Medical editor: Druzhinkina V.Yu., neurologist. November, 2020.
Synonyms: intracranial hypertension, liquor-hypertensive syndrome, liquor hypertension syndrome, intracranial hypertension, intracranial pressure, ICP. ICD-10 code: G93.2.
Intracranial hypertension is an increase in cerebrospinal fluid pressure inside the skull. The leading symptoms are intense headaches in the frontoparietal region and a feeling of pressure on the eyeballs. The basis of therapy is the use of diuretics designed to reduce intracranial pressure due to the excreted fluid.
Intracranial hypertension is not an independent disease; it is a syndrome that accompanies a number of diseases/injuries of the skull and brain. Separately, primary or idiopathic intracranial hypertension is distinguished, the causes of which are not precisely established. This pathology is diagnosed after excluding other possible factors for increased intracranial pressure (ICP).
***
Intracranial pressure is the difference between the pressure in the skull and atmospheric pressure, that is, this term determines the force with which the intracranial fluid presses on the brain. Normal values for this difference are in the range of 5-15 mm Hg. pillar When intracranial pressure increases, they speak of intracranial or intracranial hypertension.
The brain is protected from mechanical stress and shock by the skull, as well as by a liquid medium - cerebrospinal fluid or cerebrospinal fluid. It is located in the subarachnoid, epidural spaces (cavities between the meninges) and in the cerebral ventricles (cavities located in the brain tissue). The brain, cerebrospinal fluid and intravascular blood are in dynamic equilibrium. When the pressure level of one of the components changes, the pressure in the others is transformed, which is ensured by the properties of blood and brain fluid (maintaining acid-base balance), the elasticity of the walls of blood vessels and brain tissue. When exposed to certain causes, the regulation of intracranial pressure occurs, which leads to the development of cerebrospinal fluid hypertension.
General information
Intracranial hypertension is a pathological condition (syndrome) manifested by increased intracranial (intracranial) pressure.
Intracranial hypertension syndrome (syn. liquor-hypertension syndrome) is quite common in adult and pediatric neurology and can be either idiopathic or develop with a variety of brain lesions and skull injuries. The most common cerebral hypertension of unknown origin is idiopathic (primary) intracranial hypertension (ICH), which is classified as benign intracranial hypertension (ICD-10 code: G 93.2). As a rule, this diagnosis is made only after there is no confirmation of the specific causes of hypertension (the presence of a space-occupying formation in the cranial cavity, vein thrombosis, infectious lesions of the brain, etc.).
Determination of intracranial pressure (ICP) and its physiological norm
Intracranial pressure is the difference between atmospheric pressure and pressure in the cranial cavity (epidural/subarachnoid spaces, meningeal sinuses, ventricles of the brain). The level of intracranial pressure is formed by cerebrospinal fluid (CSF) circulating in the structures of the central nervous system and arterial/venous blood entering the brain.
These fluid environments are in constant motion (spinal fluid circulates through the ventricles of the brain/spinal canal, and blood through the vascular bed). Normally, the physiology of the circulation of fluid media in the brain is determined by:
- Mean arterial pressure, i.e. the average value (difference) between the systolic/diastolic blood pressure of arterial blood entering the skull, which is normally 80 mm Hg. Art.
- The average venous pressure at the exit of the skull, which is normally 0 mm Hg. Art., that is, there is no resistance to blood flow.
- The average cerebrospinal fluid pressure in the skull, which is external in relation to the brain and is equal to 10 mm Hg. Art. It is the cerebrospinal fluid pressure that has a constant compressive effect on the brain (creates constant ICP). The biomechanical balance normally present in the skull maintains the average cerebral tissue pressure at a level of 10 mmHg. Art. In a healthy adult, the total volume of circulating cerebrospinal fluid averages 150 ml, while ICP remains normal. Its slight increase is compensated by its resorption by brain tissue and outflow from the cranial cavity to the spinal cord along the liquor subarachnoid ducts through all parts of the spine, up to the sacral outlet openings.
The constant pressure inside the cranium is maintained by the formation of reserve spaces due to a decrease in the volume of CSF, as well as the cerebral blood fraction. In cases of an increase in any of the components occurring against the background of various pathologies (excessive accumulation of CSF, cerebral edema , cerebral hyperemia , impaired venous outflow), as well as with the development of pathological volumes (tumors, hematomas, parenchymal hemorrhage, abscess), a conflict occurs between the intracranial components and hypertension develops .
