Our clinic specializes in the diagnosis and treatment of diseases of the nervous system, incl. non-surgical treatment of increased intracranial pressure and hydrocephalus. You will also find help in treating the consequences of intracranial hypertension: depression and nervous exhaustion, vegetative-vascular dystonia, headaches, visual disorders and others. We will be happy to help you!
- Increased intracranial pressure: treatment at the Echinacea clinic with and without medications
- Make a diagnosis
- Symptoms of increased intracranial pressure
- Causes and consequences of increased intracranial pressure
- What is intracranial pressure
- What is hydrocephalus of the brain
What are the benefits of exercise therapy?
Most often, increased ICP is a symptom of serious diseases. To raise intracranial pressure, special conditions are necessary, for example, a sudden increase in the production of cerebrospinal fluid, which accompanies meningitis, encephalitis, and hydrocephalus. Intracranial hypertension is provoked by any lesions of the brain substance:
- injuries;
- tumors;
- strokes;
- abscesses.
To reduce intracranial pressure, inpatient treatment using intramuscular injections, intravenous drips, and medications is indicated. After discharge from the hospital, the patient needs clinical observation in the clinic at the place of residence. During this period, the attending physician may additionally prescribe physiotherapy, herbal remedies, self-massage, and a complex of therapeutic exercises.
Therapeutic exercise is aimed at accelerating circulation, removing congestion in the movement of various fluids in the body. Gymnastics helps reduce increased ICP and pain by improving blood dynamics and accelerating metabolic processes. Therapeutic exercise, consisting of simple elements, is prescribed by a doctor in addition to treatment with medications or for prophylaxis during remission, preventing a rise in intracranial pressure in children and adults.
The therapeutic complex of procedures includes:
- morning exercises (gives vigor and improves mood);
- walking before bed (saturate the body with oxygen and improve blood circulation);
- a special set of movements with increasing load helps reduce ICP.
Return to contents
Intracranial pressure: symptoms, causes, treatment
Many of us, as a rule, do not attach much importance to mild ailments, manifested by minor headaches, short-term and mild dizziness, and blurred vision. But all these signs are characteristic of fluctuations in intracranial pressure and may indicate severe structural damage to the brain.
Intracranial pressure is an indicator that reflects the degree of pressure of cerebrospinal fluid on the brain. This pressure depends on the amount of cerebrospinal fluid and on the quality indicators of its circulation and absorption.
Intracranial pressure is maintained through complex processes, so the symptoms of increased intracranial pressure that appear are signs of the possible onset of pathological processes that should definitely be paid attention to.
Symptoms of increased intracranial pressure in adults:
- headache - constant, throbbing, significantly worse at night and in the morning, pulsating behind the eye sockets;
- bright flashes of light, dots, double vision;
- lethargy, fatigue, nervousness;
- nausea, vomiting that does not bring relief;
- drowsiness;
- hallucinations;
- uncoordinated movements;
- heat;
- feeling of fullness in the head;
- vegetative-vascular dystonia - sweating, frequent fainting, surges in blood pressure, tachycardia, darkening of the eyes.
Possible reasons:
- genetic abnormalities;
- concussions, injuries;
- poisoning;
- circulatory disorders;
- hypoxia;
- cancer of any organs located in the skull;
- meningitis.
What to do to prevent increased intracranial pressure?
- Maintain a daily routine . It is important to alternate mental and physical activity. Night sleep should last at least 7-8 hours.
- Do physical exercise.
- Carry out therapy for the underlying disease. Main directions: fight against hypertension, atherosclerosis, hormonal disorders.
- Follow a diet. It is necessary to maintain a drinking regime - up to one and a half liters of fluid per day. Increase your intake of potassium and magnesium salts. These elements are found in buckwheat, beans, cashew nuts, dried apricots, kiwi, and seaweed. It is advisable to reduce the amount of salt, animal fat, confectionery, and alcohol. This diet helps reduce excess body weight, which prevents increased ICP.
- Stop smoking; nicotine causes vasospasm and interferes with the absorption of cerebrospinal fluid.
- Avoid overheating.
- Raise the head end of the bed by 30-40 degrees to improve venous outflow from the cranial cavity.
When suffering from headaches, many of us are accustomed to using painkillers exclusively. At the same time, forgetting that without eliminating the root cause of pain, it is impossible to get rid of them forever. The direction of treatment will directly depend on which disease is the root cause of the painful symptoms.
Which doctor should you contact if you have symptoms of intracranial pressure: first of all, consult a neurologist who will determine the causes of this disease. Further therapy will depend on the identified causes.
What exercises are good to do for intracranial pressure?
For increased intracranial pressure, the following are suitable:
- jogging;
- swimming;
- special breathing training;
- tilting and rotating the head;
- walking on all fours;
- stretching;
- body bends.
