General information about cardiac ischemia
Coronary heart disease develops when the heart vessels are unable to provide it with a sufficient amount of blood with oxygen and nutrients. This happens when their lumen is narrowed by an atherosclerotic plaque.
Clinical forms of coronary heart disease:
- Angina
- attacks of chest pain lasting a maximum of 20 minutes, which disappears at rest or after taking nitroglycerin. - Myocardial infarction
: acute myocardial infarction, recurrent (occurring less than 8 weeks after acute), repeated (occurring more than 8 weeks after acute) - Post-infarction cardiosclerosis
ー replacement of dead areas of the myocardium with connective tissue (“scar”). - Heart failure
is the inability of the heart to “pump” blood to ensure sufficient blood supply to all organs. - Sudden cardiac death (fibrillation)
.
Symptoms of Cardiovascular Diseases
Diseases of the heart and blood vessels in the initial stages are often asymptomatic and can manifest acutely - manifestations of a heart attack or stroke. The debut (or exacerbation of chronic pathology) is often preceded by nervous shock, overwork, physical exertion, and overeating. Most heart pathologies are accompanied by heart failure.
Symptoms of heart disease:
- Acute heart failure - cold sweat, sudden loss of strength, severe suffocation, cough with foam (a sign of pulmonary edema), cyanosis of the skin (cyanosis)
- Chronic heart failure - fatigue, poor exercise tolerance, shortness of breath, suffocation, dry cough (sometimes hemoptysis), scanty urination, edema, ascites.
- Myocardial infarction - acute chest pain radiating to the left shoulder, upper back, neck, chin (sometimes intense abdominal pain); shortness of breath, severe weakness, cold sweat; feeling of anxiety, fear of death.
- Rheumatic carditis – increased sweating, fever, signs of heart failure.
- Cardiac arrhythmia - palpitations, a feeling of “fading” of the heart, dizziness, fainting, manifestations of heart failure.
Signs of vascular pathologies:
- Arterial hypertension - heaviness, pain, pulsation in the back of the head; lethargy, dizziness, tinnitus, nausea; sensation of “floaters” before the eyes.
- Stroke - can begin gradually, with a weakening of muscle tone, numbness of certain areas of the face and limbs. Then lethargy and loss of sensitivity intensify to paresis, and the affected areas expand. Impairments in hearing, vision, speech, and coordination of movements may develop. General cerebral symptoms – nausea, vomiting, confusion, coma.
- Chronic cerebrovascular accident - attacks (transient ischemic attacks) are accompanied by more pronounced signs of arterial hypertension, transient disturbances in speech, hearing, vision, memory, unsteadiness of gait, and fainting. Symptoms disappear within 24 hours.
- Pathologies of peripheral arteries accompanied by ischemia (thromboembolism, thromboangiitis obliterans and atherosclerosis) - acute, unbearable pain, transient lameness, dry skin, change in its shade (at first pale, as it progresses - purple), the appearance of poorly healing ulcers.
- Deep vein thrombosis - a feeling of bursting pain in the affected limb, swelling, cyanosis of the skin, visible vascular network.
- PE – may combine signs of heart failure and stroke. Other symptoms are fever, pain in the right hypochondrium, skin rashes.
Acute CVD requires emergency medical care and intensive care. If you suspect these pathologies, you should immediately call an ambulance.
Risk factors for coronary heart disease
The main cause of atherosclerosis is a violation of lipid metabolism, an excess of saturated (animal) fats and a lack of unsaturated (vegetable, fish). Excess cholesterol in the blood is deposited in the wall of the vessel; over time, a dense formation is formed, which significantly reduces the lumen of the artery; blood cannot fully flow to the heart muscle.
Another possible reason for the narrowing of the lumen of the coronary vessels is spasm. The main provocateurs of arteriolar spasm are nicotine and alcohol. Therefore, it is important to give up bad habits for heart health.
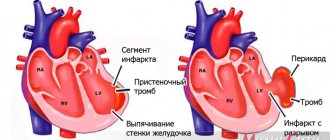
The last cause of coronary artery disease is coronary thrombosis.
Risk factors for developing coronary artery disease:
- age over 55 years;
- male gender;
- obesity;
- smoking;
- alcohol abuse;
- high cholesterol in the blood;
- diabetes mellitus type 2;
- sedentary lifestyle.
Why does pathology occur?
The main cause of the disease is damage to the coronary arteries by atherosclerosis, in which cholesterol plaques appear in the vessels. After some time, a blood clot may form at the site of the plaque, which partially or completely blocks the artery, blocking the supply of oxygen to the heart muscle.