An increase/decrease in ICP can be observed both during natural physiological processes in the human body ( coughing , loud screaming, sneezing , crying, straining, physical/nervous strain, sudden bending forward), and indicate pathology. Normally, in an adult, the pressure inside the skull should not exceed 10–15 mmHg. ICH refers to a persistent increase in ICP to a level of 20 mm or higher. rt. Art. The severity of intracranial hypertension is presented in the table below.
How can you measure VD?
In specialized medical institutions, invasive techniques are used to measure the pressure inside the ventricles of the brain using specialized pressure sensors that are inserted into the cerebral ventricles (a catheter is inserted and connected to the sensor). Sensors can also be installed subarachnoidally, subdurally, or epidurally. This procedure has a low risk of brain injury. In practice, intracranial pressure is in most cases measured indirectly using a spinal puncture, measuring it at the level of the lumbar spine in the spinal subarachnoid space.
Why is intracranial hypertension dangerous?
The severity and specificity of disorders in ICH are determined by the degree of increase in ICP, its nature (diffuse/local) and localization, as well as the duration of the impact of increased ICP on brain structures. And if, with a weak and unstable degree of increase in ICP, no significant changes are observed, then in patients with a stable increase in ICP of moderate and severe degrees it can cause serious disorders - headaches (tension, ischemic), disturbances in fine motor skills of the hands, vision, hearing, hypertonicity of the upper muscles / lower extremities, skeletal muscle rigidity, convulsions , paresis , disturbances in emotional manifestations (sleep, behavior), fatigue, delayed speech development, neurogenic disorders of the cardiovascular and respiratory systems (vegetative-vascular dystonia , pain in the heart, bradycardia / tachycardia , arrhythmias , low-grade body temperature , breathing rhythm disturbances - shortness of breath , apnea ) and others.
Benign intracranial hypertension
First of all, what is it? As already noted, benign ICH is a condition characterized by a persistent increase in cerebrospinal fluid pressure in the absence of intracranial mass formation, vein thrombosis and abnormalities in the composition of the cerebrospinal fluid. Since intracranial hypertension of a specific origin can be considered within the framework of a particular pathology/disease, we will consider only idiopathic (benign) ICH.
The primary syndrome of idiopathic intracranial hypertension (IIH) today means a condition that is accompanied by an increase in ICP without identified etiological factors (possibly due to obesity ). The incidence rate of IIH is 0.7–2 cases/100,000 population.
This type of hypertension most often occurs in young women who are overweight. Much less common in children and men. The most typical symptoms of idiopathic liquor hypertension are headache and transient (transient) visual disturbances in the form of deterioration in image sharpness, blurring, double vision, and in 30-35% of patients there is a decrease in visual acuity.
Diagnostics
In the diagnosis of pathology, it is important to collect the patient’s complaints and medical history, conduct a neurological (identification of pathological reflexes and symptoms) and ophthalmological examinations. When examining the fundus, dilation and tortuosity of the veins, their plethora, and swelling of the optic disc are revealed.
Instrumental research methods:
- Echoencephalography. Allows you to obtain indirect data on brain function, which should be compared with the clinical picture.
- X-ray of the skull. Signs of intracranial hypertension in the form of digital impressions on the bones of the skull.
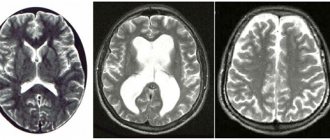
- , MRI of the brain. They allow you to evaluate the bones of the skull, brain tissue, its blood supply, identify the presence of infarctions and hemorrhages, neoplasms, expansion of the ventricles of the brain and interthecal spaces.
- Ultrasound of the head and neck vessels. Helps to establish a disorder of the venous outflow from the brain.
For idiopathic intracranial hypertension, a lumbar puncture is performed, followed by a study of the biochemical composition of the cerebrospinal fluid, in which the main indicators (electrolytes, sugar, proteins and cells) exceed the norm. A needle is inserted into the lumbar region to collect cerebrospinal fluid.
Also, the study of cerebrospinal fluid allows us to clarify the genesis of secondary intracranial hypertension (infectious, oncological, vascular).
Important! In case of acute pathology, lumbar puncture is contraindicated due to possible complications.
Differential diagnosis of primary intracranial hypertension is carried out with an epileptic seizure and toxic or metabolic dysfunction of the brain.
In epilepsy, there is a cyclical pattern of convulsive seizures, which are visible during echoencephalography. Convulsions are clonic in nature, there are sudden unstable changes in heart rate and blood pressure. Also, seizures in epilepsy are accompanied by salivation without swallowing (foaming from the mouth), and there is a history of epileptic seizures.