Return to contents
Tilts and head rotations
Starting position: standing or sitting. Tilt your head smoothly, first down and then up, while touching your chin to your chest; then the head is turned to the left and then to the right, alternately touching the left and right shoulders with the ears. The pace of movement is slow. Sharp intense rotations lead to cervical radiculopathy. Perform 10 times every day, 3 times.
On knees
This task is best performed in specialized physical therapy rooms. For this you will need a gymnastic bench. It is important to maintain balance when performing movements. Get on all fours and walk from the beginning to the end of the bench. At first it is recommended to perform the task 2-3 times, gradually increasing to 10 times. If it is difficult to complete a task, then you can take short breaks.
Set of movements "hedgehog"
Intracranial pressure will help normalize the hedgehog movement complex. The starting position is to lie on your back, covering your knees with your palms. Slowly bring your legs bent at the knees closer to your chest, as if a hedgehog is curling up into a ball. Then, in the reverse order, move your legs away from your chest and take the original position. Slowly raise your arms up and stretch. Initially, the task is performed 3 times, increasing over time to 10 times.
Breathing exercises
Special breathing training is necessary to relieve muscle spasms and reduce high-frequency pressure. Starting position: sit comfortably straight, inhale deeply through your nose. Hold your breath for 2-3 seconds. Curl your lips into a tube and exhale the air smoothly. It is advisable to perform it for 1 to 5 minutes, avoiding disruption of the respiratory rhythm.
Other exercises
In addition to the above training, the following manipulations will be useful:
- Starting position - sitting or standing straight, raise your shoulders, pull your head into your shoulders, stay in this position for 2-3 seconds, take the original position (20 times).
- Close eyes. Move your eyes left to right (20 times).
- Sit on the mat, take a breath. As you exhale, reach your toes with your hands (palms up) (40 times).
Return to contents
Head massage for ICP
Only a doctor can determine the severity of the condition and prescribe proper treatment. A procedure such as massage should be carried out by a qualified specialist. It is necessary to learn the basic movements and execution methods at the initial stage. Then you can perform self-massage at home. Standardly, with increased high-frequency pressure in adults, the massage therapist kneads the back of the head (if a headache occurs in the temple area, then rubbing in this area is necessary). When performing self-massage, it is convenient to place your palms on the top of your head and move the thumbs of both hands from the back of your head to your neck. The procedure is allowed to be performed daily. In addition to reducing headaches, the normal movement of cerebrospinal fluid (CSF) is stimulated.
To effectively combat high HF pressure, craniosacral therapy is used. This is manual therapy consisting of soft, light rubbing. The specialist performs various manipulations, including pressing on certain points of the head and neck, as a result of which headaches disappear, nerve function is normalized, and the general condition improves. The duration of the massage is from 30 minutes to 1 hour.
Do not forget about a balanced diet, if possible, eat dried fruits, it is advisable to limit the intake of fatty, salty, spicy foods. People with such a symptom as increased intracranial pressure should be wary of climate change, avoid stressful situations, overwork, refuse saunas, steam baths, they need a sleep and rest schedule.
ABOUT INTRACRANIAL PRESSURE IN A CHILD. TREATMENT.
We often hear the phrase “My child has ICP .” And this is a true statement - all living creatures on the planet that have a skull also have intracranial pressure. But what then worries parents of children?
The correct way to talk about the problem is increased intracranial pressure. Let’s make a reservation right away - this is not a diagnosis, but a description of one of the links in the development of many different diseases (that is, a symptom ). Intracranial pressure (ICP) increases with hydrocephalus, brain tumors, neuroinfections (encephalitis, meningitis), traumatic brain injury, intracranial hemorrhage, some rare hereditary diseases, etc.
Attention! If a child really has increased intracranial pressure, then he really needs medical help, since the question is about developmental disorders of the child in the future, and in some cases - even a threat to life!
Indirect signs of increased ICP are:
- — sleep and behavior disorders;
- - hyperactivity, attention deficit;
- — disorders of mental, speech and motor development, low learning ability;
- - “marble” skin pattern (including on the head);
- - nosebleeds;
- - “finger impressions” on a skull x-ray;
- - tremor (shaking) of the chin;
- - walking on tiptoes
The cause of the condition lies in the excessive accumulation of cerebrospinal fluid in the ventricles of the brain, where this fluid is produced, and the difficulty of its movement or absorption in the subarachnoid space.
Sometimes doctors give such children syndromic diagnoses: “hydrocephalic syndrome” , “increased intracranial pressure” , “dilatation of the ventricles of the brain” (symmetric or asymmetric), “Graefe’s symptom”, “setting sun syndrome”, “hypertensive-hydrocephalic syndrome”.
