The feeling of rapid heartbeat, or tachycardia, accompanied by a very high heart rate (more than 100 per minute), can be caused by many diseases that lead to arrhythmia. Often such symptoms, together with specific changes in the electrocardiogram, are based on the anatomical features of the conduction system of the heart, which is responsible for the correct heart rhythm. The combination of such features constitutes clinical syndromes, generalized by the concept of shortening of the PQ interval.
So, shortened PQ interval syndrome is a group of electrocardiological symptoms, the basis of which is a decrease in the time it takes electrical excitation to reach the ventricles from the atria through the atrioventricular connection. This group includes Wolff-Parkinson-White syndromes (WPV syndrome)
, as well as
Clerc-Levy-Cristesco syndrome (CLC syndrome)
. These syndromes can occur at any age, even in the neonatal period, regardless of gender differences.
Indications for ECG
ECG is a non-invasive and painless research method that has no contraindications. The procedure is carried out on a planned or emergency basis.
Planned electrocardiography is prescribed:
- before surgical interventions;
- during pregnancy;
- during preventive examinations of the population;
Scheduled electrocardiography is prescribed in certain cases.
Also, periodic electrocardiography must be performed for persons with health conditions or occupational hazards:
- in the presence of atherosclerotic plaques;
- hypertension;
- elevated blood cholesterol levels;
Emergency electrocardiography is performed to identify pathological processes in the heart, some of which require immediate intervention.
An emergency ECG is prescribed for:
- sharp pain localized behind the sternum or in the upper abdomen;
- sudden onset of shortness of breath;
- heart murmurs identified during initial diagnosis;
- with discomfort in the heart.
What does an electrocardiogram consist of?
To understand the elements that make up the electrocardiogram, it is necessary to delve into the processes occurring in the heart before and during its contraction.
For the heart muscle to contract, an electrical impulse must first travel through it. During the propagation of this impulse, the muscle becomes a source of electrical current, which is conducted into the surrounding tissues and onto the surface of the body.
If electrodes are placed on both sides of the heart, the potential difference that occurs during the propagation of excitation can be recorded and displayed on paper. The resulting diagram will be called an electrocardiogram.
In practice, three methods of placing electrodes, called standard leads, are used:
- In the first lead, the electrode on the left hand is positive, and on the right hand it is negative.
- In the second lead, positive electrodes are installed on the left leg and negative electrodes on the right arm.
- In the third lead, the negative electrode is located on the left arm, and the positive electrode on the right leg.
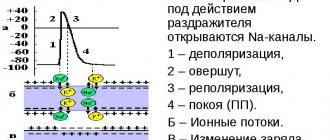
When the electrical phenomena occurring in the heart are recorded over a period of time, an image is obtained consisting of teeth, segments and intervals. The waves represent a set of positive and negative peaks and reflect the processes of changing the potential difference between the electrodes.
There are waves P, Q, R, S, T, they provide the following information:
- The P wave occurs during atrial depolarization. Depolarization is a process that precedes muscle contraction. Normally, in the second standard lead this wave is positive.
- The QRS complex consists of two negative (Q and S) and one positive (R) waves. They correspond to the process of propagation of ventricular depolarization.
- The T wave occurs when the resting potential of the cardiomyocytes (heart cells) of the ventricles returns to its original level and repolarization occurs. Normally, in the second standard lead the T wave is positive.
Segments are straight line segments connecting adjacent teeth to each other:
- The PQ segment occurs due to a delay in the impulse in the atrioventricular node; its duration can be used to judge the functioning of the conduction system of the heart.
- The ST segment corresponds to the time during which both ventricles are in a depolarized (excited) state.
The intervals consist of a tooth or several teeth and a segment:
- The value of the PQ interval is defined as the distance between the beginning of the P wave and the QRS complex. It displays the time period spent on the propagation of excitation from the atrium to the ventricles.
- The values of the QRS complexes on cardiograms are represented by the intervals from the Q wave to the S wave, and corresponds to the process of ventricular excitation.
- The QT interval refers to the distance from the starting point of the Q wave to the end of the T wave. It reflects the depolarization and repolarization of the ventricles.
How to decipher an ECG
Decoding the electrocardiogram includes assessment of intervals, waves and segments.
The duration of the intervals, the amplitude of the waves, their frequency and rhythm have strict normal limits, and deviation from these norms can indicate many pathologies. It is important to understand that only a doctor can diagnose a pathological change in an electrocardiogram, because the cardiogram readings can change.
The PQ interval on the ECG, the norm of which also has fairly strict values, can be differentiated according to the age categories of patients. Children's norms for this indicator, for example, are lower than those of adults. This factor is due to the peculiarities of children's physiology and the faster conduction of intracardiac excitation impulses.
ECG analysis
In the process of analyzing the electrocardiogram, the doctor receives information about the heart rate (HR), the main rhythm, the presence or absence of extraordinary contractions and disturbances in the conduction of the electrical impulse.
