Cardiac aneurysm (aneurysma cordis) is a limited protrusion of a thinned area of the heart wall. Most often develops as a result of myocardial infarction. Congenital, infectious, traumatic, and postoperative cardiac aneurysms are much less common. Traumatic aneurysms occur due to closed or open heart injuries. This group also includes aneurysms that occur after operations for congenital heart defects.
In the overwhelming majority of cases, cardiac aneurysm is a complication after a myocardial infarction (usually transmural). Up to 25% of heart attack patients may be affected by this disease.
Dangerous complications of chronic cardiac aneurysm are gangrene of the limb, stroke, kidney infarction, pulmonary embolism, and repeated myocardial infarction. When a cardiac aneurysm ruptures, death occurs instantly.
Based on the time of occurrence, aneurysms are divided into acute (1-2 weeks from the onset of myocardial infarction), subacute (3-6 weeks) and chronic. Most often, post-infarction aneurysms are localized on the anterolateral wall and at the apex of the left ventricle; in 50-65% of cases they spread to the anteroseptal region.
Left ventricular aneurysm is diagnosed so often because of the maximum blood pressure in this ventricle. Up to 50% of the surface of the left ventricle may be damaged as a result of the pathological process.
1 Left ventricular aneurysm
Aneurysm of the posterior wall of the left ventricle is observed in 2-8% of patients. Blood clots are often found in the aneurysm cavity, but the incidence of thromboembolic complications is no more than 13%.
What is a cerebral aneurysm
An aneurysm, most commonly a saccular aneurysm, is a spherical or similar formation on an artery in the brain. An aneurysm, as I have already noted, can be saccular and fusiform. An aneurysm consists of three parts - the neck, body and bottom or apex. Unlike a normal vascular wall, the apex of the aneurysm is not three-layered, but single-layered and is most vulnerable to rupture, especially since a shock flow of blood rushes into this place. Most often, the aneurysm is located in the anterior sections of the circle of Willis - in descending order - an aneurysm of the anterior communicating artery of the PSA, then an aneurysm of the internal carotid artery of the ICA, and an aneurysm of the middle cerebral artery. Less common are aneurysms of the vertebrobasilar region - aneurysms of the fork of the main artery of the OA, the mouth of the posterior inferior cerebellar artery of the PICA. Aneurysms of the pericallosal artery and other distal parts of the anterior cerebral and middle cerebral arteries are also quite rare.
Symptoms and signs of abdominal aortic aneurysm
In most patients, abdominal aortic aneurysms occur without any symptoms and are an incidental finding during examinations and operations for other reasons.
When signs of an aneurysm develop, the patient experiences one or more of the following symptoms:
- A feeling of pulsation in the abdomen, similar to a heartbeat, an unpleasant feeling of heaviness or fullness.
- Dull, aching pain in the abdomen, in the navel area, usually on the left.
Indirect signs of abdominal aortic aneurysm are important :
- Abdominal syndrome. Manifested by the appearance of belching, vomiting, unstable stool or constipation, lack of appetite and weight loss;
- Ischioradic syndrome. Manifested by lower back pain, sensory disturbances and movement disorders in the lower extremities;
- Syndrome of chronic ischemia of the lower extremities. Manifests itself in the appearance of pain in the muscles of the lower extremities when walking, sometimes at rest, coldness of the skin of the lower extremities;
- Urological syndrome. It manifests itself as pain and heaviness in the lower back, difficulty urinating, and the appearance of blood in the urine.
Harbingers of rupture may be increased abdominal pain.
When an aneurysm ruptures, the patient suddenly feels an increase or appearance of abdominal pain, sometimes “radiating” to the lower back, groin area and perineum, as well as severe weakness and dizziness. These are symptoms of massive internal bleeding. The development of such a situation is life-threatening! The patient needs emergency medical care!
Cerebral aneurysm photo
I present to your attention a photo of 2 aneurysms - the main artery and the bifurcation of the middle cerebral artery, which we encountered in our clinic over the past 2 weeks.