Associated symptoms are:
- non-overgrowth of fontanelles;
- drowsiness;
- noticeable squint;
- white stripe of the eyeball between the pupil and the upper eyelid;
- frequent and profuse regurgitation;
- the occurrence of seizures;
- involuntary shuddering of the whole body;
- the baby’s innate reflexes are too weak;
- decreased muscle tone;
- excessive enlargement of the skull ;
- nausea; vomit;
- dizziness;
- poor sleep;
- excessive tearfulness;
- developmental delay.
Reliable diagnostic methods for increased ICP are: ultrasound ( neurosonography ), CT and MRI of the brain.
TREATMENT OF HIGH ICP.
The choice of treatment methods depends on the severity of the disease.
Very severe forms ( hydrocephalus ) require surgical treatment with shunting to create an outflow of excess fluid. These are quite complex cases and osteopathic treatment can only be indicated after bypass surgery.
In less complex cases: traditionally, doctors prescribe diuretics, which remove fluid from everywhere, including the cerebrospinal fluid spaces. This is a nonspecific effect that is not aimed at the cause.
We set ourselves the task of normalizing the mechanisms of cerebrospinal fluid dynamics - the production and resorption of cerebrospinal fluid. This is work with the mobility of the bones of the base of the skull, which helps improve venous outflow, balance the tension of the dura mater, normalize the position and mobility of the cervical vertebrae, etc.
That is, we identify the root cause and act on it, restoring the normal physiology of the body.
Naturally, in the case of gross structural disorders, pharmacotherapy and, if necessary, surgical treatment are indicated. But if it is possible to restore normal mechanisms, this must be done.
It is important to understand that the solution to the problem does not need to be delayed or postponed, because the development of the syndrome can be prevented or reduced. It is necessary to consult a doctor - an osteopath already in the initial stages of the disease and almost always avoid serious consequences.
Gymnastics for the treatment and prevention of intracranial pressure
Intracranial pressure is an indicator that characterizes the force of cerebrospinal fluid pressure on brain tissue. Its increase indicates congenital or acquired pathologies; fluid pressure has a depressing effect on the brain matter and poses a threat to the patient’s life. Therefore, it is necessary to promptly find the cause of intracranial hypertension in order to choose an effective treatment method and thereby prevent the development of dangerous symptoms. Below we will look at gymnastics to reduce intracranial pressure as one of the effective methods of treatment.
Increased intracranial pressure: treatment at the Echinacea clinic with and without medications
We actively use methods to normalize intracranial pressure, both classically and without drugs. Some simple measures may be enough to get you back to good health. The effect is usually noticeable already in the first week of treatment.
1. Unloading the venous bed of the head using special methods of soft manual therapy and osteopathy;
Normalization of intracranial pressure: for treatment, sometimes it is enough to eliminate the infringement of blood vessels by the vertebrae
2. Special gymnastics to reduce intracranial pressure (used by the patient independently, developed by the doctor after examining muscle tone); 3. Individual drinking/eating regimen.
Living with increased intracranial pressure is both unpleasant and harmful. The human brain cannot work normally under the influence of excess pressure ; moreover, slow atrophy of the brain substance , this leads to a decrease in intellectual abilities, disruption of the nervous regulation of internal organs (hormonal disorders, arterial hypertension, etc.). Therefore, we will take measures to normalize intracranial pressure as soon as possible.
In the treatment of increased intracranial pressure, it is important to reduce the release and increase the absorption of cerebrospinal fluid. Traditionally, it is customary to prescribe for this purpose drugs that reduce the production of cerebrospinal fluid and improve venous outflow (evacuation of venous blood from the cranial cavity). Often it is enough to take the medicine 1-2 times a week.
But still, we strive to free our patients from constant medication use. There are two ways to do this:
- If possible, eliminate the cause of increased intracranial pressure and hydrocephalus;
- Use more non-drug methods for treating cerebral hydrocephalus.
What to do in very severe cases
In very severe cases (for example, cerebrospinal fluid block after neurosurgical operations or congenital cerebrospinal fluid block), surgical treatment is used. For example, a technology has been developed to implant tubes (shunts) to drain excess cerebrospinal fluid.
Reasons for increased ICP
The main cause of intracranial hypertension is a dysfunction of the cerebrospinal fluid system, in which cerebrospinal fluid is released in excess, is slowly absorbed into the brain tissue, or poorly circulates through the spinal vessels due to their low tone.
There are many reasons that cause dysfunction of the cerebrospinal fluid system and increased ICP:
- congenital brain pathologies; birth injuries; TBI; brain infection (encephalitis, meningitis); cervical osteochondrosis; hydrocephalus; oncological diseases, hematomas and abscesses of brain tissue.
If acute symptoms of intracranial hypertension occur and its cause is identified, the patient is prescribed treatment and preventive measures are prescribed to increase the period of remission.