The patient should understand that many factors can influence the result of the electrocardiogram. Any stress factors, be it emotional overexcitation, physical activity or a cup of coffee before the examination, can significantly distort the real picture. Ideally, at the time of the examination, the patient should be well-rested and in a calm, non-excited state.
In order for the research results to be reliable, a number of rules should be followed:
- avoiding strong tea, coffee and energy drinks several hours before the examination;
- lack of physical and emotional stress;
- no excessive load on the gastrointestinal tract. If the procedure is scheduled for the morning, you should postpone a hearty breakfast. If the procedure is performed during the day, it is better not to eat a few hours before the ECG;
- do not worry directly during the examination. The ECG procedure is absolutely painless and harmless, and excessive emotional stress can affect the reliability of the results;
- Smoking and drinking alcohol are prohibited several hours before the examination;
- You should not use medications that affect the cardiovascular system.
A competent specialist, having seen deviations from the norm in ECG indicators, will make sure that all of the above rules are followed, and only after that will make a final diagnosis.
How does short PQ syndrome manifest?
The clinical picture of shortened PQ syndrome is caused by the occurrence of paroxysmal tachycardia, since during the interictal period the patient usually does not present any complaints from the cardiovascular system. Symptoms of tachycardia are the following:
- The sudden, sharp onset of an attack, caused by provoking factors or occurring without them, in itself,
- Feeling of a strong heartbeat, sometimes with a feeling of interruptions in the heart,
- Autonomic manifestations - severe weakness, hyperemia or paleness of the face, sweating, coldness of the extremities, fear of death,
- Feeling of suffocation or lack of oxygen, feeling of insufficient inspiration,
- Unpleasant discomfort in the heart area of a pressing or burning nature.
If the symptoms described above appear, you should definitely seek medical help by calling an ambulance or going to a clinic.
What is PQ interval
The PQ interval is the distance from the beginning of the positive P wave to the beginning of the negative Q wave (or to the positive R wave if the Q wave is not pronounced or absent). This interval reflects the process of impulse conduction from the atria to the ventricles through the atrioventricular node.
This interval reflects the time during which the electrical impulse spreads from the place where it was generated (atrium) to the ventricles, which, thanks to this “signal,” contract and push a portion of blood into the great vessels.
The atrioventricular node serves as an intermediate point through which the electrical impulse passes. Normally, it is delayed at this intermediate point in order to prevent simultaneous contraction of the atria and ventricles.
Treatment of short PQ syndrome
- The shortened PQ ,
also called the CLC phenomenon, does not require treatment. It is quite enough to correct the lifestyle and undergo regular examinations with a doctor - a cardiologist or arrhythmologist, for a child - once every six months, for adults - once a year.- Treatment of shortened PQ syndrome
(CLC - Clerk-Levi-Christesco syndrome) consists of providing first aid at the time of tachycardia paroxysm and further taking prescribed medications.
First aid can be provided by the patient independently - this is the use of vagal tests.
These manipulations are based on a reflex effect on the vagus nerve, which slows down the heart rate. Vagal tests can be used at the time of paroxysm only if the patient has had an attack of tachycardia not for the first time, he has been diagnosed and has not previously had ventricular tachycardia. In addition, vagal tests should be explained to the patient in detail by the doctor. The most effective techniques include the following:
- Straining test (Valsalva maneuver),
- Simulating a cough or sneeze
- Lowering your face into a basin of cold water, holding your breath,
- Apply finger pressure with moderate force to closed eyeballs for three to five minutes.
Restoring the correct heart rhythm
is performed by a doctor or paramedic in an ambulance and is carried out through the administration of medications intravenously. As a rule, this is asparkam, verapamil or betaloc. After hospitalization of the patient in a cardiology hospital, treatment of the underlying heart disease, if any, is carried out.
“cauterization” of pathological pathways using RFA
In case of frequent attacks of tachyarrhythmia (several per month, per week), as well as a history of ventricular arrhythmias, a hereditary history of sudden cardiac death or death from cardiac causes in young people, the patient is indicated for surgical treatment.
The operation involves applying radio frequencies, a laser or a cold factor to an additional beam. Accordingly, radiofrequency ablation (RFA), laser destruction or cryo-destruction are performed. All indications and contraindications are determined by an arrhythmologist, cardiologist and cardiac surgeon.
Many patients are interested in the possibility of permanent pacing. An pacemaker can be installed if the patient has a tendency to paroxysmal ventricular tachycardia, ventricular fibrillation and there is a high risk of clinical death with cardiac arrest (asystole). Then you can consider installing a cardioverter-defibrillator, which, unlike an artificial pacemaker, does not impose the correct rhythm, but “restarts” the heart when such fatal arrhythmias occur.
Normal PQ interval in children and adults
The PQ interval on the ECG (the norm for adults is 0.12-0.20 s) should vary strictly within a certain range. Anything that goes beyond this is pathological.
PQ interval on ECG (normal for adults and children)
However, it should be understood that the value of this parameter depends on the heart rate (the higher the heart rate, the faster the impulse propagates). Therefore, it is more correct to evaluate the nature and state of the atrioventricular connection as the ratio of the duration of the PQ interval to the duration of the entire cardiac systole (PT).