Saccular aneurysm of the bifurcation of the basilar artery
Saccular aneurysm of the bifurcation of the left middle cerebral artery. The aneurysm and branches of M2 are outlined with a ballpoint pen.
The aneurysm of the bifurcation of the basilar artery had to be transferred to another health facility for endovascular exclusion (filling with coils), and the MCA aneurysm was operated on in our clinic.
Clinical picture
Symptoms are nonspecific. The classic triad is represented by:
- Shortness of breath;
- Pain syndrome;
- Feeling of irregularities and rapid heartbeat.
Shortness of breath is of a mixed nature and is manifested by difficulty in both inhalation and exhalation. The pain syndrome develops like angina pectoris - within 10-15 minutes after physical activity. The feeling of interruptions is due to developing arrhythmia and can be paroxysmal or permanent.
Other manifestations:
- Fainting;
- Edema;
- Decreased exercise tolerance;
- Insomnia;
- Sudden cardiac death.
Cerebral aneurysm causes of occurrence
The final genesis of the arterial aneurysm is not clear. Some argue that this is a congenital phenomenon - an undeveloped, blindly ending short vessel. Others say that this is an acquired condition - a protrusion in a weak spot of the hemangion - the structural unit of the vessel, between the circular areas of smooth muscle. As a result of the impact of the shock wave, this protrusion gradually grows. The formation of de-novo aneurysms confirms the presence of new aneurysms during control angiography in already operated patients. There is also an autoimmune inflammatory theory of the occurrence of arterial aneurysms, which is being actively developed at the University of Helsinki with the participation of Professor J. Hernisniemi. Thus, he believes that eventually a drug will be developed that can treat and prevent aneurysmal disease (he considers himself the last of the Mohicans - i.e. "aneurysmal" surgeons).
Definition:
A cardiac aneurysm is a pathological condition that is accompanied by protrusion of the wall of the heart muscle. It is one of the complications after a myocardial infarction and can develop within several months after its onset. An aneurysm not only negatively affects the functioning of the heart and its contractile functions, but also poses a serious danger to life due to the possibility of sudden rupture.
Cerebral aneurysm - symptoms
Most often, an aneurysm debuts with rupture - the most serious, often fatal complication. Hemorrhage can be subarachnoid, parenchymal and ventricular , and there are also all kinds of combinations of this trinity.
Among the atypical manifestations is pseudotumor ; with a gigantic size of the aneurysm, it can behave like a tumor and compress the brain and nerves, causing focal neurological symptoms.
A migraine-like course is manifested by hemicranialgia.
Pseudoradicular simulates radiculitis - pain in the legs, which is caused by blood flowing into the terminal cistern of the spinal cord.
Meningitis-like - in this case, patients with suspected bacterial meningitis can be admitted to an infectious diseases hospital, where SAH and suspected aneurysm rupture are diagnosed only with a lumbar puncture.
Psychotic - the name speaks for itself.
Complications
Common complications associated with AVA include:
- heart disease;
- narrowing of the pulmonary artery resulting in difficulty breathing;
- infectious diseases;
- decreased immune system functions;
- atherosclerosis;
- incorrect functioning of blood vessels.
When an aneurysm is diagnosed in the later stages of development, it may cause the following complications:
- pulmonary edema;
- thrombosis;
- strokes;
- vascular rupture and hemorrhage.
The listed complications pose a threat to the patient’s life and can lead to lifelong disability.
Treatment methods for cerebral aneurysm
Surgical
Aneurysm can only be treated surgically - by direct intervention, disconnection by clipping, wrapping with various materials (rarely) or by the endovascular method. Only milliary aneurysms can be observed in patients without risk factors for rupture. Aneurysms without previous hemorrhages are also subject to surgical treatment. It is easier to prevent a rupture than to treat its fatal consequences - vasospasm and clipping the aneurysm in the acute period.
Intraoperative photo of a clipped left middle cerebral artery aneurysm.