Causes and consequences of increased intracranial pressure
The reasons we find most often:
- disruption of the outflow of venous blood from the cranial cavity
- hypoxia (oxygen starvation)
- suffered a traumatic brain injury (even a very old one, up to birth trauma)
- meningitis or encephalitis
- congenital structural features of the central nervous system (Arnold-Chiari anomaly, congenital intracranial hypertension, etc.);
- poisoning with brain damage.
Consequences As a result of the disease, brain cells are gradually destroyed, and their place is filled with fluid. The functions of systems controlled by the brain become disordered, and complete or partial loss of vision, hearing, memory, potency, miscarriage, depression, nervous exhaustion and other health problems may occur.
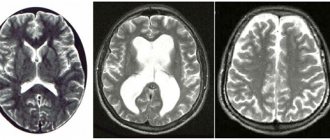
On the left is a normal brain, the liquid (cerebrospinal fluid) is indicated in white. On the right is untreated internal hydrocephalus: brain atrophy, almost the entire cranial cavity is occupied by fluid.
Treatment options for intracranial hypertension
With increased ICP, it is extremely important to start treatment in a timely manner to prevent the pressure of the cerebellar fluid on the cerebellum and the development of life-threatening pathologies. In accordance with the diagnosis, age and condition of the patient, a highly specialized specialist prescribes one or more treatment methods:
- Drug therapy. To reduce the production of cerebrospinal fluid and reduce its pressure on the brain, the patient is prescribed a complex of drugs: diuretics, neuroprotective, glucocorticosteroids, nootropic and sedative drugs, as well as injections or tablets that increase vascular tone. Surgery. If ICP is high and drug treatment fails, the patient undergoes one of the following operations: bypass surgery, endoscopy, decompression craniotomy, or ventricular puncture, which involves pumping out accumulated fluid. Physiotherapy. It is an auxiliary treatment method that complements drug therapy. A number of procedures are prescribed by the doctor in accordance with the indications. Folk remedies. They are used as adjuncts to drug treatment or to prevent exacerbations and increased brain pressure during remission. Folk remedies include herbal decoctions, tinctures, inhalations and aromatherapy. Unconventional treatment. Includes the use of acupuncture, manual therapy, hydrotherapy, and homeopathy. In a specific situation, the attending physician decides on the advisability of carrying out these procedures and the choice of treatment method - auxiliary or alternative. Therapeutic exercises to reduce intracranial pressure. A set of specially designed exercises helps reduce ICP and pain by improving blood circulation through the venous vessels. The doctor may prescribe therapeutic exercises consisting of simple elements in addition to drug therapy, instead of certain medications, or as a preventive measure that prolongs the period of remission and prevents increases in brain pressure.
Treatment of intracranial hypertension, regardless of its cause, requires an integrated approach, so the doctor, in accordance with the diagnosis, selects the most effective methods and forms them into a single technique.
Idiopathic intracranial hypertension
Introduction Idiopathic intracranial hypertension (ICH) is a disease of unknown etiology that predominantly affects obese women of childbearing age. The primary problem is chronically elevated intracranial pressure (ICP ), and the most important neurologic manifestation is papilledema , which can lead to secondary progressive optic atrophy, vision loss, and eventual blindness.
Although idiopathic intracranial hypertension and benign intracranial hypertension are synonymous in the literature, the former designation is preferable.
Signs and Symptoms Patients with ICH typically present with the following symptoms associated with increased ICP and papilledema. Symptoms of ICH may include the following:
- Headaches (usually nonspecific, with varying type, location and frequency of manifestation);
- Deterioration of vision (the visual field usually suffers, but loss of visual acuity rarely occurs);
- Diplopia (usually horizontal due to palsy of the sixth pair of cranial nerves, but rarely vertical);
- Pulsating ringing in the ears;
- Radicular pain (usually in the arms, a rare symptom).
Rarely, patients with elevated ICP and papilledema may not exhibit any symptoms. Visual symptoms of papilledema may include the following:
- Temporary deterioration of vision, usually when moving to a horizontal position;
- Progressive loss of peripheral vision in one or both eyes (due to nerve damage and enlargement of the blind spot);
- Blurring and distortion (metamorphopsia) of central vision due to macular edema or optic neuropathy;
- Sudden loss of vision (for example, with fulminant ICH).
Nonspecific symptoms of ICH may include dizziness, nausea, vomiting, photopsia, and retrobulbar pain. The most significant physical symptom is bilateral papilledema , secondary to increased ICP. Rarely, in more severe cases, macular (central) vision may deteriorate. Significant symptoms also include palsy of the sixth pair of cranial nerves . Poor prognostic signs are atrophic swelling of the optic nerve along with subretinal effusion . Untreated papilledema leads to progressive loss of peripheral vision and damage to nerve fibers. Rarely, sudden loss of central vision is caused by ischemic optic neuropathy or vascular occlusion. Visual function tests are the most important neurological examination for the diagnosis and follow-up of patients with ICH. Such tests include:
- Ophthalmoscopy, photography of the optic nerve and, in some cases, optical coherence tomography;
- Formal visual field assessment;
- Examination of eyeball mobility.