ECG in children has its own peculiarities. Differences from the electrocardiogram in adults are most pronounced at an early age; after 13-14 years, its characteristics are increasingly closer to the standard norm. The PQ interval is shorter in children, which is due to a higher heart rate compared to adults.
The PQ interval and heart rate values when deciphering an ECG for children are normally based on the following indicators:
| Age (years) | Heart rate (beats per minute) | Interval (s) |
| 0-1 | 120-140 | 0,09-0,12 |
| 1-2 | 110-130 | 0,10-0,12 |
| 3-4 | 90-110 | 0,11-0,13 |
| 5-7 | 80-105 | 0,12-0,14 |
| 8-11 | 75-95 | 0,12-0,14 |
| 12-15 | 70-90 | 0,12-0,16 |
ECG interpretation algorithm
There is a scheme for deciphering an ECG with a sequential study of the main aspects of heart function:
- sinus rhythm;
- Heart rate;
- rhythm regularity;
- conductivity;
- EOS;
- analysis of teeth and intervals.
Sinus rhythm is a uniform heartbeat rhythm caused by the appearance of an impulse in the AV node with gradual contraction of the myocardium. The presence of sinus rhythm is determined by deciphering the ECG using P wave indicators.
Also in the heart there are additional sources of excitation that regulate the heartbeat when the AV node is disturbed. Non-sinus rhythms appear on the ECG as follows:
- Atrial rhythm - P waves are below the baseline;
- AV rhythm – P is absent on the electrocardiogram or comes after the QRS complex;
- Ventricular rhythm - in the ECG there is no pattern between the P wave and the QRS complex, while the heart rate does not reach 40 beats per minute.
When the occurrence of an electrical impulse is regulated by non-sinus rhythms, the following pathologies are diagnosed:
- Extrasystole is premature contraction of the ventricles or atria. If an extraordinary P wave appears on the ECG, as well as when the polarity is deformed or changed, atrial extrasystole is diagnosed. With nodal extrasystole, P is directed downward, absent, or located between QRS and T.
- Paroxysmal tachycardia (140-250 beats per minute) on the ECG can be presented in the form of an overlay of the P wave on the T wave, standing behind the QRS complex in standard leads II and III, as well as in the form of an extended QRS.
- Flutter (200-400 beats per minute) of the ventricles is characterized by high waves with difficult to distinguish elements, and with atrial flutter, only the QRS complex is distinguished, and sawtooth waves are present in place of the P wave.
- Flicker (350-700 beats per minute) on the ECG is expressed in the form of inhomogeneous waves.
Heart rate
The interpretation of the ECG of the heart must contain heart rate indicators and is recorded on tape. To determine the indicator, you can use special formulas depending on the recording speed:
- at a speed of 50 millimeters per second: 600/ (number of large squares in the RR interval);
- at a speed of 25 mm per second: 300/ (number of large squares between RR),
Also, the numerical indicator of the heartbeat can be determined by the small cells of the RR interval, if the ECG tape was recorded at a speed of 50 mm/s:
- 3000/number of small cells.
The normal heart rate for an adult is between 60 and 80 beats per minute.
Regularity of rhythm
Normally, the RR intervals are the same, but an increase or decrease of no more than 10% from the average value is allowed. Changes in the regularity of the rhythm and increased/decreased heart rate can occur as a result of disturbances in automatism, excitability, conductivity, and contractility of the myocardium.
When the automatic function is impaired, the following interval indicators are observed in the heart muscle:
- tachycardia - heart rate is in the range of 85-140 beats per minute, a short period of relaxation (TP interval) and a short RR interval;
- bradycardia - heart rate decreases to 40-60 beats per minute, and the distances between RR and TP increase;
- arrhythmia – different distances are tracked between the main heartbeat intervals.
Conductivity
To quickly transmit an impulse from the source of excitation to all parts of the heart, there is a special conduction system (SA and AV nodes, as well as the His bundle), the violation of which is called blockade.
- How to decipher an ECG analysis, norms and deviations, pathologies and diagnostic principles
There are three main types of blockades - sinus, intraatrial and atrioventricular.
With sinus block, the ECG shows a violation of impulse transmission to the atria in the form of periodic loss of PQRST cycles, while the distance between RRs increases significantly.
Intraatrial block is expressed as a long P wave (more than 0.11 s).
Atrioventricular block is divided into several degrees:
- I degree – prolongation of the PQ interval by more than 0.20 s;
- II degree – periodic loss of QRST with an uneven change in time between complexes;
- III degree - the ventricles and atria contract independently of each other, as a result of which there is no connection between P and QRST in the cardiogram.
Electric axis
EOS displays the sequence of impulse transmission through the myocardium and normally can be horizontal, vertical and intermediate. In ECG interpretation, the electrical axis of the heart is determined by the location of the QRS complex in two leads - aVL and aVF.