CT angiography the next day after surgery. Aneurysm is turned off. The M2 segments of the left MCA are contrasted.
The red circle marks the intervention area where 2 clips are installed. There are signs of vasospasm.
In the area of surgery on a native CT scan of the brain along the Sylvian fissure there is a small amount of blood - impregnated surgicell.
On a CT scan in bone mode, the clip is clearly visible.
Publications in the media
A cardiac aneurysm is an area of thinned myocardial tissue with protrusion of the ventricular wall in this area. This section covers only post-infarction cardiac aneurysms due to their significant epidemiological significance.
Statistical data • Post-infarction aneurysm complicates 10–35% of transmural MI • According to pathological studies, the incidence of post-infarction aneurysm is 8.5–34% • In men, cardiac aneurysms form 5–7 times more often than in women • Under the age of 40 years, post-infarction aneurysm occurs in 13% of people, and among people over 60 years of age - in 5.5%, which is due to the higher frequency of extensive transmural MI at a relatively young age • The frequency of formation of post-infarction aneurysms has a clear dependence on the strategy of early revascularization in individual clinics • Congenital Cardiac aneurysms formed from diverticula of the right ventricle and left ventricle (LV) are isolated cases; post-traumatic aneurysms are also rare.
Etiology • Acute post-infarction aneurysm (formed during acute transmural MI) is represented by necrotic tissue, chronic (forms at least 6-8 weeks, if there is no relapse of MI) - cicatricial • The formation of aneurysms is facilitated by arterial hypertension, the use of GCs, non-compliance by the patient with the regimen in acute period of MI.
Classification. The following types of post-infarction aneurysms are distinguished: • True aneurysms: •• diffuse; •• sac-like (with a narrow base); •• dissecting • False aneurysms - formed when the myocardial wall ruptures and limited to pericardial adhesions • Functional aneurysms - zones of viable (so-called hibernating) myocardium that has lost contractility and bulges during ventricular systole.
Pathogenesis • Contractile dysfunction in the area of the aneurysm is represented by akinesia (lack of contractile activity) and dyskinesia (bulging of the ventricular wall in systole and its retraction in diastole) • Hemodynamic disturbances are caused by the following mechanisms •• Decreased systolic function (when switched off from contraction more than 20–22 % LV area) •• Impaired diastolic function (impaired pressure-volume relationship leads to a disproportionate increase in end-diastolic pressure [EDP]) •• Mitral regurgitation (due to dilatation of the annulus fibrosus or damage to the papillary muscles) •• Thrombosis of the ventricular cavity ( observed in 40% of cases) • Compensatory mechanisms in the form of myocardial hypertrophy, changes in the configuration of the LV cavity and its dilatation (remodeling) lead to the progression of heart failure • Thromboembolism develops in 2–5% of patients, and in most patients, certain ventricular arrhythmias.
Clinical manifestations • Complaints •• Signs of heart failure - shortness of breath, episodes of pulmonary edema (20%) •• Rhythm disturbances - syncope episodes and a feeling of interruptions in the heart (35%) •• Thromboembolism, usually occurring in the femoropopliteal or iliac segments, less often - in the brachiocephalic trunk, and ischemia of the viable myocardium, for example angina pectoris (60%) • Objective examination data •• Signs of circulatory failure - tachypnea, moist rales in the basal parts of the lungs, later - edema, ascites, hepatomegaly •• Symptoms of mitral regurgitation - see Mitral valve insufficiency •• Signs of previous embolisms are focal neurological defects, absence of pulsation in the arteries of the lower extremities.
Instrumental diagnostics
• ECG •• There are no pathognomonic signs •• Signs of previous MI •• There is no dynamics of ST segment displacement, characteristic of an uncomplicated course of MI (“frozen” MI) •• In 85% of cases, post-infarction changes are localized in the anterolateral region.
• EchoCG •• Visualization of the aneurysm cavity, measurement of its size, assessment of the configuration of the aneurysm and diagnosis of thrombosis of the LV cavity •• Calculation of the index of local contractility disorders •• Stress test to identify viable myocardium in the area of the aneurysm •• Differentiation of true and false aneurysms (highly specific method) •• Identification and functional assessment of mitral regurgitation (see Mitral valve insufficiency).
