Violation of the functional activity of blood vessels is a common problem in cardiological practice. Mainly of organic origin, defects lead to the impossibility of adequate blood circulation in the tissues. Is it dangerous.
Aortic thickening is not a diagnosis. We are talking about a random clinical finding obtained as a result of an instrumental study. Objectively, it represents hypertrophy (proliferation) of tissue throughout the entire thickness of the vessel structure.
Contrary to possible misconception, this is not good. Rigidity (decrease in elasticity) affects the vessel’s ability to withstand enormous loads.
It is possible and even probable that many dangerous complications will develop: from an aneurysm to an instant rupture with massive bleeding and death in a matter of seconds.
If the aorta is compacted, this means that there is a third-party pathology; the deviation is not primary, it is always caused by another disease.
The vast majority of cases are associated with tuberculosis, arterial hypertension and atherosclerosis. Accordingly, therapy for the underlying condition is indicated.
Development mechanism
The basis of the pathological process is destruction of the aortic wall or a constant increased impact on the structure.
In the first case, we are talking about infectious-inflammatory, less often autoimmune processes. As a result of the constant violation of the anatomical integrity of the endothelium and other tissues, severe scarring occurs.
Epithelization leads to a gradual overgrowing of the lumen with dense connective tissue and its narrowing. The blood flow weakens, and the pressure in the local area becomes higher due to the need to overcome a mechanical obstacle.
The second factor is approximately identical, in terms of creating excess load on the walls of blood vessels. The main etiological point is an increase in blood pressure and the constant preservation of tonometer readings at consistently high numbers.
Both options pose a colossal danger to human life and health.
Organic disorders are difficult to treat, and not every doctor is ready to take on such unpredictable cases. Therefore, the logical solution would be to carry out treatment in the early stages, when there are no anatomical abnormalities yet.
Causes
There are both fundamental factors and risk factors that do not directly determine the development of the pathological process. First group:
Current or previous tuberculosis
This is a dangerous infectious disease. It is provoked by mycobacterium, also called Koch's bacillus. Can exist for a long time without symptoms. The clinic is already formed at pronounced stages.
Damage to the aorta is a complication, the prevalence is up to 25% of the total number of cases. Timing does not matter; involvement is possible at the very first stages, which affects the overall forecast.
The walls of the vessel are destroyed and scarred, the lumen narrows, and the process progresses independently. Recovery is possible only with comprehensive treatment of tuberculosis in a hospital setting.
The total duration of supervision is 6-12 months. Hospital stage - no more than 3. The rest of the period is spent on outpatient care. Throughout the rest of life, the patient should be monitored for relapses.
Syphilis
Danger does not come immediately. This sexually transmitted infection can be transmitted non-sexually, but the likelihood of this option is extremely low.
Urgent treatment of the condition is required. Because aortic damage occurs in approximately 30% of situations.
Thickening of the aortic walls does not occur immediately; it is a later complication. There are known cases of the development of a delayed phenomenon after 10-20 years from the conditional cure of syphilis.
Therefore, such patients are recommended to undergo at least echocardiography every 6 months and closely monitor their well-being.
Aortitis
Inflammatory process in the corresponding vessel. Relatively rare. Again, as a consequence of an infectious disease.
It is a complication of herpes, damage by pyogenic flora, and septic myocarditis. In rare cases, it develops as a result of autoimmune pathologies. For example, rheumatism or vasculitis.
Inflammatory diseases need to be treated in a timely manner, because the likelihood of complications is significant.
Aortitis can be treated with antibiotics or immunosuppressants, depending on the etiology of the process. In any case, hospitalization in a cardiac hospital is indicated.
Hypertension
Stable increase in blood pressure. It occurs for many reasons, which themselves require identification and qualified assessment by doctors.
At the first stage of deviation, when the disease is still unstable in its manifestations, there is a chance for normalization. As the condition progresses, the risks of impairment increase. The third degree of hypertension cannot be treated.