In acute poisoning and generalized infections, incoherent speech, confusion and disorientation, and anxious agitation are observed.
Pathogenesis
The pathogenesis of increased ICP in adults may be based on various mechanisms - edema/swelling of the brain, an increase in the mass of the contents of the cranium ( tumor , hematoma , abscess ), difficulty in the outflow of cerebrospinal fluid, disturbances in the venous outflow of the cerebral blood fraction). Within one article, it is not possible to consider the pathogenesis of high-frequency hypertension in a particular pathology, so we will only consider the pathogenesis of the development of high-frequency hypertension with cytotoxic cerebral edema .
Understanding the development of increased intracranial pressure (ICP) is based on a model of progressive cerebral edema, based on the theoretical Monroe-Kelly model, which is based on the thesis of a close relationship between the rigid cranium of an adult and components such as the brain, blood, and cerebrospinal fluid. The basis of such a connection is the interaction of any of the components with the others, manifested by a reaction to an increase in one of them by a corresponding (proportional) decrease in the volume of the other, due to which the constancy of intracranial pressure is maintained.
cytotoxic edema due to disruption of the transmembrane transport of electrolytes . Edema cells, due to their increased volume, exert a compressive effect (pressure) on neighboring cells, thereby promoting the spread of edema to intact cells (mass effect).
As the pathological volume of cells with cytotoxic edema increases, compression develops in the capillary-pial bed system, which leads to disruption of microcirculation and the development of hypoxemia / ischemia in areas of the brain that are not directly related to the primary mass effect, that is, this leads to pathological separation of different sections of the contents of the cranium. As a result, the pressure created by the pulse oscillations of the arteries and the cerebrospinal fluid loses the ability to spread freely along the tissues and spaces of the cerebrospinal fluid located inside the skull/spinal canal. This leads to the emergence of a difference in parenchymal pressure between intact and those involved in edema of the brain structures, which initiates its dislocation in the direction of relatively low pressure.
As a result of this process, diffuse edema of the entire brain develops and its gradual dislocation (movement in the direction of the foramen magnum (the only open exit from the cranium). As a result, various types of dislocation occur. More often, this is a hernial protrusion into the tentorial notch of the middle-basal parts of the temporal lobes and compression of the mesencephalic structures of the brain stem with inhibition of the primary circulatory/respiratory centers and a sharp disruption of brain function, up to the cessation of its vital activity. Neurological symptoms manifest themselves at the stages of cerebrovascular accident. The figure below shows a diagram of the progression of ICP and the stages of the cerebral protection mechanism.
Causes of development and risk factors
Due to its occurrence, intracranial hypertension is divided into:
- primary (idiopathic);
- secondary.
According to the speed of occurrence, the pathology can be
- acute, when an increase in intracranial pressure develops rapidly (brain infection, trauma, acute circulatory disorder);
- chronic - intracranial pressure increases gradually as the brain tumor grows or due to residual effects after trauma, surgery, or stroke.
An increase in intracranial pressure is facilitated by an increase in the volume of any structure that is located in the cranium (vessels, brain tissue, cerebrospinal fluid depot and the cerebrospinal fluid itself). As a result, compression of the brain occurs, which leads to metabolic disorders in its cells, displacement of brain structures and disruption of vital functions (respiratory, cardiac). This happens due to compression of the brain stem, which contains the respiratory and cardiovascular centers.
Photo: example of compression of the brain in the case of hydrocephalus
In this regard, all triggers leading to intracranial hypertension are divided into 4 groups.
Vascular pathology
Conditions that cause excessive blood filling of the brain:
- increased temperature (hyperthermia);
- hypercapnia (excess CO2, for example, in case of impaired pulmonary ventilation, poisoning with drugs, alcohol, toxic substances).
Conditions that interfere with the flow of blood from the brain:
- encephalopathy;
- cervical osteochondrosis.
Edema of the brain or its membranes
It can be diffuse (widespread) and local (local).
Observed in the following conditions:
- brain contusions;
- ischemic stroke (due to hypoxia);
- infectious diseases (encephalitis, arachnoiditis, meningitis);
- severe hypoxia caused by any pathologies;
- hepatic encephalopathy.
Volumetric formations in the skull
The most common reasons:
- brain tumor (primary or metastatic);
- cyst, including parasitic origin (echinococcosis);
- aneurysms of cerebral vessels;
- brain abscess.