• X-ray of the chest organs •• Cardiomegaly due to bulging of the LV arch or local bulging along the left contour of the heart shadow •• When performing kymography - paradoxical pulsation in the area of the aneurysm •• Symptoms of congestion in the pulmonary circulation (increased pulmonary pattern, expansion and lack of structure of the roots of the lungs , Kerley lines type B).
• Radioisotope ventriculography •• Determination of the location and size of the aneurysm, thrombosis of its cavity •• Calculation of volumetric indicators of the LV and assessment of its contractile function at rest and during pharmacological testing.
• MRI allows you to obtain the same information as radiopaque ventriculography •• Performed when radiopaque ventriculography is contraindicated •• A highly specific method for detecting LV thrombosis •• Three-dimensional reconstruction of the LV cavity is possible (important information for determining surgical tactics).
• Perfusion scintigraphy or single photon emission CT of the myocardium: detection of perfusion defects in the aneurysm and other areas at rest and during pharmacological testing.
• Positron emission tomography of the myocardium: identification of viable myocardium in the area of the aneurysm and other areas.
• X-ray contrast left ventriculography •• Determination of the location and size of the aneurysm, thrombosis of its cavity •• Calculation of volumetric indicators of the LV and assessment of its contractile function •• Calculation of the area of the aneurysm (using the central angle method or graphic integration) and the contractile part of the LV.
• Catheterization of the left atrium and LV: increased EDP, systolic blood pressure, diastolic blood pressure.
• Coronary angiography •• Performed in all candidates for surgical treatment and in patients in whom noninvasive testing reveals ischemic viable myocardium.
• Electrophysiological study is performed in patients with ventricular arrhythmias in the presence of clinical manifestations.
TREATMENT
Drug therapy - see Ischemic heart disease, Chronic systolic cardiac failure, Mitral valve insufficiency.
Surgery
• Indications •• Large size of the aneurysm (more than 22% of the LV wall area) in the presence of the following clinical indications: ••• anginal pain ••• clinically significant heart failure ••• ventricular arrhythmias ••• LV wall rupture ••• pseudoaneurysm • •• congenital aneurysm ••• thromboembolism ••• asymptomatic aneurysms with a progressive increase in their size •• Severe mitral regurgitation.
• Relative contraindications •• Asymptomatic aneurysms of stable size, even if these patients are scheduled for coronary bypass surgery •• High anesthetic risk •• Inability to restore myocardial function outside the aneurysm area, cardiac index <2.0 l/min/m2 •• Confirmed non-transmural perfusion defect ( the presence of hibernating myocardium in the area of the aneurysm) •• Progressive mitral regurgitation.
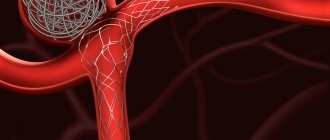
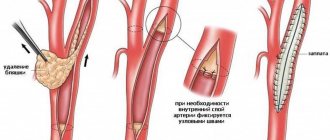
• Methods of surgical treatment •• Palliative interventions - support-ring mitral anuloplasty according to Carpentier •• Radical interventions ••• Resection of aneurysm ••• In the presence of an aneurysm of the interventricular septum - septoplasty according to Cooley ••• For large aneurysms - resection followed by reconstruction of the LV with a patch according to Jatin-Dor ••• In case of rupture of the free wall of the LV, post-traumatic and false aneurysms - suturing of the rupture of the LV wall ••• If it is necessary to perform revascularization interventions, preference is given to coronary bypass surgery, performed in one stage with surgery for the aneurysm.
Specific postoperative complications • Small output syndrome - 22-39% • Rhythm disturbances - 9-19% • Respiratory failure - 4-11% • Bleeding - 4-7% • Acute vascular insufficiency with the need for dialysis - 4% • Acute cerebrovascular accident - 3–4%.