Diagnosis Typically, laboratory tests are not mandatory, but some authors recommend blood tests depending on the clinical picture, including the following tests:
- Detailed blood test;
- Electrolytes, bicarbonates;
- Complete procoagulant profile (only in patients with a previous medical history including thrombosis or MRI findings indicating dural sinus occlusion on magnetic resonance venography).
Neuroimaging studies are necessary to rule out the possibility of brain damage before performing a lumbar puncture. In addition, it is important to exclude the possibility of dural sinus thrombosis. As a result, the most preferred method is MRI of the brain with contrast (for example, gadolinium). At least early in the patient's evaluation, a CT scan can be performed to rule out brain damage if an MRI is not available.
Once brain damage has been ruled out, the patient is usually prescribed a lumbar puncture, which includes the following tests:
- detection of increased cerebrospinal fluid pressure,
- number of leukocytes,
- number of red blood cells,
- total protein,
- quantitative protein electrophoresis,
- glucose level
- the presence of an aerobic bacterial culture,
- presence of acid-fast bacilli,
- cryptococcal antigen (especially in patients with HIV),
- markers of syphilis (for example, rapid plasma reagin),
- tumor markers and cytology (in patients with a history of cancer or clinical features suggestive of malignancy).
Management of patients with ICH
The goal of therapy is to preserve optic nerve function while treating ICP . Pharmacological therapy may be as follows:
- Acetazolamide (the most effective drug for reducing ICP) and furosemide, less often other diuretics;
- To prevent headaches - amitriptyline, propranolol, other anti-migraine drugs, or topiramate;
- Corticosteroids to reduce ICP in ICH of inflammatory etiology or as an additional agent during acetazolamide therapy.
As a rule, corticosteroid therapy is used only on a short-term basis and only in patients with severe loss of visual function, since in the long term, corticosteroids can cause weight gain and forced cessation of their use in therapy.
If visual function deteriorates with the best possible medical therapy described above, surgical intervention . These could be:
- Excision of the optic nerve sheath, a necessary measure to decompress the fluid surrounding the nerve;
- Installation of a lumboperitoneal or ventriculoperitoneal shunt;
- Stenting of the intracranial venous sinus.
Treatment of ICH with repeated lumbar punctures is interesting for us only in the historical aspect, since the volume of cerebrospinal fluid is quickly restored. However, in some cases, when patients refuse or for some reason cannot undergo surgical therapy, lumbar puncture is applicable (for example, pregnant women). In particular, the use of lumbar puncture can be used in cases where ICP increases rapidly and measures need to be taken before surgery is possible.
Meta-analyses comparing these methods report the following:
- 252 optic nerve sheath decompression surgeries: visual defects improved or eliminated in 80% of cases.
- 31 operations to install a ventriculoperitoneal shunt: visual defects were improved or eliminated in 38.7% of cases.
- 44 operations to install a lumboperitoneal shunt: visual defects were improved or eliminated in 44.6% of cases.
- 17 operations for the installation of intracranial venous stents: visual defects improved or were eliminated in 47% of cases.
Of course, there are different benefits and risks associated with each of these interventions. In the long term, the mainstay of treatment for patients with ICH is weight loss. Restriction of physical activity is not required; on the contrary, a diet in combination with an exercise program is highly recommended.
Some patients with ICH show significant improvement with bariatric surgery (the branch of surgery that treats obesity).
Source
Idiopathic Intracranial Hypertension (IIH) [Electronic resource]. – Access mode: https://emedicine.medscape.com/article/1214410-overview, free. - Cap. from the screen.
Gymnastics for the treatment of intracranial pressure
Therapeutic exercises for ICP can act as both an alternative to some medications for drug treatment, and an effective preventive measure to reduce the risk of attacks. Depending on the diagnosis, the doctor selects techniques that are aimed at normalizing ICP, alleviating the general condition and reducing headaches.
The most common exercises in therapeutic exercises for intracranial hypertension:
- Using smooth movements, tilt your head to the right and left, touching your ears to your shoulders, forward and back, pulling your chin to your chest. After this, you should slowly rotate your head in both directions. Each element of the exercise is performed on average 20 times. In the first days, pain may occur due to tension in the neck muscles, but subsequently, when performing this exercise, the discomfort will disappear.