In some cases, axis deviation occurs, which in itself is not a disease and occurs due to an enlargement of the left ventricle, but, at the same time, may indicate the development of pathologies of the heart muscle. As a rule, the EOS deviates to the left due to:
- ischemic syndrome;
- pathology of the valve apparatus of the left ventricle;
- arterial hypertension.
A tilt of the axis to the right is observed with enlargement of the right ventricle with the development of the following diseases:
- pulmonary stenosis;
- bronchitis;
- asthma;
- pathology of the tricuspid valve;
- congenital defect.
PQ interval pathologies
Changes in the PQ interval indicate pathologies of the cardiac conduction system. This interval can be either shortened or lengthened. In some cases, there is dissociation of the P wave from the QRS complex.
A shortening of the interval indicates a faster than normal conduction of excitation from the atria to the ventricles. This can be dangerous due to the development of tachycardia attacks.
Lengthening the interval, on the contrary, indicates difficulty in conducting excitation between the atria and ventricles. These pathologies are called atrioventricular conduction blocks. They are classified as both physiological and pathological.
Pathologies of the PQ interval are fraught with the development of tachycardia
A shortening of the interval may indicate the presence of premature ventricular excitation syndrome. This syndrome is associated with the presence of additional (abnormal) pathways through which excitation from the atria reaches the ventricles. As a result, the impulse spreads without physiological delay, faster than necessary.
There are two types of this syndrome: CLC syndrome and WPW syndrome ; they can be differentiated from each other by the characteristics of the QRS complexes. You can recognize accelerated impulse conduction on an ECG by measuring the duration of the PQ interval. Its normal values should be less than 0.11 seconds.
The PQ interval on the ECG (the norm for children is less than for adults) during diagnosis depends on the age of the patients. With this pathology, the QRS complex and the T wave remain unchanged.
The danger of this phenomenon is the possibility of developing arrhythmias (paroxysmal tachycardias). During the course of the disease without attacks of tachycardia, the patient may not realize for a long time that there are additional pathways in the heart.
An increase in the interval may occur in cases of atrioventricular blockade. There are partial (types 1 and 2) and complete (type 3) blockades. The cause of blockades can be functional or organic factors.
Functional reasons include the use of certain medications that reduce intracardiac conduction and intense exercise. Examples of organic causes are myocardial infarction, infectious diseases of the heart muscle, myocardial ischemia and heart defects.
Intense sports may cause the development of PQ interval pathologies
The PQ interval on the ECG (the norm against the background of partial blockades is violated) in the first type increases, since the conduction of excitation is slowed down, but all impulses from the atria reach the ventricles. This type of blockade is physiological and is quite often observed in young patients and athletes.
Often this type of blockade has no clinical manifestations and does not affect people’s daily lives. On the ECG, this type of blockade manifests itself as an increase in the PQ interval (duration more than 0.2 s).
If a blockade of this type is detected, it is advisable to undergo additional examination to exclude the possibility of concomitant pathologies. Treatment is not prescribed until the factors that trigger the development of the pathology are identified.
PQ interval on ECG - pathologies
In the second type of disorder, not all impulses from the atria reach the ventricles. The ECG recording clearly shows that there are no QRS complexes following some P waves. There are two variants of the manifestation of the second type of blockade: Mobitz I and Mobitz II.
Treatment of rhythm and conduction disorders at the prehospital stage
Acute arrhythmias and blockades, which can complicate the course of diseases of the cardiovascular system - ischemic heart disease (including myocardial infarction, post-infarction cardiosclerosis), rheumatic heart defects, primary and secondary cardiomyopathies, sometimes develop as a result of congenital abnormalities of the conduction system (Wolf-Parkinson-White syndromes - WPW , Launa-Genong-Levaina - LGL). Arrhythmias often occur against the background of arterial hypertension, congestive heart failure, and electrolyte disorders (for example, hypokalemia, hypomagnesemia). Their appearance can be triggered by taking medications (cardiac glycosides, theophylline; drugs that prolong the QT interval - terfenadine, cisapride), alcohol, as well as excessive consumption of caffeine-containing drinks.
At the prehospital stage, it is advisable to identify those rhythm disturbances for which emergency therapy is indicated (see table).
Paroxysmal supraventricular tachycardia
Medical tactics for paroxysmal supraventricular tachycardia (PSVT) are determined by the patient’s hemodynamic stability. A drop in blood pressure (BP) with the development of syncope, an attack of cardiac asthma, pulmonary edema, and the development of a severe anginal attack against the background of tachycardia are indications for immediate electrical pulse therapy.
With relatively stable hemodynamics, the choice of drug depends on the electrocardiographic picture (Fig. 1).
Tachycardia with “narrow” QRS complexes (unchanged QRS no more than 0.1 s) is stopped by administration of the calcium antagonist verapamil (isoptin), which lengthens the refractory period in the atrioventricular node. The drug is administered intravenously as a bolus at a dose of 2.5-5 mg over 2-4 minutes (to avoid the development of collapse or severe bradycardia) with possible repeated administration of 5-10 mg after 15-30 minutes if tachycardia persists and there is no hypotension.
