Many people, in normal condition or with various diseases, experience a symptom such as cardiac arrhythmia. This is a kind of heart rhythm disorder, which is expressed in changes in the frequency of contractions, disturbances in the conductivity of the electrical impulse, as well as irregular rhythm reproduction.
One of the types of arrhythmia of a physiological nature is respiratory arrhythmia of the heart, better known as sinus arrhythmia. Its main difference is that there is a certain connection between the functioning of the respiratory organs and the cardiovascular system. In fact, this disease is typical for adolescent children.
In most cases, patients do not complain of any ailments, but with deep breathing this type of arrhythmia becomes more noticeable. This is due to the fact that at the moment of inhalation, contractions of the heart muscle become more frequent, and when exhaling, the opposite is true.
In young men, this can occur throughout the entire respiratory process, but in adults, especially older people, it occurs only when taking a deep breath.
Causes of pathology
- Alcohol abuse, smoking, drug use
- Including plenty of caffeine-containing foods and drinks in your diet
- Side effects of certain medications
- Psycho-emotional stress and hard physical labor
- Somatic diseases (coronary heart disease, consequences of myocardial infarction, arterial hypertension, diseases of the adrenal glands and thyroid gland)
- Traumatic brain injuries
- Menopause
Clinical symptoms
Clinically, various rhythm disturbances may not manifest themselves in any way, that is, the patient himself does not complain, or predictors of arrhythmia are identified during a preventive or any other examination (during ECG registration, examination by a therapist). With a clinically pronounced course, a number of symptoms can be identified:
- tachycardia (increased heart rate)
- bradycardia (slow heart rate)
- feeling of heart failure
- sensation of a foreign body, heaviness in the chest
- change in the frequency and depth of breathing movements
- general weakness
- loss of consciousness (in extremely severe clinical cases)
Stages and signs
Sinus arrhythmia can also be classified based on the severity of the process.
Accordingly, three stages are distinguished:
- Soft or weak. Changes are minimal or completely absent, although organic damage to the heart already exists. Careful diagnostics are required to identify the problem. It exists in three named forms: tachycardia (over 110 beats per minute), bradycardia (less than 70 beats per minute), classic violation of the interval between contractions.
- Moderate sinus arrhythmia. Accompanied by pronounced deviations in the functional activity of the heart. The clinical picture is noticeable without diagnosis, but everything disappears quickly. Therefore, the patient does not have time to react. Increased rhythm - more than 120 beats. per minute Weakening - less than 60. Complications are not common, but are possible. You need to monitor your own condition.
- Severe sinus arrhythmia is the most dangerous type and can lead to cardiac arrest, heart attack, and complications. Heart rate is more than 140 or below 50.
Regardless of the type of pathological process, its stage, the symptoms are always the same, only the strength of expression differs. Some manifestations appear at later stages.
A sample list of symptoms is:
- Dyspnea. The patient lacks air, although there are no objective changes in the lungs and bronchi. The result of tissue hypoxia.
- Feeling of heartbeat. Both in the case of tachycardia and bradycardia.
- Discomfort in the chest and abdomen. Pressing and aching type, radiating to the arms and shoulder blades.
- Headache in the temporal region of a pulsating nature. Follows the beat of your heart.
- Vertigo. Vestibular phenomena are possible.
- Loss of consciousness, fainting, syncope.
- Weakness, drowsiness, problems with performance.
Signs of sinus arrhythmia are of cardiac and neurological origin, caused by tissue hypoxia and impaired cellular nutrition. Objectively, this is manifested by false reflex phenomena.
Types of arrhythmias
Bradycardia
With sinus bradycardia, heart rate is recorded up to 60 beats/min or less. Subjectively, it is felt as a feeling of tightness in the chest , in particular in the cardiac region, general weakness up to loss of consciousness.
It must be remembered that a decrease in heart rate is possible in a completely healthy person during sleep or at rest and is not a pathological condition!
Bradycardia can be triggered by low blood pressure, hemodynamic disorders associated with reduced blood flow in the peripheral arteries, and hypothyroidism.
