% of doctors correctly measure blood pressure in children using age-specific cuffs and following the methodology and frequency of blood pressure measurement;
- the majority of doctors (51.6%) are not familiar with the methodology for assessing blood pressure results in accordance with gender, age and height.
the main reasons for the low diagnosis of hypertension in childhood to be :
- lack of methodological recommendations (46.5%),
- lack of percentile tables (37.1%),
- “disconnection of methodological recommendations from practice” (8.6%).
The actual knowledge of pediatricians in the treatment of hypertension in children and adolescents does not meet existing standards: most doctors (42.3%) use short (7-21 days) courses of NT and underestimate its importance, especially physical activity (0.1%), and the vast majority of pediatricians (63.4%) are not familiar with modern antihypertensive drugs.
The main drugs for the treatment of hypertension in children and adolescents , according to respondents, are drugs for the treatment of autonomic dysfunction syndrome (62%). Drugs with a low safety profile are unreasonably often used for the treatment of arterial hypertension in pediatrics: captopril (36.3%), atenolol (37.8%), propranolol (30.8%), combination drugs (7.3%) and not recommended for the treatment of this pathology - furosemide (30.4%), spironolactone (13.1%), triamterene (3.8%).
Respondents believe that the main reasons for the low level of knowledge in the field of drug therapy for hypertension in childhood are: lack of methodological recommendations (37.3%), lack of treatment practice (30.4%) and lack of indications for prescribing drugs (31.9%).
Source: Medical Council magazine No. 3 2007.
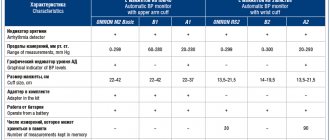
Suitable tonometers for measuring
It is not necessary to buy a separate blood pressure monitor for a child; it is enough to purchase a children’s cuff. When purchasing a tonometer, pay attention to its functionality. For a large family, it is worth choosing a tonometer with measurement memory for two users with recording of measurement time. This will help track the slightest deviations in pressure from the norm. For hypertensive patients, morning hypertension monitoring functions and a high blood pressure indicator will not be superfluous.
Tonometer Omron M1 Eco Approximate price: 1,700 rubles
- semi-automatic tonometer;
- memory for 42 results + date and time registration;
- indicators of arrhythmia and high blood pressure;
- calculation of the average blood pressure value from the last three results;
- large display.
Tonometer Omron M10-IT Approximate price: 8,900 rubles
- automatic tonometer;
- memory for 2 users for 84 measurements + guest mode;
- indicators of movement, arrhythmia, high blood pressure;
- the presence of a function for calculating the average blood pressure value from three measurements;
- It is possible to connect to a computer.