Side effects of verapamil include: bradycardia (up to asystole with rapid intravenous administration due to suppression of the automatism of the sinus node); AV blockade (up to complete transverse with rapid intravenous administration); transient ventricular extrasystole (self-limited); arterial hypotension due to peripheral vasodilation and negative inotropic effects (up to collapse with rapid intravenous administration); increase or appearance of signs of heart failure (due to negative inotropic effects); pulmonary edema. From the central nervous system, dizziness, headache, nervousness, lethargy, facial redness, peripheral edema, feeling of lack of air, shortness of breath, allergic reactions are noted.
Verapamil should only be used for disorders of the QRS complex. In case of a “wide” QRS complex and suspected Wolff-Parkinson-White syndrome (WPW syndrome), the drug is contraindicated, as it shortens the refractory period of additional conduction pathways and can cause an increase in heart rate and ventricular fibrillation. Diagnosis of WPW syndrome is possible with appropriate anamnestic indications and/or by evaluating previous ECGs with sinus rhythm (PQ interval less than 0.12 s, QRS complex widened, delta wave detected). Other contraindications to the use of verapamil are:
- absolute: severe bradycardia, sick sinus syndrome, AV block II and III degrees, cardiogenic shock, chronic and acute heart failure, hypersensitivity to the drug;
- relative: bradycardia with a heart rate less than 50 per minute, AV block of the first degree, ventricular tachycardia, arterial hypotension (SBP less than 90 mm Hg).
In addition, verapamil is contraindicated in patients who have used any beta-blocker within the last two hours.
An alternative to verapamil is procainamide (procainamide); it can also be used in case of ineffectiveness of verapamil, but not earlier than 15 minutes after the administration of the latter and provided that stable hemodynamics are maintained. Procainamide is effective for reciprocal tachycardia in patients with WPW syndrome (in cases where verapamil is contraindicated). Procainamide is administered intravenously slowly at a dose of 1000 mg over 8-10 minutes (10 ml of a 10% solution, adjusted to 20 ml with isotonic sodium chloride solution) with constant monitoring of blood pressure, heart rate and ECG (in case of sharp expansion of QRS complexes, administration must be stopped). When sinus rhythm is restored, the drug administration is stopped. Due to the possibility of lowering blood pressure when administering procainamide, the patient should be in a horizontal position; it is also necessary to prepare a syringe with 0.1 mg of phenylephrine (mesatone).
Side effects of procainamide include arrhythmogenic effects, ventricular arrhythmias due to prolongation of the QT interval, slowing of atrioventricular and intraventricular conduction, arterial hypotension, dizziness, weakness, disturbances of consciousness, depression, delirium, hallucinations, allergic reactions.
Contraindications to the use of procainamide are arterial hypotension, cardiogenic shock, chronic heart failure, sinoatrial and AV blockades of the second and third degrees, intraventricular conduction disorders, prolongation of the QT interval and indications of episodes of torsade de pointes in the anamnesis, severe renal failure, systemic lupus erythematosus , hypersensitivity to the drug. The toxic effect of novocainamide is eliminated by intravenous injection of 100 ml of 5% sodium bicarbonate solution.
It is also possible to use beta-blockers (propranolol) and cardiac glycosides (digoxin), but their effectiveness in paroxysmal supraventricular tachycardia is only 40-55%. If the patient has already been administered verapamil, then propranolol (obzidan, anaprilin) can be used no earlier than 30 minutes sublingually at a dose of 10-20 mg. The drug is contraindicated in cases of arterial hypotension and bronchial obstruction syndrome. IV administration of propranolol in a dose of up to 0.15 mg/kg at a rate of no more than 1 mg/min should preferably be carried out under the control of an ECG monitor in a cardiac block. Propranolol is highly effective for paroxysmal tachycardia caused by a re-entry circle in the sinus or atrioventricular node; in other types of tachycardia, its use can reduce heart rate. Digoxin in an initial dose of 0.25-0.5 mg is effective for nodal reciprocal tachycardia, in other cases it only reduces heart rate. Digoxin is not indicated for WPW syndrome for the same reasons as verapamil.
Therapy of paroxysmal supraventricular tachycardia in a specialized cardiac intensive care unit and in a hospital can be carried out by intravenous administration of ATP (or adenosine), interrupting the circle of “re-entry”: 10 mg (1 ml of 1% solution) ATP is administered intravenously over 5 -10 s, if there is no effect, another 20 mg (2 ml of 1% solution) is reintroduced after 2-3 minutes. When using adenosine (adenocor), the initial dose is 3 mg (1 ml). The effectiveness of the drug for this type of rhythm disturbance is 90-100%. As a rule, it is possible to stop paroxysmal supraventricular tachycardia within 20-40 s after ATP administration.
IV administration of adenosine also makes it possible to differentiate between atrial flutter with 1:1 conduction and supraventricular tachycardia; inhibition of AV conduction makes it possible to identify characteristic flutter waves, but the rhythm is not restored.
Contraindications to the use of the drug are AV block of the second and third degree, sick sinus syndrome (in the absence of an artificial pacemaker), increased sensitivity to adenosine. It should also be taken into account that the administration of ATP or adenosine can provoke an attack in patients with bronchial asthma.