As mentioned, hardening of the aorta of the heart is the result of degeneration, excessive stress on the walls, or a combination of these factors.
In the absence of therapy, there is a high probability of vessel rupture. Sooner or later this will happen. Specific medications are prescribed to lower blood pressure (ACE inhibitors and others, as indicated).
Age-related changes
Violation of the functional activity, anatomical characteristics of the connective tissue that makes up the aorta and its walls. Mainly appears to be the result of age-related changes.
Variations are possible. The same phenomena are observed in diabetes mellitus, genetic pathologies, anomalies of intrauterine development with spontaneous features.
Atherosclerosis
There are two types.
- The first is a narrowing of the vessel, stenosis. Occurs in smokers, alcoholics, drug addicts, and people with arterial hypertension. It is a complication and requires urgent help. If the process is stable, surgery may be required if conservative methods do not have an effect.
- The second option is occlusion or blockage of the vessel with a cholesterol plaque. The result of a disorder of lipid metabolism in the body. It is less dangerous because the condition develops over months or even years.
Gradually, the formation becomes calcified and becomes covered with mineral salts. Such an atherosclerotic plaque cannot be dissolved with statins. Surgical treatment is required.
Aortic valve stenosis
The answer to the question of aortic stenosis, what it is, is quite simple - it is a narrowing or blockage of the aortic valve, which occurs when the valve leaflets become covered with deposits. Such deposits change the shape of the leaflets and reduce blood flow through the valve. The left ventricle must work to compensate for the decreased blood flow. Over time, the extra work to overcome this narrowing can weaken the heart muscle.
Risk factors
And the corresponding groups with an increased likelihood of developing compaction:
Physical inactivity
Insufficient physical activity of a person. It is common both for bedridden patients confined to a wheelchair and for persons leading a sedentary lifestyle. Which is the majority these days.
Blood stasis develops, general hemodynamics are disrupted. A hardening of the aorta is a possibility, but not the only problem.
To reduce the risks of the process, at least an hour of walking or cycling is enough. More is possible, at the discretion of the person himself. If there are no contraindications.
Excessive physical activity
Leads to an increase in blood pressure, the release of inadequate amounts of cortisol, strerlide hormones and catecholamines.
This provokes a narrowing of the lumen of blood vessels, including the aorta. Blood flow is disrupted, and the load on structures increases. The body is forced to resist.
In general, the thickening of the aortic walls is a compensatory mechanism aimed at preventing rupture as a result of excess load.
Obesity
It is not increased body weight that has an effect, although it plays a role. Responsibility lies with disruption of normal lipid metabolism. Fats are deposited (deposited), there is no rapid catabolism, that is, breakdown.
The excess enters the bloodstream. Due to their structure, lipids are well attached to blood vessels. Then the process continues, the formation grows, the walls of the aorta thicken and lose elasticity.
The disorder can only be stopped with the help of drugs, statins. A change in diet is also indicated. Less fat and easily digestible carbohydrates, more protein, plant foods.
Excess weight causes an increase in blood pressure, acceleration of cardiac activity due to the high load on the muscles (just imagine who will have it easier: a person with empty hands or someone carrying a bag of potatoes).
Diabetes
Causes generalized disruption of all organs and systems. Including circulatory.
The process is twofold. On the one hand, there is a stable narrowing of the aorta and other structures, on the other, a violation of lipid metabolism. Atherosclerosis develops.
The likelihood of death from blood vessel rupture increases without treatment every month, if not daily. Therefore, timely diagnosis of endocrine disease is necessary.
Smoking
Long lasting. Against the background of constant consumption of tobacco, tar, and cadmium compounds, a physiological addiction of the body is formed. Stenotic atherosclerosis develops.
Even after giving up the bad habit, spontaneous regression of narrowing does not occur. Treatment is needed. Considering that many return to addiction, the likelihood of further development of pathology increases.
