Patients who are forced to constantly take blood thinners are required to monitor their blood clotting abilities. This is necessary not only to assess the effectiveness of treatment, but also allows you to select an adequate dose of funds. In the same way, a person can be protected from an overdose of anticoagulants, preventing the development of corresponding complications against this background. One of the modern methods of such control is INR (international normalized ratio).
INR blood test - what is it?
An INR analysis paired with another indicator called PTI shows the quality of functioning of the blood coagulation system. INR is the international normalized ratio, it is a coagulogram that is calculated using a special formula, it includes the PTI value. PTI – prothrombin index. It shows how long it will take for a patient's blood sample to clot. This value is compared with the established norm, and the percentage of the result obtained to the standard is calculated.
INR, in turn, is calculated from the ratio of the prothrombin index to the standard value of this indicator, and the result is multiplied by the international sensitivity index, which, in turn, is also a given standard.
Together, all these indicators help the doctor understand at what speed the patient’s blood is clotting, whether there is pathology, and in what doses therapy is required for cardiovascular diseases.
A coagulogram is a study of the hemostatic system that allows you to evaluate the external and general pathways of blood coagulation and identify the risk of hypercoagulation (excessive clotting) or hypocoagulation (bleeding).
Synonyms Russian
Hemostasiogram: prothrombin index (PI), prothrombin time (PT); international normalized ratio (INR); factor I (first) of the plasma coagulation system.
English synonyms
Coagulation studies (coagulation profile, coag panel, coagulogram): Prothrombin time (Pro Time, PT, Prothrombin time ratio, P/C ratio); International Normalized Ratio (INR); Fibrinogen (FG, Factor I).
Units
% (percent), sec. (second), g/l (grams per liter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress and do not smoke for 30 minutes before the test.
General information about the study
The hemostasis system consists of many biological substances and biochemical mechanisms that ensure the preservation of the liquid state of the blood and prevent and stop bleeding. It maintains the balance between blood clotting and anti-clotting factors. Significant disturbances in the compensatory mechanisms of hemostasis are manifested by processes of hypercoagulation (excessive thrombus formation) or hypocoagulation (bleeding), which can threaten the patient’s life.
When tissues and blood vessels are damaged, plasma components (clotting factors) participate in a cascade of biochemical reactions, which results in the formation of a fibrin clot. There are internal and external pathways of blood coagulation, which differ in the mechanisms that trigger coagulation. The internal pathway is realized when blood components come into contact with the collagen of the subendothelium of the vessel wall. This process requires coagulation factors XII, XI, IX and VII. The extrinsic pathway is triggered by tissue thromboplastin (factor III) released from damaged tissues and the vascular wall. Both mechanisms are closely interrelated and from the moment of formation of active factor X they have common paths of implementation.
The study of indicators such as PTI (prothrombin index) and INR (international normalized ratio) allows us to assess the state of the external coagulation pathway. PTI is calculated as the ratio of the standard prothrombin time (the clotting time of control plasma after the addition of tissue thromboplastin) to the plasma clotting time, expressed as a percentage. INR is a prothrombin test standardized in accordance with international recommendations. It is calculated by the formula: INR = (patient prothrombin time / control prothrombin time) x MICH, where MICH (international sensitivity index) is the sensitivity coefficient of thromboplastin relative to the international standard. INR and PI are inversely proportional indicators, that is, an increase in INR corresponds to a decrease in the patient’s PTI and vice versa.
Reference PTI values depend on the set and characteristics of the reagents and differ in the activity of thromboplastin used in the test. The results of INR determination, thanks to standardization, make it possible to compare the results of different laboratories.
Tests for PTI (or a similar indicator - prothrombin according to Quick) and INR in a coagulogram help to identify disorders in the external and internal blood coagulation pathways associated with a deficiency or defect of fibrinogen (factor I), prothrombin (factor II), factors V (proaccelerin) , VII (proconvertin), X (Stewart-Prower factor). With a decrease in the concentration of these coagulation factors in the blood, the prothrombin time increases in relation to control laboratory parameters.