It must be taken into account that intravenous administration of a bolus of adenosine (ATP) during supraventricular paroxysms in approximately 50% of cases leads to 5-15 second asystole, and in 0.2-3% of cases asystole can last for more than 15 s, which can require a precordial blow and even chest compressions (only a few massage movements are required). Due to the risk of developing such complications, the use of adenosine (ATP) is permissible only in a specialized intensive care unit or in a hospital.
Atrial fibrillation and flutter
When treating patients with atrial fibrillation and flutter at the prehospital stage, the feasibility of restoring sinus rhythm should be assessed.
The absolute indication for restoration of sinus rhythm during the development of paroxysm of atrial fibrillation is the development of pulmonary edema or arrhythmogenic shock; in this case, emergency cardioversion should be performed prehospital.
Contraindications to the restoration of sinus rhythm at the prehospital stage include the duration of paroxysm of atrial fibrillation for more than two days, proven dilatation of the left atrium (antero-posterior size 4.5 cm, according to echocardiography), the presence of blood clots in the atria or a history of thromboembolic complications, the development of paroxysm on background of acute coronary syndrome (in the presence of stable hemodynamics), development of paroxysm against the background of severe electrolyte disturbances, decompensation of thyrotoxicosis. If you refuse to restore sinus rhythm, it is necessary to establish control over the heart rate in order to maintain it within 60-90 beats per minute.
The drug of choice for controlling heart rate is cardiac glycosides: 0.25 mg of digoxin (1 ml of 0.025% solution) in 20 ml of isotonic sodium chloride solution is administered intravenously as a slow bolus. Further tactics are determined in the hospital. A permanent normosystolic form of atrial fibrillation without signs of heart failure does not require antiarrhythmic therapy at all (Fig. 2). Side effects of digoxin (manifestations of digitalis intoxication) - bradycardia, AV block, atrial tachycardia, ventricular extrasystole, anorexia, nausea, vomiting, diarrhea, headache, dizziness, blurred vision, syncope, agitation, euphoria, drowsiness, depression, sleep disturbances , confusion.
Contraindications to the use of digoxin:
- absolute: glycoside intoxication, hypersensitivity to the drug;
- relative: severe bradycardia (negative chronotropic effect); AV blockade of II and III degrees (negative dromotropic effect); isolated mitral stenosis and normo- or bradycardia (danger of dilatation of the left atrium with worsening left ventricular failure due to increased pressure in its cavity; risk of developing pulmonary edema due to increased contractile activity of the right ventricle and increased pulmonary hypertension); idiopathic hypertrophic subaortic stenosis (possibility of increasing obstruction of the left ventricular outlet due to reduction of the hypertrophied interventricular septum); unstable angina and acute myocardial infarction (the danger of increasing myocardial oxygen demand, as well as the possibility of myocardial rupture during transmural myocardial infarction due to increased pressure in the cavity of the left ventricle); WPW syndrome (improves conduction along accessory pathways), frequent or polytopic ventricular extrasystole, jogging ventricular tachycardia.
The drug of choice for restoring sinus rhythm in stable hemodynamics is procainamide.
In some cases, verapamil can serve as an alternative to procainamide. It does not always restore sinus rhythm, but effectively reduces heart rate by blocking the atrioventricular node. We must not, however, forget that for atrial fibrillation in patients with WPW syndrome, the use of verapamil is not indicated (the drug improves conduction along additional pathways).
In case of magnesium-dependent atrial fibrillation (proven hypomagnesemia or the presence of a prolonged QT interval), the drug of choice is magnesium sulfate (cormagnesin), which in other cases is an additional agent for slowing down (reducing the frequency of contractions) the rhythm.
If one antiarrhythmic drug is ineffective, drug therapy at the prehospital stage is stopped; in case of complications (see above), electrical pulse therapy is performed.
Atrial flutter with low atrioventricular conduction leading to mild tachycardia, and in the absence of complications, does not require emergency treatment.
In case of unstable hemodynamics, the development of complications due to atrial flutter with a high heart rate (AV conduction 1:1), emergency electropulse therapy is indicated.
Uncomplicated atrial flutter with a high ventricular rate in the prehospital phase requires only slowing the heart rate, for which digoxin or verapamil is used. The use of beta-blockers in this case is least advisable, although possible.
Ventricular arrhythmias
In most cases, both ventricular and supraventricular extrasystole are not “malignant” rhythm disturbances and do not require immediate therapeutic intervention (the exception is frequent and/or polytopic ventricular extrasystole during myocardial infarction). In this case, oral beta blockers may be an option. From today's perspective, it is optimal to prescribe selective drugs with lipophilic properties. The most studied drug in this group is metoprolol, the use of which in a daily dose of 50–200 mg (in two doses) is recommended primarily for patients in whom extrasystole is a manifestation of coronary artery disease and/or accompanies arterial hypertension.