Sinus tachycardia
An increase in heart rate of more than 90 beats/min is registered and is subjectively felt by the person as a feeling of heartbeat in the chest.
This type of arrhythmia can be symptomatic and associated with temporary psycho-emotional and heavy physical stress, and be a symptom of fever during viral and bacterial infections.
Paroxysmal tachycardia
According to the ECG, the rhythm in this pathology is correct, sinus, but frequent (up to 120-240 beats/min), which is subjectively defined by a person as a feeling of pronounced heartbeat, and may be accompanied by dizziness and weakness, sweating.
Atrial fibrillation
This is a type of rhythm disorder in which the atria contract chaotically at a frequency of 350-700 beats/min (there are many pacemakers - non-sinus rhythm), which creates conditions for discoordinated contraction of the muscle fibers of the heart and manifests itself in the form of an irregular weak pulse.
With paroxysms of atrial fibrillation, the clinical manifestations can be mild, but with a long course of the disease and the absence of proper treatment, the disease goes into a more severe stage, manifested clinically by signs of heart failure (shortness of breath, discomfort in the chest, congestion in the pulmonary or systemic circulation), dizziness, general weakness, sometimes loss of consciousness.
The cause of this pathology is congenital and acquired heart defects, intoxication with harmful substances, alcohol, and medications.
Respiratory arrhythmia
This is a type of rhythm disorder in which the heart rate increases as you inhale (tachyarrhythmia), and decreases as you exhale (bradyarrhythmia). This condition can be a temporary phenomenon (during heavy physical exertion, deep and rapid breathing) and is not a pathology. It most often occurs in children and adolescents, but adults are no exception. Respiratory arrhythmia does not require special treatment and may not manifest itself clinically.
Extrasystoles
Extrasystoles are characterized by extraordinary contractions of the heart muscle. They are felt as a temporary feeling of tightness in the chest, interruptions in the functioning of the heart, or this condition does not manifest itself clinically. Can be recorded in healthy people.
Heart blocks
A type of arrhythmia characterized by a slowdown in the passage of an electrical impulse through the myocardial conduction system. The causes of this pathology may be congenital and acquired heart defects, various types of intoxication, as well as diseases that contribute to the degeneration of muscle tissue into connective tissue (cardiosclerosis, myocardial infarction, myocarditis). The main symptoms of blockades are: general weakness, dizziness, sensations of interruptions in the heart area, and in severe clinical cases even fainting and convulsions.
Blockades can be of 3 degrees depending on the severity of the condition, as well as complete and incomplete.
Methods of influence
Treatment of respiratory arrhythmia is prescribed depending on the results of the examinations. Medication is necessary only if another disease is detected in the background.
Under no circumstances should you prescribe medications on your own; doctors say that this is fraught with serious consequences. Nowadays, a method such as breathing exercises is gaining popularity. There is such a program as “Strelnikova’s gymnastics,” which is aimed at optimizing blood circulation, as well as saturating the blood vessels of the upper and lower extremities with oxygen. This method is more related to prevention, and it is not for nothing that doctors say that a disease is much easier to prevent than to treat.
A kind of training of the cardiovascular system, as well as the respiratory system, given the modern lifestyle, is very necessary. If earlier this happened in the process of physical labor, now most professions involve sitting in one position for a long time, which is also stressful. Breathing exercises are definitely very important, but certain conditions and additional time must be provided for it.
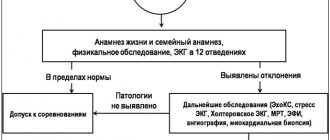
Diagnosis of arrhythmias
Quite often, many types of arrhythmias do not manifest themselves clinically, so they can be detected accidentally during a routine examination (examination by a therapist, ECG registration), or during accidental hospitalization in a hospital (during an examination).