As a rule, narrowing of the lumen of the vessel up to 50% occurs without any clinical manifestations. Vivid symptoms appear when the artery is blocked by 70% or more.
Very rarely (up to 5% of cases) IHD is caused by:
- congenital anomalies of the origin of the coronary arteries;
- Marfan, Ehlers-Danlos syndromes - hereditary pathologies of connective tissue;
- infective endocarditis - inflammation of the inner lining of the heart caused by pathogenic pathogens;
- Kawasaki syndrome is a systemic vasculitis affecting medium and small arteries;
- syphilitic aortitis is a complication of syphilis, in which inflammation of individual layers or the entire thickness of the aortic wall occurs;
- overdose of vasoconstrictors, narcotic drugs.
Symptoms of coronary heart disease
The main symptom of IHD
ー pain behind the sternum or in the heart area of a burning or pressing nature. There is irradiation of pain to the left arm, shoulder blade, neck, and face. Sometimes pain due to coronary heart disease is masked as a pathology of the abdominal organs: pain in the supra-umbilical region can be mistaken for manifestations of gastritis, pancreatitis or even appendicitis.
Pain in the heart area is a good reason to consult a therapist or cardiologist for a more detailed examination.
How to distinguish heart pain from neuralgia
Heart pain is often confused with neuralgic pain. Among the main characteristic symptoms of neuralgia are the following:
- the ability to determine a clear localization;
- unpleasant sensations are concentrated at one point;
- the nature of the pain is shooting, aching or stabbing;
- lasts for several days;
- the intensity of sensations does not depend on the time of day;
- worsens with twisting, sneezing or coughing, walking, palpation of intercostal areas;
- nitroglycerin is ineffective;
- the ability to breathe only superficially;
- often occurs after hypothermia;
- accompanied by impaired sensitivity of the skin;
- in the affected area, motor activity is significantly reduced.
Diagnosis of coronary heart disease
The diagnosis is established based on the patient’s complaints and symptoms, risk factors, as well as additional examination methods:
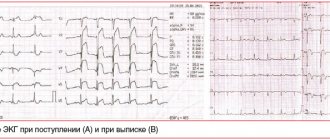
- ECG at rest and with physical activity;
- cardiac echocardiography (Echo-CG);
- clinical and biochemical blood tests;
- angiocardiography is an x-ray examination with the introduction of a contrast agent into the vessels of the heart.
These methods make it possible to assess the degree of patency of the coronary vessels and the presence of functional changes in the heart muscle.
Complications of CVD
According to WHO, cardiovascular pathologies are the main cause of death and often lead to disability. Death is not uncommon with large heart attacks and strokes, massive pulmonary embolism, heart failure complicated by pulmonary edema, and cardiogenic shock. A stroke can lead to a wide range of neurological disorders, and chronic cerebrovascular accident can lead to progressive cognitive impairment. Peripheral arterial pathologies are dangerous due to the development of gangrene with subsequent amputation of the limb (often at a young age). CVDs have a detrimental effect on the state of the reproductive sphere: impotence is often registered in men, and infertility and childlessness in women.
Forecast and prevention of coronary heart disease
Coronary heart disease is much easier to prevent than to cure. If the atherosclerotic process has already begun, it cannot be reversed, only slow down its development. Basic preventive measures:
- quitting smoking and alcohol abuse;
- healthy diet (reducing the level of animal fats, preferring vegetable fats, sufficient amounts of vitamins, fiber, protein);
- regular physical exercise in accordance with your health status;
- preventive blood tests every 1-2 years;
- timely visit to the doctor if alarming symptoms appear.
Prevention
Preventing a disease is much easier than curing it. To maintain healthy arteries and blood vessels, it is necessary to eliminate risk factors that negatively affect your health:
- To give up smoking;
- Monitoring blood pressure levels
- Normalization of the level of “bad” cholesterol (low-density lipoproteins)
- Fighting stress and depression
- Minimize alcohol consumption;
- Refusal of smoked, fatty, fried and salty foods.
Spend more time on an active lifestyle: moderate physical activity, therapeutic exercises, morning exercises, walking, swimming, dancing. Physical activity will help strengthen the walls of blood vessels and maintain normal weight, and if necessary, reduce it.
The most important thing in prevention is timely observation by a specialist. In order not to visit medical institutions several times to undergo all the necessary tests and examinations, contact our cardiology center. Federal Research Center FMBA offers patients several programs for comprehensive heart research. You can find them here.