Finally, alcoholism and the use of psychoactive substances have an effect. Many drug addicts do not have time to live to see either a rupture or an aortic aneurysm. Death occurs from heart failure much earlier. Alcoholics have a better chance.
Reasons are being eliminated gradually. One at a time during the diagnosis.
Symptoms
There are no such manifestations. If the walls of the aorta are compacted, there is no clinical picture. Signs and disturbances in well-being arise later, after complications of the pathological process.
Organic changes, such as an aortic aneurysm, give the following moments:
- Pain syndrome. Localization and nature depend on the location of the violation. If the abdominal region is affected, there is discomfort in the abdomen, and in the chest there is a pressing, burning sensation. If the aortic arch is compacted, there is pain in the neck, turning into discomfort at the location of the heart.
- Dyspnea. Disruption of a natural physiological process.
Further manifestations depend on which area has undergone changes.
Abdominal:
- Nausea, vomiting, heartburn, belching, other dyspeptic symptoms. Such patients are falsely sent to gastroenterology.
- Increased gas formation in the intestines.
- Pulsating sensations in the abdomen.
Arc, descending section:
- Inability to swallow normally.
- Violations of voice, timbre and general ability to speak.
- Excessive saliva production.
- Weakness.
- Numbness of the upper and lower extremities. In exceptional cases, paresis and paralysis occur. This is the result of compression of the nerve roots.
Such conditions require urgent treatment; irreversible changes in the musculoskeletal system are possible.
Compaction of the aortic root and ascending section:
- Chest pain.
- Dyspnea.
- Abnormal heart rate, other arrhythmias.
- Cephalgia, vertigo.
- Loss of consciousness, fainting.
Classic signs of damage to cardiac structures.
Attention:
You cannot focus on symptoms when identifying the causes of poor health. These are unreliable clinical signs.
Endovascular interventions
They allow you to dramatically reduce the amount of surgical trauma, shorten hospitalization periods and reduce the inevitable suffering of the patient associated with surgical approaches. One of the main disadvantages of the method is the need for repeated interventions.
Types of endovascular operations for aortic aneurysm:
- implantation of a stent graft into the abdominal aorta,
- implantation of a stent graft into the ascending (thoracic) aorta.
The most modern method of treating aortic aneurysm is a hybrid method, which allows achieving optimal treatment results with the least surgical trauma.
Hybrid surgeries combine the advantages of open and endovascular interventions.
To prevent the development of aortic aneurysms, the most important thing is the need to control risk factors, namely arterial hypertension. In addition to arterial hypertension, the most significant risk factors are age (over 55 years), male gender, smoking, the presence of aneurysms in direct relatives, and high cholesterol levels.
Diagnostics
It takes place on an outpatient basis, under the supervision of a cardiologist or vascular surgeon. The following activities are shown:
- Oral interview with a person. To get a rough picture.
- Anamnesis collection. Family history, addictions, past pathologies.
- Measurement of blood pressure and heart rate.
- Echocardiography. One of the first methods. Gives an idea of the state of the muscular organ itself and the ascending aorta, arch.
- Aortography. Targeted assessment of the largest vessel. It is used both to verify the diagnosis and to determine the effectiveness of the treatment.
- MRI. Used to clarify the localization of the pathological focus. Typically, tomography is prescribed before surgery as an informative way to visualize tissue.
- ECG. To identify functional disorders that inevitably arise at advanced stages of changes in the aorta.
- Ultrasound of the abdominal cavity.
- Plain chest x-ray.
Methods provide nuggets of valuable information. To get a complete picture, you need to carry out all these activities. They are not dangerous and painless. Therefore, it is not recommended to hesitate.
Diagnostic procedures
Diagnosis of the described pathology includes several stages:
- To begin with, the patient undergoes the necessary tests and is examined for the presence of infections.
- During an auscultatory examination, the doctor may hear changes in the sounds of the aorta and note the appearance of a characteristic noise.