Diagnostic methods:
- Electrocardiography
- Holter blood pressure monitoring
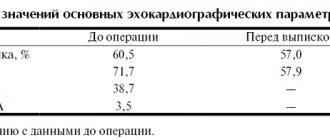
- Echocardiography
- Ultrasound examination of the heart
The gold standard in diagnosing arrhythmias is the ECG, but the disadvantage of this method is that only a certain fragment is recorded on the film, but it is impossible to monitor the work of the heart muscle over the course of a day, as with Holter monitoring. For a more thorough and detailed study of the structures of the heart and blood vessels, research methods such as echocardiography and ultrasound of the heart are used.
Principles of arrhythmia treatment
- Regular events
- Diet therapy
- Drug therapy
Must remember! Before starting treatment measures, it is necessary to know exactly the cause of this pathological condition and whether it is pathological at all. Once the cause is established, it will be easy for the doctor to select the correct treatment and avoid complications of the disease.
If arrhythmia is not an independent nosology, but a complication of any other pathological condition, then it is necessary to eliminate not the effect, but the cause that caused it.
Regular events
It is necessary to do light physical exercise (squats, light walking and swimming in the morning) to strengthen the heart muscle and improve its function. It is necessary, together with the instructor, to develop the correct set of exercises to obtain the desired effect and try to avoid excessive physical activity (lifting weights, speed running, jumping, strength training for all muscle groups)
Diet therapy
It is necessary to exclude pickled, salty, fatty and fried foods from the diet. It is worth eating as many fresh vegetables (cabbage, potatoes, beets, parsley) and fruits (apples, bananas, dried apricots, raisins) as possible, rich in vitamins and microelements that are necessary for the implementation of various metabolic processes in the body. Important! An important role in diet therapy is played by the vitamin load and consumption of foods rich in certain microelements, especially potassium (bananas, dried apricots, greens) and magnesium (legumes, seeds, nuts, avocados).
Drug therapy
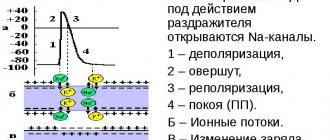
The drugs of choice are antiarrhythmic drugs that can affect the electrical activity of myocardial cells, the process of conducting an electrical impulse from one bundle to another.
There are 4 main groups of these drugs
Fast Na channel antagonists:
- 1A – increase repolarization time (“Quinidine”, “Procainamide”)
- 1B – shorten the repolarization time (“Lidocaine”, “Mexiletine”)
- 1C – do not affect the repolarization time (“Propafenone”, “Etatsizin”, “Aprindin”)
Beta blockers - block adrenergic receptors of the myocardium:
- "Concor"
- "Acebutolol"
- "Nadolol"
K channel antagonists:
- "Amiodarone"
- "Nibentan"
- "Sematilide"
Ca channel antagonists - prevent the passage of calcium ions through the channels of the same name to the muscle fibers, which reduces the contractile activity of the myocardium. There are 2 groups of these drugs:
- Non-dihydropyridine blockers: Nifedipine, Amlodipine
- Dihydropyridine blockers: Verapamil, Gallopamil
Must remember! The dosage of drugs and the method of their administration depend on the morphofunctional characteristics of the patient and the severity of his condition.
Way of life with respiratory arrhythmia of the heart
As stated above, this disease does not require any treatment, however, experts recommend that people who are prone to this condition lead a healthy lifestyle and, if possible, engage in sports.
Equally important is a healthy diet, which includes proper and healthy foods that help normalize heart function. The diet should be varied, well-balanced, preferably a predominance of seafood, raw vegetables and fruits, dairy products, herbs, etc.
Ideal conditions for normal heart function are the absence of stress and quiet activities, for example, hobbies, forest walks, yoga. Remember, if a patient with respiratory arrhythmia leads a healthy lifestyle and does not have bad habits, he will not feel any discomfort.
Prevention of rhythm disturbances
- Treatment of somatic diseases and regular medical examination for these conditions (coronary heart disease, hypertension)
- Proper balanced nutrition (products rich in vitamins and microelements);
- Light physical activity (morning exercises, walking in the fresh air, swimming), exercise therapy according to a specially designed scheme
- Correct work and rest schedule
- Categorical refusal to smoke, drink alcohol, coffee, strong tea
- Weight control (obesity prevention)
- Psycho-emotional peace