Plasma factors of the extrinsic coagulation pathway are synthesized in the liver. For the formation of prothrombin and some other coagulation factors, vitamin K is required, the deficiency of which leads to disturbances in the cascade of reactions and prevents the formation of a blood clot. This fact is used in the treatment of patients with an increased risk of thromboembolism and cardiovascular complications. Thanks to the prescription of the indirect anticoagulant warfarin, vitamin K-dependent protein synthesis is suppressed. PTI (or Quick prothrombin) and INR coagulation are used to monitor warfarin therapy in patients with factors that promote thrombosis (eg, deep vein thrombosis, presence of prosthetic valves, antiphospholipid syndrome).
Normally, a coagulogram in a healthy person has an INR in the range of 0.8-1.2; in patients being treated with indirect anticoagulants to prevent thromboembolic complications - 2.0-3.0, in patients with prosthetic valves and antiphospholipid syndrome - 2.5-3.5.
Simultaneous determination of fibrinogen in a coagulogram allows a comprehensive assessment of the state of the plasma hemostasis system.
Fibrinogen is blood clotting factor I, which is produced in the liver. Thanks to the action of the coagulation cascade and active plasma enzymes, it is converted into fibrin, which is involved in the formation of a blood clot and thrombus. Fibrinogen deficiency can be primary (due to genetic disorders) or secondary (due to excessive consumption in biochemical reactions), which is manifested by impaired formation of a stable blood clot and increased bleeding.
Fibrinogen is also an acute phase protein. Its concentration increases in the blood during diseases accompanied by tissue damage and inflammation. Determining the level of fibrinogen is important in the diagnosis of diseases with increased bleeding or thrombosis, as well as for assessing the synthetic function of the liver and the risk of cardiovascular diseases with complications.
What is the research used for?
- For a general assessment of the blood coagulation system.
- For the diagnosis of disorders of the external and general pathways of blood coagulation.
- To study the activity of coagulation factors I, II, V, VII, X.
- To monitor the patient's condition when prescribing anticoagulants.
- To assess the risk of cardiovascular complications.
- To assess the protein-synthesizing function of the liver (synthesis of blood clotting factors).
When is the study scheduled?
- With a comprehensive examination.
- When planning surgical interventions.
- When examining patients with nosebleeds, bleeding gums, blood in the stool or urine, hemorrhages under the skin and in large joints, chronic anemia, heavy menstrual flow, sudden loss of vision.
- When examining a patient with a history of episodes of thrombosis.
- With a hereditary predisposition to disorders of the hemostatic system.
- With a high risk of cardiovascular complications and thromboembolism.
- Before prescribing anticoagulants.
- When monitoring the hemostatic system while taking anticoagulants.
- For liver diseases.
What do the results mean?
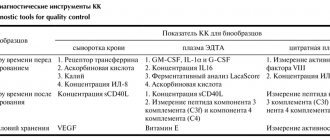
Reference values (table of normal coagulogram indicators)
- Prothrombin according to Quick: 70 - 120%.
- INR
| Age | Reference values |
| Less than 3 days | 1,15 — 1,35 |
| 3 days – 1 month | 1,05 — 1,35 |
| 1 month – 1 year | 0,86 — 1,22 |
| 16 years | 0,92 — 1,14 |
| 6 – 11 years | 0,87 — 1,20 |
| 11 – 16 years | 0,97 — 1,30 |
| More than 16 years | 0,8 — 1,2 |
| Week of pregnancy | Reference values |
| 13-21st | 0,56 — 1,1 |
| 21st-29th | 0,5 — 1,13 |
| 29-35th | 0,58 — 1,17 |
| 35-42nd | 0,15 — 1,14 |
- Fibrinogen: 1.8 - 3.5 g/l.
| Week of pregnancy | Reference values |
| 1-13th | 2.12 - 4.33 g/l |
| 13-21st | 2.9 - 5.3 g/l |
| 21st-29th | 3 - 5.7 g/l |
| 29-35th | 3.2 - 5.7 g/l |
| 35-42nd | 3.5 - 6.5 g/l |
Reasons for an increase in INR and a decrease in the level of prothrombin according to Quick (indicates a possible deficiency of factors in the external hemostasis pathway and a tendency to increased bleeding):
- DIC syndrome (disseminated intravascular coagulation) during the period of hypocoagulation;
- hypofibrinogenemia (factor I deficiency);
- dysfibrinogenemia (synthesis of a defective protein that is unable to participate in the cascade of biochemical reactions);
- hereditary or acquired deficiency of factors II, V, VII;
- Factor X deficiency (eg, purpura due to amyloidosis);
- vitamin K deficiency;
- hemorrhagic disease of newborns;
- malabsorption with impaired fat absorption (due to celiac disease, chronic diarrhea);
- acute leukemia;
- antiphospholipid syndrome;
- congestive heart failure;
- liver pathology (hepatitis, cirrhosis, alcoholic liver disease);
- obstruction of the biliary tract, obstructive jaundice;
- pancreas cancer;
- Zollinger-Ellison syndrome (pancreatic adenoma);
- toxic shock syndrome;
- nephrotic syndrome (excessive urinary excretion of factors V and VII);
- oral anticoagulants (warfarin).
