The ICP monitoring system allows you to conduct a primary screening study of intracranial pressure in newborns and children under 1 year of age in a non-invasive way and see ICP numbers on the screen of a bedside monitor. Includes ICP sensor, amplifier (signal decoder), cable for connection to a bedside monitor (custom made), 2 calibration kits, instructions and recommendations for clinical use. The system is calibrated at the interface between water and air and is intended for reusable use. The measurement error is 2-3 mmHg, due to the anatomy and principle of the study. Considering that the measurement is carried out without a high potential risk for a small patient (non-invasively), the results are interpreted as screening and allow one to assess the risks of developing complications of increased intracranial pressure. For example, if a child’s ICP figures are 20-25 mmHg. and higher, then the existing measurement error can be neglected, since the zero drift is 2-3 mmHg. Art. in such conditions it has no clinical significance; urgent measures are required to reduce intracranial pressure in the child. The measurement error of ICP monitors designed for invasive ICP measurement through the burr hole or subdural ranges from 1 to 2 mmHg. (depending on the brand of monitor).
Currently, this technique is successfully used in the Russian Federation and the CIS and is available for both public health facilities and private clinics. The system can be used both in a hospital and on an outpatient basis. The system is manufactured in the UK.
Symptoms of increased intracranial pressure in infants (from open sources)
Anxiety, vague moodiness, sleep disturbance, tearfulness and loudness. All children cry, but if a child constantly screams at the slightest irritation, sleeps poorly, is restless, then there is reason to think.
In addition, increased intracranial pressure can be assumed if the child eats poorly and little or eats small portions very often, spits up a lot and often, and perhaps periodically vomits.
Symptoms may also include increased muscle tone and tremors of the arms and legs when they tremble, for example, when excited or screaming.
There may be ophthalmological symptoms: constant or periodic strabismus, protrusion and drooping of the eyes and other changes.
Ways to reduce pressure in intracranial hypertension
Since such a pathology is most often a symptom of a disease, it is necessary to eliminate the cause of its occurrence.
To ensure the flow of cerebrospinal fluid, in some cases, surgery is performed to remove a tumor, abscess or hematoma. If the cause is an infectious inflammation of the meninges, then massive antibiotic therapy is carried out. It is possible to introduce them into the subarachnoid space.
To eliminate symptoms, methods are used that include non-drug and drug therapy. First, you need to raise the victim's head and limit fluid intake.
Diuretics are used among medications to remove excess fluid from tissues. Acetazolamide and Furosemide have this effect. The therapy is selected by a neurologist. Diacarb effectively reduces the production of cerebrospinal fluid.
To improve microcirculation and blood supply to tissues, neuroprotectors and nootropics are used. In severe cases, hormonal therapy is required under monitoring of vital signs.
Carrying out a spinal puncture with mechanical extraction of cerebrospinal fluid has a hypotensive property. Surgery is often required. Shunt surgery is planned to artificially drain fluid from the brain.
ICP norms of intracranial pressure in children and adults (from open sources)
Intracranial pressure in newborns is normally lower than in older children and adults. It should be taken into account that the normal numbers can change both up and down, but this will not mean that the child is sick. Increased or slightly decreased intracranial pressure in newborns and children may be due to exposure to some external irritants. For example, a cold or, conversely, hot room, emotional state (when, say, the baby was upset about something, the mother scolded or did not buy the desired toy, when the child did not get enough sleep) and even the posture when measuring ICP. Normally, intracranial pressure in infants, children and adults is measured in the supine position.
- Intracranial pressure in children is normally 3–7 mmHg. Art.
- Intracranial pressure in newborns is 1.5–6 mmHg. Art.
- Intracranial pressure in adults is 3–15 mmHg. Art.
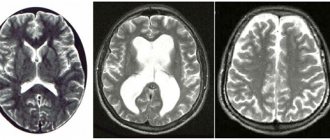
Non-invasive research methods
Non-invasive methods are used at the initial stage of diagnosis; measurements are carried out using external hardware systems. They make it possible to identify pathological changes in brain structures, as well as diagnose cranial pressure. Non-invasive techniques are safe and painless. However, the assessment of indicators is indirect, since the data obtained as a result of the examination may be mistakenly taken for signs of increased ICP, namely the expansion of the interventricular gap and the ventricles themselves. These methods are necessary to establish the reason that provoked the change in indicators.
Fundus examination is the most informative method of non-invasive monitoring of intracranial hypertension
To identify increased cranial pressure in a clinic, a specific algorithm is used, including the following methods:
- Fundus examination. Detection of swollen optic discs in the fundus and expansion of the vascular network are signs of pathology that require additional research. In the absence of pathological changes, additional techniques are not required, since ICP is within normal limits.
- Tomography, ultrasound of the brain. They allow you to determine the cause of the disorder, but do not determine the exact amount of cranial pressure.
- Electroencephalography. Determines changes in brain electrical activity, indicating an increase in ICP indicators (chaotic excitation of structural elements of the brain, formation of high-frequency rhythms, diffuse changes).
- Otoacoustic examination. The technique is carried out through the ears. With cerebral hypertension, blood pressure values in the inner ear increase.
- Transcranial Dopplerography. Blood pressure is measured by determining the decrease in blood flow velocity resulting from the development of cerebral hypertension.