Diagnosis and treatment of coronary heart disease in Medical
When should you see a doctor?
The reason for a visit to the doctor should be the appearance of pain and discomfort in the heart area, which appears during physical activity or at rest. These symptoms cannot be ignored, because IHD does not go away on its own, it only progresses over the years.
Over time, heart failure develops and there is a risk of myocardial infarction and sudden cardiac arrest. Don’t deprive yourself of the possibilities of modern medicine - make an appointment with a cardiologist or general practitioner at a medical clinic.
Drug treatment of ischemia
IHD cannot be cured with medications, but it can be controlled. Patients are prescribed drugs that increase blood flow to the myocardium and reduce its oxygen demand: antithrombotics, B-adrenergic receptor blockers, ACE inhibitors. To eliminate pain during an attack, it is recommended to take nitrates, for example, nitroglycerin.
Silent myocardial ischemia
Silent ischemia is based on a discrepancy between the myocardial oxygen demand and the actual perfusion of the heart muscle. Under the influence of certain reasons (emotional stress, physical activity, etc.), cardiomyocytes begin to feel oxygen starvation and compensatoryly switch to an oxygen-free type of energy synthesis - anaerobic glycolysis. This type of glucose metabolism leads to rapid energy depletion of cells and the accumulation of compounds that normally irritate nerve endings that are involved in the formation of the sensation of pain in the cerebral cortex. With BBIM this sensation does not occur. There are several pathogenetic hypotheses, but none of them fully explains the mechanism of development of painless attacks.
The painlessness of ischemic episodes is associated with reduced sensitivity of intracardial nerve endings due to diabetic neuropathy, partial death of neurons during infarction, and the effects of drugs and toxins. The paradox is that painless ischemia also occurs in relatively healthy individuals who do not have a history of factors that can reliably disrupt the conduction of nerve fibers of the heart (without a heart attack, other cardiovascular events, diabetes, chronic or acute intoxication).
The absence of pain is also associated with insufficient strength and duration of myocardial ischemia. It has been experimentally proven that ischemia causes pain only when certain threshold values are reached - for a duration of at least 3 minutes. However, cases of anginal pain with minimal manifestations of ischemia and, conversely, the absence of any symptoms with extensive long-term disturbances in cardiac muscle perfusion are also known.
“Silent” ischemia is also explained by a failure in the formation of pain sensations due to a decrease in the number of intramuscular receptors for adenosine (the main activator of pain receptors released during cardiac ischemia) or a decrease in the sensitivity of these same receptors to it. However, it is impossible to reliably establish exactly how the number of receptors changes from the onset of the disease to the moment the patient seeks help. It is also unclear why, with the same concentration of adenosine, in some cases the ischemia is “silent”, while in others it is accompanied by pain.
The absence of pain is also associated with an increase in the activity of the anti-pain system, which has a neurohumoral regulation mechanism. Reduction of pain due to activation of the nervous component is realized by increased activity of the reticular formation and thalamus in the brain. The humoral component is manifested by an increase in the plasma concentration of natural opioids - endorphins, which reduce susceptibility to pain. It has been established that patients with BBIM have a higher level of endorphins in the blood plasma both after exercise and at rest than patients with clinical manifestations of ischemia.
Treatment
Depending on the type of pathology, treatment is carried out under the guidance of a cardiologist, neurologist, vascular surgeon, neurosurgeon, cardiac surgeon, phlebologist, rheumatologist. Emergency conditions require the help of a resuscitator. There are conservative and surgical methods for treating CVD.
Conservative methods include:
- drug therapy – medications are prescribed depending on the diagnosis;
- plasmapheresis, autohemotransfusion - in the treatment of rheumatic carditis;
- thrombolysis – dissolution of a blood clot during arterial embolism;
- physiotherapy – in the treatment of chronic cerebrovascular accidents, thromboangiitis obliterans.
Surgical methods for treating CVD:
- thromboembolectomy – surgical removal of a blood clot in case of ineffectiveness or contraindications to thrombolysis;
- thrombectomy – for deep vein thrombosis;
- stenting of peripheral vessels and coronary arteries – for atherosclerosis,
- heart valve replacement – for endocarditis;
- stereotactic aspiration of hematoma – for hemorrhagic stroke.
Today, open surgical interventions are rarely performed; preference is given to vascular surgery - this contributes to the speedy recovery of the patient and minimization of postoperative complications. However, after treatment of severe CVD, patients most often require long-term rehabilitation.