- Place both hands behind the neck and clasp the lower part of the back of the head with them so that the thumbs are on the neck muscles located at the level of the earlobes. After this, you need to run your fingers up and down over the neck muscles for 15 minutes to provoke the outflow of blood from the brain. This exercise allows you to feel instant relief in your temples and back of your head.
- Take a small round stick in both hands, place it behind your head, and with light pressure for 15 minutes, move it from the lower part of the back of the head along the neck muscles located to the right and left of the vertebrae, and back.
- Do slow stretches every morning and evening to activate muscle function throughout the body and normalize blood circulation.
- To reduce ICP and headaches, perform breathing exercises. To do this, you need to sit up straight, inhale through your nose, and hold your breath for a few seconds. Exhale slowly through pursed lips. The duration of the exercise is several minutes, and you need to carefully observe your own sensations.
Cranial therapy
In the treatment of ICP, cranial therapy is considered one of the most effective types of alternative medicine. Despite the fact that the bones of the skull of an adult are fused, they have elastic sutures, due to which their amplitude movement occurs. Violation of their mobility leads to tension in the lining of the brain and, as a consequence, the development of intracranial hypertension as a symptom of pathological processes.
The technique of cranial therapy involves diagnosing the condition of the sutures and the location of the bones of the skull, the symmetry of both of its parts, and subsequent treatment if their mobility is impaired.
A session lasting from 30 to 60 minutes is conducted by a chiropractor. By placing the palms of his hands on the patient’s head, the specialist studies his cranial rhythm and, with soft, gentle movements, normalizes the tense tissues. For this, the most effective unfolding technique is used. The procedure resembles a light and pleasant stroking of the head, from which the patient feels relief and relaxes so much that he can fall asleep.
Cranial therapy can reduce intracranial hypertension by improving the circulation of cerebrospinal fluid, get rid of attacks of severe headaches, normalize blood circulation throughout the body and alleviate post-traumatic conditions associated with the brain. The procedure is painless, does not cause complications or side effects, therefore, after consultation with a doctor, it can be prescribed to both adults and children.
Describe your problem to us, or share your life experience in treating the disease, or ask for advice! Tell us about yourself right here on the site. Your problem will not go unnoticed, and your experience will help someone! Write >>
Cranial therapy is not recommended for patients with infectious diseases, acute thrombosis, aneurysms or malignant tumors.
The information on the site is created for those who need a qualified specialist, without disturbing the usual rhythm of their own lives.
Prevention of intracranial pressure with gymnastics - what the doctor didn’t tell you
The brain is located in a special liquid environment called the fluid space or cerebrospinal fluid. Inside it contains cavities - ventricles, through which this cerebrospinal fluid regularly circulates. The cerebrospinal fluid is under pressure, which is why when it begins to put pressure on the brain, intracranial pressure occurs.
Various gymnastic exercises can be done independently
For the brain to function properly, it requires normal pressure, but due to destabilization of the cerebrospinal fluid, a person begins to experience headaches. Low and high intracranial pressure can occur in adults and children. The difficulty is that it is almost impossible to install it at home, because a headache can start due to many reasons.
With any illness, a serious disease is formed, called either intracranial hypertension or hypotension. Both have unpleasant consequences. With normal pressure in the brain, the vessels are in good shape and are able to regulate blood flow. Otherwise, due to their narrowing or expansion, the patient may experience strong pulsation in the head.
Intracranial pressure disorders
The relative closedness of the cranial cavity leads to the fact that a decrease or increase in the volume of its contents is accompanied, respectively, by intracranial hypotension or hypertension. With intracranial hypotension, the cerebrospinal fluid pressure is below 100 mm of water column, with hypertension – above 180–200 mm of water column.
1) Intracranial hypotension. It occurs for a number of reasons. The main one is the leakage of cerebrospinal fluid, or liquorrhea (Latin liquor - liquid; Greek rheo - flow), with fractures of the skull bones.
Especially often, liquorrhea occurs with fractures of the ethmoid bone and the pyramid of the temporal bone, as well as the bones of the base of the skull, in which both layers of the dura mater are torn, followed by the leakage of cerebrospinal fluid through the nose. With a fracture of the ethmoid bone, liquorrhea from the nose is observed. When the pyramid of the temporal bone is fractured, cerebrospinal fluid penetrates into the tympanic cavity of the middle ear. If the eardrum is damaged, cerebrospinal fluid leaks from the ear. If it is intact, the cerebrospinal fluid enters the Eustachian (auditory) tube, which connects the middle ear cavity with the nasopharynx. From the auditory tube, the cerebrospinal fluid enters the nasopharynx, and is then released through the nose and partially swallowed.
Another cause of liquorrhea is medical manipulation: removal of a significant amount of cerebrospinal fluid during puncture of the ventricles of the brain or liquor tanks, as well as a technical error, that is, damage to the dura mater with a needle that is too thick. The danger of liquorrhea is that the risk of infection of the brain and its membranes increases significantly.