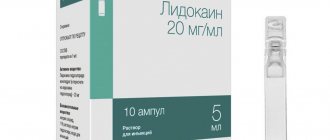
In acute myocardial infarction, the drug of choice for stopping ventricular arrhythmias is lidocaine (Fig. 3).
In conditions of stable hemodynamics, the drug of choice for stopping ventricular tachycardia (VT) is lidocaine, administered intravenously as a bolus at a dose of 1-2 mg/kg (80-100 mg) over 3-5 minutes, followed by a maintenance drip infusion for up to 24 minutes. 36 hours at a rate of 20-55 mcg/kg/min (maximum 4 mg/min). If necessary, during the infusion, an additional jet injection of lidocaine at a dose of 40 mg is acceptable 10-30 minutes after the first bolus. Prolongation of the QT interval and increase in its dispersion are indications for intensifying maintenance therapy by drip administration of cormagnesin (magnesium sulfate) at a rate of 3-20 mg/min. In the future, it is possible to switch to prophylactic intramuscular administration of lidocaine at a dose of 2-4 mg/kg (160-200 mg, maximum 600 mg, and in case of myocardial infarction no more than 300 mg) every 4-6 hours.
If lidocaine is ineffective, the use of other antiarrhythmics to stop VT is indicated if stable hemodynamics are maintained and there are no adverse reactions (risk of collapse and potentiation of the arrhythmogenic effect of antiarrhythmic drugs) or when electrical pulse therapy is impossible. In these cases, the second most important drug is procainamide (procainamide), administered with appropriate precautions intravenously in fractional doses of 100 mg/5 min until sinus rhythm is restored or a saturating dose is reached (500-1000 mg).
The effectiveness of procainamide in all paroxysmal tachycardias makes it the drug of choice for the treatment of tachycardia of unknown origin with a wide QRS complex (ventricular or supraventricular with conduction aberration).
The drug of choice for ventricular tachycardia of the “pirouette” type and an additional drug for other types of ventricular tachycardia (including those refractory to therapy with lidocaine and procainamide) is magnesium sulfate (cormagnesin), administered intravenously over 10-15 minutes at a dose of 400-800 mg of magnesium (20-40 ml of 10% or 10-20 ml of 20% solution). If there is no effect, the drug is re-administered after 30 minutes. Once the effect is achieved, maintenance therapy consists of drip administration of cormagnesin (magnesium sulfate) at a rate of 3-20 mg/min for 2-5 hours.
Ventricular tachycardia with unstable hemodynamics requires immediate electrical impulse therapy (Fig. 4).
Bradyarrhythmias
Bradyarrhythmias (sinus bradycardia, sinoauricular block, slow atrioventricular replacement rhythm, atrioventricular conduction disturbances of degree II and III) require treatment in cases where these conditions are accompanied by unstable hemodynamics and arise as a complication of organic heart damage or develop during resuscitation measures, as well as during the appearance of frequent attacks of Morgagni-Edams-Stokes. To restore hemodynamics, it may be sufficient to increase the heart rate intravenously by administering a 0.1% solution of atropine sulfate in a dose of 0.3-1.0 ml, repeating the initial dose (if effective) after 4-5 hours.
Side effects of atropine include dry mouth, thirst, nausea, vomiting, intestinal atony and constipation, increased cough in patients with bronchial asthma, urination disorders, mydriasis, photophobia, paralysis of accommodation, tachycardia, anxiety, tremor, headache, psychomotor agitation.
Contraindications to the use of atropine are glaucoma, chronic urinary retention, intestinal atony, tachycardia, severe heart failure, severe atherosclerosis, and hypersensitivity to the drug. For bradyarrhythmias and AV blockades, it is permissible to use atropine for vital indications, even in case of myocardial ischemia, intestinal obstruction, intestinal atony, liver and kidney diseases, and angle-closure glaucoma.
The ineffectiveness of atropine therapy is an indication for temporary cardiac pacing, and if it is impossible for health reasons, orciprenaline is used (at a dose of 10-30 mcg/min under heart rate control, intravenous drip until a therapeutic effect appears).
O. B. Talibov, Candidate of Medical Sciences A. V. Topolyansky, Candidate of Medical Sciences
Mobitz I
This type of blockade of the second type can be physiological for young people and athletes. On the ECG it appears as an increase in the PQ interval with each contraction. The interval increases until the atrial impulse is blocked (this is shown on the cardiogram as the absence of the QRS complex).
Also, as with the first type of blockade, patients may not suspect the presence of disturbances in the conduction system of the heart and may not experience any clinically manifested symptoms.
If a second-degree block of Mobitz type I is detected, a re-examination should be carried out , including 24-hour heart rate monitoring and a repeat electrocardiogram. Treatment is prescribed after identifying the cause of the blockade.
Mobitz II
This type is always pathological. The pulse travel time is constant, but the pulses are periodically blocked. This is reflected as the absence of some QRS complexes. Most often, a violation of the passage occurs on every third (3:1) or fourth (4:1) excitation. In severe cases, the blockade occurs every second contraction (2:1).