Causes of increased fibrinogen levels (indicates an increased risk of blood clots and cardiovascular complications):
- acute infection (eg pneumonia, tuberculosis);
- autoimmune diseases (rheumatoid arthritis, reactive arthritis);
- acute coronary syndrome, myocardial infarction;
- burns;
- cancer (breast, kidney, stomach);
- multiple myeloma;
- Hodgkin's disease (lymphogranulomatosis);
- glomerulonephritis, nephrotic syndrome, nephrosis;
- pregnancy;
- eclampsia;
- cerebrovascular disease, stroke;
- hepatitis;
- postoperative period;
- rheumatic fever;
- tissue damage.
Reasons for a decrease in INR and an increase in prothrombin according to Quick (indicates a tendency to form blood clots):
- DIC syndrome (period of hypercoagulation);
- deep vein thrombosis (initial stages);
- polycythemia;
- pregnancy (last months);
- increased activity of factor VII.
Reasons for decreased fibrinogen levels (may indicate an increased risk of bleeding):
- dysfibrinogenemia;
- hereditary afibrinogenemia;
- DIC syndrome;
- fibrinolysis;
- hemophilia A and B;
- liver pathology (hepatitis, cirrhosis);
- abortion;
- premature placental abruption;
- late stage of cancer;
- embolism (amniotic fluid, meconium, fat, tissue);
- anemia;
- eclampsia;
- leukemia;
- malabsorption;
- shock;
- sepsis;
- post-transfusion reactions.
What can influence the result?
- Factors that distort the result of the analysis: the presence of lupus anticoagulant in the blood (directly inhibits coagulation factors);
- transfusion of donor blood components in the last month (distorts the fibrinogen indicator).
- drinking alcohol, fatty foods;
- excess intake of vitamin K from food (found in beef or pork liver, green tea, broccoli, chickpeas, cabbage, turnips, soy, green leafy vegetables);
INR norm
Units are used to express INR. The higher the INR, the less blood contains prothrombin and other factors that affect coagulation. The INR of a healthy person ranges from 0.85 units. up to 1.37 units. At the same time, the patient’s age affects the values of the norms:
- Newborns and children of the first year of life – from 0.9 units. up to 1.25 units
- Children from one to six years old can normally have 0.95-1.1 units.
- In patients aged 12-16 years, the normal INR ranges from one to 1.35 units.
- After 16 years, the value should be within 0.85 units. – 1.3 units.
For those who have already been prescribed anticoagulant therapy, the INR should be between 2.0 units. up to 3.0 units, because drugs that fight the formation of blood clots do not allow the blood to thicken, which also affects the prothrombin index.
If a patient is not taking blood thinning medications, but his INR is higher than normal, this may indicate:
- liver diseases;
- coagulopathies;
- prothrombin deficiency;
- lack of fibrogen;
- vitamin K deficiency;
- taking certain medications that affect blood composition;
A low INR always indicates that a person is at risk. Value below 0.5 units. reports the onset of venous thrombosis.
Who do doctors prescribe “indirect” anticoagulants (warfarin)?
Patients who need treatment and prevention of thrombosis and embolism of blood vessels, including: – heart rhythm disturbances (atrial fibrillation); – heart valve diseases;
– presence of prosthetic heart valves or blood vessels, incl. in combination with aspirin (acetylsalicylic acid); – acute venous thrombosis (phlebothrombosis) and pulmonary embolism (in combination with heparin); – recurrent venous thrombosis; – repeated pulmonary embolism; – thrombosis of peripheral, coronary and cerebral arteries; – postoperative thrombosis; – myocardial infarction, complicated by the development of an aneurysm and intracardiac thrombus; – during surgical or thrombolytic treatment of thrombosis; – when performing electrical cardioversion of atrial fibrillation (as an additional therapy); – congenital diseases accompanied by pathological thrombosis (thrombophilia).