With intracranial hypotension, the state of the subarachnoid space surrounding the brain—the cerebrospinal fluid “cushion”—changes. In this case, a change in the tension of the vessels and nerves that perform the function of “anchor” formations occurs, as well as irritation of the meninges.
Clinical manifestations of liquor hypotension:
- persistent diffuse headache occurs, especially intense in the back of the head (“drainage” or “puncture” headache, if it is associated with cerebrospinal fluid sampling);
- headache intensifies with rapid turns of the head, walking (“every step hits the head”), moving from a horizontal to a vertical position;
- headache is often accompanied by nausea, vomiting, unsystematic dizziness (uncertainty when standing, moving), and a feeling of “fog” before the eyes. If the patient lies in bed for some time with the leg raised, the headache decreases;
— lethargy, apathy, increased fatigue, impaired concentration, and a tendency to increase heart rate (up to 85–100 beats per minute) are also characteristic;
- mild signs of meningeal syndrome may be detected - “meningism” (the term indicates irritation of the meninges of non-inflammatory etiology).
Treatment of cerebrospinal fluid hypotension: bed rest, avoidance of physical activity, drinking plenty of fluids, elimination of the dural defect.
2) Liqueur hypertension. It occurs when the total volume of tissue located in the cranial cavity increases. This occurs for various reasons: cerebral edema, venous congestion, hydrocephalus, space-occupying processes (tumor, abscess, parasitic cyst, infectious granuloma, etc.), various damage to the brain and its membranes (meningitis, encephalitis, arachnoiditis, traumatic brain injury, eclampsia pregnant women, status epilepticus), hyponatremia with the flow of water from the blood into the brain tissue, hypoxia, intoxication. With craniostenosis and depressed fracture of the bones of the calvarium, a decrease in the volume of the cranium is observed.
There are two stages of development or existence of intracranial hypertension.
1. The compensated stage is a condition in which the increase in the total volume of intracranial tissue is compensated by a decrease in the amount of blood and cerebrospinal fluid. In this case, the blood moves from the vessels of the cranial cavity to the reserve vascular spaces, and the cerebrospinal fluid begins to be intensively absorbed and/or its secretion slows down. This stage does not manifest itself clinically.
2. When reserve capacity is depleted, the 2nd stage occurs - decompensation of intracranial hypertension with characteristic and increasing symptoms. Cerebral circulation is impaired, as perfusion pressure in the vessels of the brain drops (it is defined as the difference between mean arterial pressure and intracranial pressure). If the perfusion pressure is below 50 mm Hg. Art., the stage of decompensation begins - arterial blood flow becomes insufficient. When the difference becomes zero, it stops completely.
Clinical picture of intracranial hypertension (ICH):
— at the beginning of the development of ICH it is characterized mainly by paroxysmal headaches, which occur and are most intense more often in the mornings;
- then an increasing diffuse headache of a bursting nature joins. It intensifies with coughing, sneezing, physical stress, moving the head, flexing and straightening the neck, squeezing the veins in the neck;
- “cerebral” vomiting not associated with food intake is observed;
- swelling of the optic discs appears, fraught with secondary atrophy of the optic nerves and loss of vision;
— the most severe complication of intracranial hypertension is the displacement and herniation of brain structures into the cracks between the sheets of the dura mater.
Return to Contents
Causes of increased pressure
When a headache occurs, the patient takes a painkiller, and if it works, the illness is successfully forgotten. However, this is a fundamentally wrong action, since it is important to establish the cause of the headache. In most cases, it is caused by increased intracranial pressure when there is an excess of cerebrospinal fluid (CSF). The reasons for this phenomenon include:
- consequence of head injury;
- constriction of blood vessels in the brain;
- impaired circulation of cerebrospinal fluid;
- inflammation of the brain;
- taking potent hormonal drugs;
- hydrocephalus.
The last point can be noted additionally. When intracranial pressure is elevated for a long time, the cerebral ventricles greatly expand, which leads to hydrocephalus - dropsy. The skull has a closed shape, so the expansion of the ventricle is carried out due to the contraction of the medulla. This is what has serious consequences.
What is intracranial pressure
Wise nature placed the human brain in a protective liquid environment ( subarachnoid fluid spaces ) and provided it with internal fluid cavities ( ventricles ). Thus, the brain is actually suspended in a special fluid - cerebrospinal fluid (also known as cerebrospinal fluid or CSF ). The cerebrospinal fluid is in the cranial cavity under a certain pressure. It is the pressure of the cerebrospinal fluid on the brain that is called intracranial pressure .
A normal level of intracranial pressure is very important for the proper functioning of the brain and all processes subordinate to it. We often see a total improvement in the well-being of our patients as intracranial pressure normalizes.