Liquorodynamic disorders (cerebrospinal fluid hypertension)
May be caused by excess production of cerebrospinal fluid, impaired absorption or circulation disorders (hydrocephalus).
Factors contributing to the occurrence of primary cerebrospinal fluid hypertension have not been sufficiently studied. Most often this pathology is diagnosed in women and is caused by weight gain. Intracranial hypertension is also observed in overweight teenage girls, in the case of venous sinus thrombosis due to hemorrhagic diathesis, when taking vitamin A in increased dosages, treatment with tetracycline, penicillins or after discontinuation of glucocorticoids, with hypo- and hyperthyroidism, pregnancy, cycle disorders.
Causes
Intracranial hypertension in adults can be caused by many different causes, the diversity of which can be grouped according to the mechanism of development of the pathology:
- Intracranial space-occupying formations causing an increase in ICP ( benign/malignant tumor intracranial hematoma , parasitic cyst , abscess );
- Cytotoxic cerebral edema caused by hypoxic damage to cells of brain structures (severe respiratory failure after cardiac arrest), early stage cerebral ischemia hepatic / renal encephalopathy , hyponatremia , Reye's syndrome , syndrome of inadequate production of andidiuretic hormone ).
- Vasogenic cerebral edema caused by damage to the blood-brain barrier (infectious diseases - meningitis / encephalitis , intracranial trauma - bruises, concussions, birth injuries), hematomas , ischemic / hemorrhagic stroke .
- Interstitial edema caused by impaired outflow of cerebrospinal fluid ( occlusive hydrocephalus ).
Types of disease
Intracranial hypertension (ICP) is a disease that often occurs not only in adults, but also in children. The measure of intracranial pressure corresponds to the height of pressure in the spinal cord fluid, which is why this disease is also called cerebrospinal fluid hypertension syndrome. After head injuries or during brain diseases, hypertension is of a secondary nature. In a larger number of patients, hypertension is primary and manifests itself without visible motives - idiopathic hypertension, which is defined according to the ICD-10 classifier as benign. This diagnosis is established by a differential method of eliminating all possible causes of increased pressure inside the head.
ICP is divided into acute and chronic. The acute form occurs against the background of traumatic brain injury or infection, the chronic form occurs when vascular problems or intracerebral formations (tumors, cysts) occur. Chronic hypertension can be a side effect after brain surgery or after strokes, infections, or injuries.
Symptoms of increased intracranial pressure
Symptoms of intracranial hypertension in adults are manifested mainly by headaches of varying intensity. The pain syndrome is characterized by pronounced intensity in the morning, increased pain when tilting the head/coughing, sometimes the pain can be accompanied by nausea and, less often, vomiting.
Visual disturbances are especially characteristic of idiopathic ICH, which manifest themselves as transient darkening (fogging) of the eyes and are present in 48-55% of cases. Many patients complain of pain behind the eyeballs/pain when moving the eyeballs. Sometimes visual disturbances can be precursors to headaches. Signs of intracranial hypertension may also include complaints of noise in the head, photopsia , diplopia (double vision) and progressive decrease in vision.
Acute, rapidly increasing intracranial hypertension often leads to short-term loss of consciousness up to coma . With chronic ICH, there is a progressive deterioration in the general condition in the form of sleep disturbances, irritability, and mental/physical fatigue. Indirect signs of hypertension include increased meteosensitivity (reaction to weather changes), rapid heartbeat, increased sweating , loss of appetite , and drowsiness . The severity of clinical manifestations is largely determined by the nature/severity of the underlying disease, as well as the rate of increase in ICP.
Features of treatment of ICH in certain conditions
Corticosteroids are quite effective in reducing the degree of ICH if it is caused by a tumor process. The drug of choice is dexamethasone. It is prescribed intravenously at 4-12 mg three times a day. For ICH caused by other causes, the effectiveness of corticosteroids has not been proven.
If ICH is caused by hydrocephalus (occlusion of the cerebrospinal fluid ducts due to SAH, meningitis, brain tumors, etc.), in addition to the main therapy, furosemide 1 mg/kg or acetazolamide (Diacarb) 10-20 mg/kg per day is prescribed (the dose is divided into 3 doses ). Both drugs reduce the production of cerebrospinal fluid, which helps reduce ICP.
Dihydroergotamine, a selective venous vasoconstrictor, may be effective in people with severe cerebral congestion (brain swelling) and refractory ICH. 250-500 mcg of the drug is administered intravenously, if necessary, repeat after 1 hour, maximum dose 2 mg per day.