Prognosis • In the absence of clinical symptoms, the prognosis is favorable: more than 2/3 of patients do not develop symptoms within 10 years • 10-year survival rate in the absence of clinical manifestations is 90%, in patients with symptoms of the disease - 46% • Despite the fact that Early studies demonstrated low survival rates in patients receiving drug treatment (12% at 5 years), the use of angiotensin-converting enzyme (ACE) inhibitors, control of thrombus formation and arrhythmias, according to recent studies, increases 5-year survival to 47– 70% • Among the causes of death, 44% are rhythm disturbances, 33% are heart failure, 11% are recurrent MI, 22% are noncardiac causes • Factors influencing the prognosis in patients receiving drug therapy - age, cardiac class insufficiency according to NYHA (USA), the presence of anginal episodes, mitral regurgitation, ventricular arrhythmias, aneurysm volume, ejection fraction • In patients with thrombosis of the LV cavity identified by echocardiography, the risk of thromboembolism is 19% within 24 months • The risk of thromboembolism against the background of a short course of anticoagulant therapy is 0.35% per year; Long-term treatment with anticoagulants in these patients does not improve the prognosis • Factors influencing the risk of thromboembolism are aneurysm volume and atrial fibrillation • With surgical treatment, in-hospital mortality is 2-19% (average 9.9%), in more recent reports - 3- 7% • Factors that increase in-hospital mortality are age, incomplete revascularization, high class of heart failure, female gender, urgency of intervention, left ventricular ejection fraction less than 20–30%, the need for simultaneous mitral valve replacement, refusal to use the internal mammary artery • Distant results vary among patient populations •• 5-year survival - 58-80% •• 10-year overall survival - 34% •• 10-year cardiovascular event-specific survival - 57% • Cause of most cardiovascular events deaths becomes recurrent MI • Preoperative factors that increase long-term mortality are age, class of heart failure, ejection fraction less than 35%, cardiomegaly according to radiography, CDP >20 mm Hg, mitral regurgitation.
Abbreviations • LV - left ventricle • EDP - end diastolic pressure.
ICD-10 • I25.2 Past MI • I25.3 Cardiac aneurysm
Cerebral aneurysm - consequences after surgery
The consequences of the operation, as well as the natural course of the disease, very often is cerebral vasospasm, which leads to unsatisfactory treatment results - death or severe neurological deficit in the form of paresis and paralysis, aphasia, mental disorders (which is typical for aneurysms of the anterior communicating artery). Meningitis may be a complication of the operation itself, which is associated with the presence of blood - a rich nutrient medium in the subarachnoid space, in the basal cisterns, cerebral ischemia, and a rather long operation time.
Thus, the treatment of arterial aneurysms is a very urgent and difficult problem in neurosurgery, especially in the acute and acute periods of hemorrhage.
Author of the article: neurosurgeon Anton Viktorovich Vorobiev Frame around the text
Why choose us:
- we will offer the most optimal treatment method;
- we have extensive experience in treating major neurosurgical diseases;
- We have polite and attentive staff;
- Get qualified advice on your problem.
Diagnostics
Computed tomography and x-rays are the main methods to detect abnormalities. In the first case, medical workers discover that bleeding has begun in the lungs.
X-ray allows you to diagnose where exactly the structural disorder of the pulmonary artery wall is localized, what its size is, and how best to eliminate the threat to the patient’s life.
Despite the complexity of diagnostic measures, it is better to identify an aneurysm in the early stages, which will help to exclude death. During the initial examination, the pulmonologist interviews the patient, establishes the cause of the pathology, and draws conclusions about the appropriateness of certain types of exposure.
Classification
Depending on the time period after myocardial infarction the aneurysm formed, the following forms are distinguished:
- Acute and subacute - develop in the early stages after a heart attack, often complicated by incomplete rupture.
- Chronic - formed after acute due to the replacement of a dead section of the heart muscle with connective tissue. They can be muscular, musculofibrous or fibrous.