What is increased intracranial pressure? All fluid spaces and ventricles are interconnected by ducts. The liquor is constantly circulating. In some parts of the brain it is released, and then flows through the cerebrospinal fluid ducts to other parts of the brain, where it is absorbed into the bloodstream. Complete renewal of the cerebrospinal fluid occurs on average 7 times a day. Excessive accumulation of cerebrospinal fluid causes an increase in its pressure on the brain substance. This is called increased intracranial pressure (intracranial hypertension).
Three common causes of chronic increased intracranial pressure:
- too much cerebrospinal fluid is released;
- the cerebrospinal fluid is not absorbed fully enough;
- the patency of the cerebrospinal fluid circulation pathways is impaired.
Symptoms and diagnosis
This phenomenon is often accompanied by the following symptoms:
- “Heavy” headache in the morning, often developing into an unpleasant throbbing.
- Fast fatiguability.
- State of fainting.
- Dizziness and poor coordination.
- Frequent heartbeat.
- High blood pressure.
- Dark circles under the eyes.
- Nausea, urge to vomit.
- A sharp deterioration in condition when weather conditions change.
- Nervousness.
Since intracranial pressure may be caused by some disease, it is worth noting that if one of the signs is observed, coupled with an increase in temperature (more than 38 degrees) and clouding of consciousness, then most likely these are the consequences of meningitis.
Symptoms of increased intracranial pressure
Increased pressure on the brain substance can disrupt the functioning of the central nervous system. Hence the characteristic symptoms:
- Heaviness in the head or headaches that increase in the morning or in the second half of the night;
- In severe cases, nausea and/or vomiting in the morning may occur;
- Vegetative-vascular dystonia (sweating, a drop or increase in blood pressure, palpitations, lightheadedness, etc.) is an almost obligatory symptom;
- Fatigue, “dullness”, easy exhaustion during work or study loads;
- Nervousness;
- “Bruises” under gases (if you stretch the skin under the eyes in the area of the “bruise”, dilated small veins are visible);
- Possible decrease in sexual desire and potency;
- If the human body is in a horizontal position, cerebrospinal fluid is released more actively and absorbed more slowly, so intracranial pressure and its symptoms tend to peak in the second half of the night or in the morning;
- The lower the atmospheric pressure, the higher the intracranial pressure, so the deterioration of the condition is associated with changes in weather.
Exercises
How to relieve intracranial pressure at home?
“By following a special technique, you can achieve positive results within a week. All elements of gymnastics should be done very carefully! No sudden movements, jerks or turns. Only neat and smooth movements.”
In some cases, you can ask another person to do certain movements for greater effect:
- Cervical massage: in the lower part of the back of the head (approximately at the level of the earlobes) there are two small bulges. You can feel them, clasp the back of your head with both hands. Your thumbs will rest against these neck muscles. You need to move your thumbs from top to bottom along the bulges for 15 minutes. You will immediately feel lightness in the back of your head and temporal lobes. This is caused by blood flowing away from the brain.
- Bend-overs: These exercises should be done as often as possible. At first it will be difficult, but soon, when the muscles are well warmed up, the movements will seem easy. It is necessary to alternately tilt the head back and forth, left and right. It is advisable to touch your chin to your chest and your ears to your shoulders. Each tilt is done slowly, without jerking. Enough 20 times per side. It is also necessary to do rotations in different directions.
- Massage with a stick: for this exercise you will need a rolling pin or any short round stick. Holding with both hands, you need to move the stick from top to bottom along the neck. You should start from the end of the head to the first protruding vertebra.
- Walking on all fours: This is a physical therapy exercise. Standing on all fours, you need to walk on a narrow bench for 10 minutes. You can lay a narrow (no more than 30 cm) path on the floor and try not to go beyond.
- Breathing exercises: proper breathing can relieve pain (during childbirth or strenuous exercise), muscle spasms, and also normalize intracranial pressure. Sitting straight, you need to take a deep breath and hold your breath for a couple of seconds. Then exhale slowly through your lips with a straw. It turns out to be a slight whistle. You should be extremely careful with breathing exercises. 2-3 minutes of exercise is enough.
- Stretching: Every morning and before bed, you need to stretch your muscles thoroughly. This will improve blood circulation throughout the body.
Cranial therapy
Cranial therapy is a type of alternative medicine that is aimed at reducing intracranial pressure. The therapy has a unique technique: thanks to a special effect on the cranial bones, the regulation of the cerebrospinal fluid is normalized, and the blood flow is stabilized.
Cranial therapy consists of several special techniques. For example, the popular “unfolding” is aimed at relaxing soft tissues. After it, the patient plunges into a state of relaxation and enjoys lightness in the head area. This therapy is very effective and absolutely safe. It is carried out only in specialized centers. But that is another story.