Why do you need to know the INR?
INR analysis is a common research method during the diagnosis of cardiovascular diseases. In addition, bleeding and severe thrombus formation are direct indications for studying all parameters affecting coagulation.
Knowing the INR is very important for the cardiologist who prescribed anticoagulants to the patient, since this allows him to control the correctness of the dose calculation, in order not to harm the patient. This also includes taking warfarin, the dosage of which is determined for each patient individually.
In case of cirrhosis of the liver or other disease of the filtering organ, it is also important to know the INR level, because it is the liver that produces many factors that clot the blood.
A separate group of patients are pregnant women. First of all, this is due to the fact that the entire body system begins to work differently during pregnancy. The level of hormones and enzymes changes, and the volume of blood circulating through a woman’s veins increases. Hence the need to control the functioning of the hematopoietic system. Due to the high level of blood clot formation, the likelihood of complications is high. And if the blood is too thin and there is a lack of platelets, there is a high probability of dangerous bleeding during childbirth.
At the very beginning of labor, each woman in labor is given a catheter in a vein, into which, if necessary, an IV will be placed with a composition that increases the level of blood clotting to prevent large blood losses.
Complexes with this research
Examination during pregnancy.
1st trimester 17,040 ₽ Composition Female infertility Analysis of women's reproductive health 16,470 ₽ Composition
Examination during pregnancy. 3rd trimester 9,840 ₽ Composition
IN OTHER COMPLEXES
- Coagulogram RUB 2,080
- Men's check-up No. 1 RUB 18,920
- Women's check-up No. 1 RUB 19,720
- Pregnancy planning. Clinical indicators 6,800 ₽
- For those at risk of COVID-19 RUB 4,620
Do I need to prepare for an INR test?
First of all, you need to remember that blood to determine the INR value is taken from a vein. A prerequisite is on an empty stomach. This means that you cannot eat or drink sugary water 6-8 hours before. At the same time, you should not fast for more than 10 hours before donating blood, as this will distort the data.
The day before the test, you do not need to do heavy physical work. If the patient jogs in the morning every day, before going to the laboratory, you will have to abandon the activity and reschedule it for the evening. Since jogging will affect the speed of blood flow, blood oxygen saturation and its composition.
Any daily medication intake should also be taken into account - the evening dose on the eve of sampling should be taken no later than 17:00. And triple the appointment must be rescheduled, and you need to take the medicine/get an injection after donating blood.
It is recommended to approach the building of the medical institution 15 minutes before the appointed time in order to have time to put your outerwear in the cloakroom, take your time, find an office and calm down before the procedure. Even slight anxiety associated with the fear of being late can affect the composition of the blood.
We must not forget that taking oral contraceptives significantly distorts the actual state of the coagulation systems due to the elements included in the composition that prevent the formation of blood clots. Therefore, an INR test should be scheduled on the fourth day after completing a three-week course of birth control pills. In other words, the test can be taken closer to the end of the week during which withdrawal bleeding occurs. If this is difficult, you must tell the laboratory assistant the name of the drug you are taking so that he takes its effect into account when calculating the result.
Technique and frequency of blood sampling
A blood test to determine the INR is carried out for persons who are constantly taking indirect anticoagulants (Sincumar, warfarin), at intervals of two to three weeks. Sometimes there is a need to conduct research more often. It all depends on the duration of treatment, the patient’s condition and the specific type of pathology. Patients with an adjusted anticoagulant dose and appropriate INR can be monitored once a month.
It is possible to obtain blood for research only by collecting it from a peripheral vein. The sampling technique does not differ from standard tests. Compliance with the study rule on an empty stomach is mandatory.