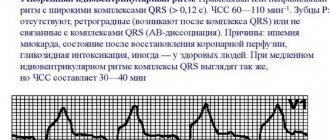
- X-ray examination and fluorography are informative. The aorta is thickened (you already know what this means and why it develops), its shadow in the image is elongated, and a pathological turn or an uncharacteristic bend along the course of the vessel may appear.
- The gold standard today is contrast angiography. During this procedure, the doctor can study the characteristics of blood flow and see certain deviations.
- Ultrasound examination and Doppler sonography are also performed.
- If the doctor needs additional information, the patient is sent for magnetic resonance imaging. Using three-dimensional images, the doctor can carefully examine and study the structure of the aorta and nearby organs.
Treatment
Depends on the primary diagnosis. The goals of therapy are to prevent complications and eliminate the origin of the condition. Medicines are used.
Which ones are determined by the doctor based on the underlying disease:
- Antihypertensive. ACE inhibitors, calcium antagonists, centrally acting agents, beta blockers, mild diuretics.
- Statins. They dissolve cholesterol and prevent its further deposition on the walls of blood vessels.
- Thrombolytics, antiplatelet agents. They prevent blood from stagnating, improve its fluidity and rheological properties, and prevent the formation of dangerous clots.
- Antituberculosis drugs. Also medications for the treatment of syphilis.
Surgery is required when a threatening aneurysm forms due to calcification of the cholesterol plaque. At the discretion of the specialist after careful consideration of all options.
A change in diet is shown throughout life. Less fat, easily digestible carbohydrates, more protein and plant foods, walking, minimal physical activity, proper rest at night. Issues of lifestyle correction are also resolved by a specialist.
Forecast
{banner_banstat9}
In itself, aortic thickening is not a diagnosis, but just an instrumental finding. You can say anything concrete after assessing the root cause.
The following factors play a major role:
- Dynamics of deviation. Progression is associated with more severe general condition and outcome.
- The age of the person. Elderly people have a relatively unfavorable prognosis.
- Family history. If there was at least one representative in the family with the condition in question, it is necessary to carefully check every six months. In such individuals, the anomaly progresses rapidly. Therefore, delay reduces the chances of successful treatment.
- The presence of concomitant somatic pathologies. Among the especially dangerous ones are hypertension, diabetes mellitus, metabolic syndromes, and atherosclerosis.
- Possibility and necessity of radical treatment. If surgery is required, the prognosis is initially worse. Further, everything depends on the success of the therapy. The absence of such a need gives a better outcome, although it does not guarantee it.
In general, even an aneurysm, as one of the most severe complications, is associated with a survival rate of 85-90%.
Attention:
Heart failure and circulatory disorders in the brain reduce the patient's chances by 30-40%.
Atherosclerosis of the aorta: prevention
Proper prevention is one of the key conditions for successful recovery, which cannot be neglected:
- Stop smoking and drinking alcohol
- Avoid foods and dishes containing animal fats
- Treat concomitant diseases in a timely manner if you have them: diabetes mellitus, arterial hypertension, obesity
- Lead an active lifestyle, move more, play sports, but do not overwork your body
- Don't be nervous about trifles
- Cure infectious diseases in a timely manner
- Get annual checkups and examinations, especially if you are over 40 years old
Complications
{banner_banstat10}
Possible consequences:
- Thrombosis. The formation of a clot in one of the arteries, sometimes in the aorta itself. Causes local ischemia. When torn off and moved along the riverbed, it often blocks the pulmonary vessel and coronary structures, which immediately leads to death.
- Aneurysm. Wall protrusion. It is observed against the background of stable degeneration and dystrophy of aortic tissue.
- Rupture, delamination. Leads to death within a matter of seconds. There were cases to the contrary, but they were casuistic. There are hardly more than 0.5%.
Thickening of the aortic walls is not an independent disease. It is not considered a diagnosis and is not represented in the ICD-10 classifier. This is a consequence, an accidental find.
After eliminating the root cause, there is every chance to stop the progression and achieve results without affecting the quality and length of life.