The results obtained during the studies do not provide an accurate picture of the indicators of cerebral hypertension; they are used to establish the primary diagnosis of the disease.
How is intracranial pressure measured in our children now? (from open sources)
Unfortunately, there is not yet a device that can quickly measure intracranial pressure without performing surgical manipulation in the same way, for example, as a tonometer measures blood pressure.
ICP can be measured directly only by inserting a special needle with a sensor connected to a monitor into the spinal cord canal or into the ventricles of the brain. This method, of course, is used in extremely rare cases.
Therefore, increased intracranial pressure in children and adults can be indirectly judged by:
- tortuosity and dilatation of fundus veins;
- expansion of the ventricles of the brain and rarefaction of the brain substance along the edge of the ventricles (determined by magnetic resonance imaging (MRI) or computed x-ray tomography (CT));
- disruption of venous outflow from the cranial cavities (determined by ultrasound examination of blood vessels).
Intracranial pressure in infants before the fontanel closes can be measured using ultrasound of the brain. In this case, not only ICP is determined, but also the state of brain tissue and fluid. In addition, increased ICP in infants is indicated by a swollen, pulsating fontanel and, of course, symptoms.
Modern methods of treatment
In some cases, the patient does not require treatment; he is observed and treated for the underlying disease, which caused the increase in ICP.
If it is necessary to treat pathology, two approaches are used - conservative and surgical.
Conservative interventions are carried out for those patients whose ICP elevation is chronic and there is no significant deterioration of the condition over time. The basis of treatment is drugs that have a diuretic effect, which reduce the volume of fluid in the head. The specific medicine is determined by the level of pressure and the situation. In severe and acute processes, osmotic diuretics (mannitol) are used, in chronic cases - furosemide, hydrochlorothiazide, spironalactone. While taking them, you need to drink a potassium preparation - Asparkam, Potassium orotate, Panangin.
Surgical methods for treating increased ICP depend on the stage and severity of the disease. In acute situations, craniotomy is performed to reduce fluid pressure on the brain and drain excess fluid. Special shunts (tubes) are installed as planned, which drain fluid from the brain into the abdominal cavity.
Invasive methods for monitoring ICP
To accurately diagnose cerebral hypertension, invasive methods are used; they are carried out through surgery, when a special sensor is inserted into the cranial cavity through a burr hole. The procedure is carried out in a hospital equipped with the necessary equipment. During the examination, there is a high risk of injury to the brain and spinal cord, so this method is used in extreme situations that require immediate confirmation of the diagnosis.
You can measure cerebral pressure using an invasive method if you have the following indications:
- intracranial hemorrhage;
- stroke;
- hydrocephalus;
- meningitis of an infectious nature;
- posthypoxic encephalopathy.
Important! Thanks to cerebral pressure monitoring, it is possible to coordinate perfusion pressure, which reflects the effectiveness of cerebral hemodynamics, and also makes it possible to evaluate the results of decongestant therapy.
Depending on the location of the drainage system, indicators are measured using the following techniques:
- intraventricular;
- intraparenchymal;
- subdural;
- subarachnoid.
Intraventricular technique
The earliest method of cranial pressure control. The main advantage is the possibility of drainage of cerebrospinal fluid and direct endolumbar administration of medications.
External ventricular drainage
The procedure for measuring ventricular pressure is carried out using a strain gauge. The technique is easy to interpret the results and does not require the use of expensive equipment. This procedure is not only diagnostic, but also therapeutic, since it allows you to control cranial pressure by draining the cerebrospinal fluid.
Parenchema method
During the study, the sensor is installed through the trefination hole in the parenchyma of the medulla to a depth of no more than 2.5 cm. This method is preferable, since the data obtained during the study are more consistent with the readings of intraventricular pressure.
Epidural technique
Direct technique for monitoring ICP using sensors. The technique is based on the introduction of special devices into the cerebral ventricles, which make it possible to measure cerebral pressure values to set accurate pressure.
The following examination systems are used:
- Microsensory. The tensor apparatus is introduced into the required brain area, after which the information converted into electrical signals is reflected on the monitor.
- Fiber optic. Additionally, a drainage system is connected, which allows a moderate reduction in cerebral pressure values.
- Pneumatic. A catheter with a latex balloon filled with air is installed.
Reasons for development
Under normal conditions, a healthy person's brain is surrounded by intracerebral fluid. This fluid moves non-stop at a certain speed, affecting the brain with a certain level of normal pressure. At the same time, an important point to understand is the “circulation” of the cerebrospinal fluid: part of the liquid is absorbed into the blood, while new cerebrospinal fluid is produced, replacing the total volume of fluid to a normal value. If the absorption of cerebrospinal fluid slows down, or its production becomes excessively active, the volume of liquid at some point begins to exceed the norm. An obvious consequence of this will be an increase in pressure during the movement of intracerebral fluid.
Intracranial hypertension can also develop in newborns. The reason for this, as a rule, is hydrocephalus of any etiology. Among newborns with fluid hypertension in the skull, a large percentage of premature babies.
In adult patients, intracranial hypertension can develop even against the background of swelling of the brain tissue, for example, as a result of traumatic brain injury, meningitis - an infection of the meninges, sarcoidosis, or other diseases of the brain or heart.
Also, long-term use of corticosteroids, hormonal contraceptives, and antibiotics can lead to an increase in cerebrospinal fluid pressure inside the skull.