If symptoms of brainstem dislocation develop quickly (in minutes), you can try using hypertonic sodium chloride solution in higher doses. A quick infusion (about 10-20 minutes) of 7.5% sodium chloride solution is performed at a rate of 3-4 ml/kg. At the same time, of course, resuscitation measures continue - sedation, mechanical ventilation in hyperventilation mode, administration of vasopressors, etc.
Intracranial hypertension in children
Increased HF in infants and children of the first years of life can be caused by: unfavorable course of pregnancy (infectious diseases of the woman during this period, intrauterine hypoxia), difficult birth accompanied by birth injuries, oxygen starvation during childbirth, congenital anomalies/malformations ( hydrocephalus ), prematurity, neuroinfections, inflammatory diseases of the membranes of the brain ( encephalitis , meningitis ).
As a rule, ICH in children of the first years of life is manifested by regurgitation, general anxiety, autonomic disorders (increased sweating , marbling of the skin, etc.), sleep disturbances, rapid increase in head circumference, pulsation/tension of the large fontanel, tremor of the chin/hands, weather sensitivity, symptom Graefe (when moving the gaze downward, a lag of the upper eyelid from the iris is noted). If such symptoms are present, parents should contact a pediatric neurologist.
Treatment methods
Regular use of medications is necessary for the chronic course of the disease or during crises in the absence of deep disorders of consciousness. Depending on the level of ICP, one or another diuretic pharmaceutical is prescribed. In mild cases - furosemide, hydrochlorothiazide, spironolactone, in acute form - mannitol. Taking diuretics should be combined with potassium preparations - potassium chloride, potassium aspartate.
In the presence of concomitant infectious diseases, antiviral and antibacterial drugs are prescribed. When the body is intoxicated, detoxification measures are carried out. For venous circulation - venotonics. In conditions of ICP, nerve cells need special nutrition; for this purpose, piracetam, gamma-aminobutyric acid, and glycine are prescribed. It is advisable to undergo courses of cranio-manual therapy, which improves the outflow of venous blood. During crises, excessive strain on the eyes and emotional overload should be avoided.
Neurosurgical surgical interventions can be performed urgently or plannedly in severe forms of the disease. In acute prolonged crises, external ventricular drainage or craniotomy is indicated to reduce intracranial pressure. Removal of brain tumors, elimination of hydrocephalus, and cerebral shunting are routinely performed.
Consequences and complications
A long-term (chronic) increase in ICP, even with minor deviations from the norm, negatively affects the function of the central nervous system and is manifested by signs of nervous exhaustion: irritability , frequent headaches, sleep disturbances, increased fatigue, decreased physical/intellectual performance, decreased cognitive functions (decreased concentration, memory , weakening of intelligence). With a significant increase in ICP, there is a high risk of developing visual impairment and epileptic seizures.
List of sources
- Skvortsov I.A. Developmental neuroscience: a guide for clinicians. M.: Litterra, 2008. - 544 p.
- Bashkirov M.V., Shakhnovich A.R., Lubnin A.Yu. Intracranial pressure and intracranial hypertension // Ros. magazine anesthesiol. and intensive ter. - 1999. - No. 1. - P. 4-11.
- Krylov V.V., Talypov A.E., Puras Yu.V. Intracranial pressure in brain injuries // Neurosurgery: scientific and practical. magazine - 2007. - No. 4. - P. 12-19.
- Gasparyan S.S., Eliseeva N.M., Tanyashin S.V. Clinical recommendations. Diagnosis and treatment of benign intracranial hypertension. M. 2015. 17 p.
- Sergeev A.V. Idiopathic intracranial hypertension. Journal of Neurology and Psychiatry. S.S. Korsakov. 2016; 116(5): 93–97.
Test for suspected ICH
As noted above, the course of many diseases can be complicated by ICH and depression of consciousness. It is especially difficult to exclude intracranial hypertension if the brain damage is not focal. For example, for meningitis, liver failure, tick-borne encephalitis, post-hypoxic conditions, etc.
Unable to instrumentally control intracranial pressure, some specialists in such cases resort to a test with the administration of hyperosmolar drugs (mannitol, 3-10% sodium chloride solutions). The most commonly used dose is mannitol at a dose of 1 g per 1 kg of body, which should be administered intravenously over 20-30 minutes.
In case of unstable hemodynamics, hyponatremia, preference is given to hypertonic solutions of sodium chloride - 200 ml of 7.5% administered in approximately half an hour. The test is considered positive if the patient’s degree of depression of consciousness decreases in the next few hours.