Diet while taking warfarin. Vitamin K content
Warfarin is absorbed in the stomach and jejunum, so changes in the intestinal microflora that produce vitamin K may affect the effect of the drug. The activity of warfarin can also be affected by the food the patient eats. The diet when taking warfarin should take into account those foods that contain large amounts of vitamin K, which can weaken the effect of warfarin, and the lack of vitamin K in the diet can enhance the effect of the drug. Therefore, if you are prescribed warfarin, try to eat a balanced diet and try not to change your diet dramatically so as not to change the amount of vitamin K you get from food.
| Vitamin K content in foods (µg/100 g) | |
| Beef liver | 93 |
| Cheese | 35 |
| Butter | 30 |
| Egg | 11 |
| Soybean oil | 193 |
| Broccoli | 175 |
| Cabbage | 125 |
| Salad | 129 |
| Watercress | 200 |
| Head lettuce | 120 |
| Spinach | 415 |
| Cauliflower | 80 |
| Green tomatoes | 80 |
| Beans | 45 |
| Cucumbers, zucchini | 30 |
| Potato | 16 |
| Green tea | 712 |
| Note: daily requirement of vitamin K is 0.03-1.5 mcg/kg/day (up to 105 mcg/day) | |
Warfarin and alcohol
Alcohol is not recommended during warfarin treatment.
You can indulge in a glass of wine once or twice a week. Exceeding this norm may lead to increased effects of the drug and, as a result, possible bleeding. Illnesses that affect appetite and digestion (vomiting, diarrhea) can also reduce or increase the effect of warfarin, so tell your doctor about any changes in how you feel.
Be sure to tell us about all the medications you are taking or have taken shortly before starting warfarin treatment, as well as new prescriptions if you are already taking warfarin therapy. Many drugs can increase or decrease the effect of warfarin on blood clotting. Keep all prescriptions and write down the names of medications you take. The table shows the most commonly prescribed drugs that can affect the effectiveness of warfarin.
How to take medications correctly
In what situations is this examination prescribed?
This examination is prescribed during treatment with indirect anticoagulants - vitamin K antagonists (neodicoumarin, warfarin, syncumar), which reduce the level of prothrombin in the blood, thus thinning it.
Regular monitoring of the indicator allows you to control the dosages of the above drugs to avoid bleeding or blood clots.
When is it necessary to take indirect anticoagulants?
In what situations is it necessary to regularly take a blood test for INR and prothrombin?
- Treatment and prevention of thrombosis of the superficial and deep veins of the lower extremities;
- Varicose veins;
- Acute coronary syndrome;
- Cerebrovascular accident in the acute stage (ACVA);
- PE (pulmonary embolism);
- Permanent form of atrial fibrillation;
- Heart disease;
- Thrombophlebitis;
- The presence of artificial valves in the heart;
- The presence of a vena cava filter (a filter in a large vein of the body that prevents thrombotic masses from entering the veins of the lower extremities and pelvic organs to the heart and lungs.
It must be remembered that when using warfarin and other anticoagulants, the INR level is increased and should be kept within 2.0 - 3.0 (the optimal value is 2.5), and with prosthetic heart valves from 2.5 to 3.5. Patients with an INR value above 6.0 require urgent treatment.
If a person is not treated with anticoagulants, then a deviation of the INR from the norm can cause serious pathological changes in the body. Let's consider in what situations the level of this indicator may change.
What are the indications for an emergency test?
- Acute infectious disease (respiratory, intestinal infection).
- Climate change (long-distance and long flights, transfers).
- Changing work and rest schedules, diet, physical activity, taking new medications. It should be noted that when taking new medications or consuming new foods, the INR should not be rechecked immediately, but after 2-3 days. It must be remembered that there is a list of drugs that increase or decrease the effect of warfarin.
- Frequent and prolonged bleeding (nose, gum, menstrual, blood in stool, urine, sputum).
- The appearance of compactions and swelling in the joints.
- Before planned invasive procedures (tooth extraction, gastroscopy)
In conclusion, I would like to say that following simple rules for taking anticoagulants with regular monitoring of INR will save you from unnecessary costs for expensive and inappropriate treatment and severe complications.
How is it carried out?
Biological material is collected using a sterile dry syringe or a vacuum blood collection system. The puncture of the vein must be non-traumatic, otherwise there will be a lot of thromboplastin in the test tube, which will lead to distortion of the final results of the study.
The specialist fills two test tubes with blood, but only sends the second one for analysis. A coagulant (sodium citrate) is applied to its walls. In the laboratory, a series of reactions are carried out with blood, which takes some time. The analysis usually takes 1-2 business days. However, much also depends on the availability of reagents and the workload of the laboratory.