The condition of patients with this pathology can be very different. Some patients note a sharp deterioration in their condition, darkening of the eyes, coinciding with the loss of the QRS complex. A number of patients may not even be aware of the presence of these problems.
The severity of the blockade and the risk of transition to a complete blockade (third degree blockade) depends on the causes of the development of the pathology. Treatment is also prescribed based on the etiology of the disease. Blockade of the third type is characterized by complete disruption of impulse conduction. On the cardiogram, this appears as a separation between the P waves and the QRS complexes.
Cardiac activity in such patients is maintained by the rhythm generated by the ventricles. Depending on the cause of the development of third-degree blockade, treatment methods can be either medicinal or surgical (implantation of a pacemaker). If this type of block is congenital, most patients do not require a pacemaker.
Disturbances in the conduction system of the heart can cause sudden cardiac arrest and death. These disorders can be either congenital or acquired.
In the case of acquired diseases, early diagnosis and correctly prescribed treatment can affect a favorable outcome of the disease. That is why an ECG should be performed periodically to make sure that its indicators (in particular the PQ interval) are normal.
Materials for electrocardiography analysis
Options for changing the
U
Pronounced
U .
This variant may be associated with hypokalemia.
Negative
U .
Wave inversion may be a manifestation of heart disease.
Options
QT
interval Prolonged
QT .
It indicates prolongation of ventricular repolarization, which indicates a longer period of relative refractoriness.
Prolongation of the QT interval can be congenital or familial. It may also be a consequence of the use of medications, especially type I antiarrhythmic drugs. Most commonly seen in myocardial ischemia or infarction, a prolonged QT interval may indicate a life-threatening ventricular arrhythmia (eg, torsade de pointes). Shortened QT .
May be due to hypercalcemia or toxic effects on the myocardium of cardiac glycosides.
Options for changing the
T
Negative wave
T.
Considered normal in lead aVR. In leads III ,
Vx and V2, both negative and positive T waves are considered normal. However, a negative T wave in leads I,
II ,
V35 or V6 may indicate myocardial ischemia.
Pointed T wave.
Also known as tenting, the T wave indicates hyperkalemia or myocardial ischemia.
Heavily serrated T wave.
In children, severe is a variant of the norm; in adults, it may indicate the presence of pericarditis.
High or low T wave.
Occurs with electrolyte disturbances.
T wave
bulges.
The P wave may be hidden within the T wave. When this occurs, atrial depolarization occurs, indicating that the impulse is originating from a location above the ventricles.
Options for changing the
ST
ST segment elevation .
Segment elevation of 0.2 mV or greater above centerline indicates myocardial injury.
Decreased
ST .
Indicates myocardial injury or ischemia.
ST segment changes .
May occur with pericarditis, myocarditis, left ventricular hypertrophy, pulmonary embolism and electrolyte disturbances. These changes can also be observed in patients taking drugs that disrupt the processes of depolarization and repolarization, such as antiarrhythmic drugs (amiodarone).
Options for changing
QRS
complex Extended
QRS
(more than 0.12 s). Such a complex can be observed in conditions with slow conduction of the impulse to one of the ventricles (bundle branch block) and conditions in which the impulse is formed in the ventricles (premature contraction of the ventricles, idioventricular rhythms and ventricular tachycardia).
Variants of the shape of the
QRS .
Impaired intraventricular conduction will be reflected in the shape of the QRS complex. With a bundle branch block, for example, an additional R wave, designated R', or an additional S wave, designated S', may appear.
Varying
QRS .
If the amplitude and outline of the complex varies from cycle to cycle, this indicates the presence of an ectopic or aberrant source of impulses.
Dropped
QRS .
If the QRS complex does not appear after each P wave, conditions in which ventricular depolarization does not occur (AV block or ventricular asystole) should be suspected.
Options for changing the
PR
Shortened
PR .
This option indicates that the impulse originates somewhere other than the SA node. A shortening of the interval is characteristic of atrioventricular arrhythmia and premature ventricular excitation syndrome.
Extended
PR .
A lengthening of the interval indicates that there is a delay in the passage of the impulse through the AV node. This is accompanied by atrioventricular block of the first or second degree.
Options for changing the P wave
Pointed R wave.
An increase in the amplitude of the P wave can be observed with hypertrophy of the right atrium.
Wide double-humped R wave.
Observed in left atrial hypertrophy, this wave may appear in leads I, II, III and aVF. The first peak indicates depolarization of the right atrium, the second - depolarization of the left atrium.
Inverted P wave.
Inversion in all leads except aVR may indicate that the SA node is not a pacemaker and that the electrical impulse through the atrium is traveling in the opposite direction. An inverted P wave is usually found in atrioventricular arrhythmias. All cases where the positive sinus P wave suddenly becomes inverted indicate retrograde propagation of the electrical impulse.
Variable R wave.
If the shape and size of the P wave varies, this means that impulses can occur in different places, as in an atopic rhythm. Other reasons for this phenomenon may be increased excitability of the atrium tissue and the lesion localized near the SA node.
Prolapsed R wave.
If the P wave does not precede every QRS complex, this may indicate third-degree AV block or output block.