General information about heart defects in children
Heart disease
- a violation of the anatomical structure of the walls or valves of the heart, as well as the blood vessels that enter or exit it. Cardiac function and hemodynamics in the entire circulatory system are impaired.
Depending on the reasons for development, there are congenital
and
acquired vices
.
It is believed that congenital ones appear during the first weeks of pregnancy during the “initial formation” of future life. The reasons for the development of defects have not been studied reliably, but they predispose to them:
- genetic diseases (50% of children with Down syndrome suffer from this disorder);
- diabetes mellitus in a pregnant woman;
- bad habits of the expectant mother (half of children with fetal alcohol syndrome (FAS) have heart defects);
- infections (a mother who has had rubella in the first trimester will almost always have a child with severe pathology);
- taking medications prohibited for pregnant women;
- phenylketonuria in an expectant mother.
However, heart disease does not always develop from birth. It can manifest itself as a complication of diseases suffered in childhood (rheumatism, influenza, tonsillitis) in severe forms. This disorder is called an acquired defect.
hearts.
Degrees of heart defects in a child
Depending on the severity of the symptoms of heart disease, there are four degrees of impairment:
- first degree
- heart function deviates slightly from the norm; - second degree
- symptoms of the disease appear, parents can notice them; - third degree
- in addition to specific symptoms, disturbances in the functioning of the nervous system appear, as a result of a lack of oxygen to the brain; - fourth degree
- respiratory and cardiac activity is inhibited, such changes can lead to the death of the child.
Congenital heart diseases that cause disability
The heart is one of the most important elements of the human body, ensuring its vital functions. The heart is an organ consisting of muscles and the work of which is like a pump that delivers blood to all tissues and organs.
Medicine is now developed at a decent level, so there is always hope, even with the most complex heart diseases, even if not completely cured, but to provide a person with a quiet life, making every effort to fight the disease.
The number of heart diseases increases every year. A person is exposed to regular stress, which affects the functioning of the cardiovascular system. Also, poor-quality ecology, disrupted diet, and its inferiority have a great impact on heart health. Such factors in any case affect the functioning of the heart, causing various diseases that cause disability.
Diseases that are congenital are described as a malformation or defect of the heart or blood vessels. Congenital heart disease can be caused by various reasons, among which the main ones can be identified:
- first of all, it can be transmitted hereditarily, that is, genetic predisposition. It is more likely to occur if the mother has a heart defect. In the case when a family already has a child who has a congenital heart defect, and the disease was not detected in the parents, this determines a high probability that another baby may be born with the same disorders;
- if a child was born with genetic disorders, for example, Down syndrome;
- heart defects can be provoked if during pregnancy a woman used drugs or alcohol in excess;
- if while carrying a child the woman was exposed to severe infectious diseases.
Medical reference books list more than one hundred heart diseases that are congenital. The most common diseases among them are:
- mitral heart defects. These include mitral stenosis and mitral valve regurgitation. These heart defects are caused by disturbances in the functioning of the heart valve system. The most common defects of this type are stenosis and insufficiency;
- arterial valve defects. If the functioning of the arterial valve is disrupted, blood is able to enter the left ventricle without possible obstacles. The reason for this may be a pathology of valve “doors” that cannot close the duct. With aortic stenosis, there is increased pressure in the section where impaired blood circulation into the aorta from the left ventricle occurs;
- heart defect Tetralogy of Fallot. This defect is the most common among congenital cyanotic heart defects. This defect is also distinguished by its complexity, since it simultaneously represents four anomalies: dextraposition of the aorta, subaortic ventricular septal defect, right ventricular hypertrophy and right ventricular outflow stenosis.
It is noted that not every time even an ultrasound examination of the fetus can reveal disturbances in the cardiovascular system of a developing organism, which is why congenital heart diseases are dangerous. The survival rate of a child born with congenital heart disease depends on the severity of the case.
Heart diseases that lead to varying degrees of disability:
- third stage of hypertensive heart disease. If changes of an organic nature are observed that are not treated, occurring in the fundus of the eye, kidneys, central nervous system and heart muscle.
Hypertensive heart disease is caused by a regular increase in blood pressure. If the disease has reached the third stage, then there is a constant increase in pressure, which is accompanied by crises. They, in turn, can cause more serious circulatory disorders in the brain, and paralysis often develops;
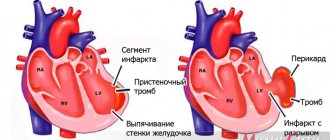
— disability is received by persons who have suffered a myocardial infarction, as well as those who suffer from severe coronary insufficiency, when significant changes occur in the heart muscle and blood circulation is impaired (third degree);
- heart defects, which are marked by narrowing of the left atrioventicular orifice, aortic valve defects, combined defects, which are accompanied by persistent third-degree circulatory disorders.
To cure a newborn baby with Tatrad Fallot defect, only the intervention of surgeons is necessary. But this does not guarantee that the baby will live to see his birthday, since there is a 75% mortality rate in this case. With such indicators, only 5% of patients can live to be fifty years old.
Normal heart function depends on various factors. The mother plays a major role in human health, giving new life. The more a mother worries about the health of her body, the less likely the child will have birth defects.
Tell! Is a child diagnosed with “CONGENAL ANOMALITY OF DEVELOPMENT” eligible? KIDNEY, SMALL ANOMALY OF DEVELOPMENT. HEARTS » disability
You wrote the diagnosis incompletely. What is the anomaly? UPS
with signs of heart failure, they give
disability
. If there is impaired renal function, they also give it.
Or if reb. up to a year, they can give it for a year, if after a year there is a violation of the function. no, they take it off. If there is renal or heart failure, then it is prescribed
.
and if there is no deficiency, then thank God. there must be either a dysfunction, or pronounced morphological changes without a violation of the function of organs is not allowed
Refer to.
Types of heart defects
| Type | Name |
| Congenital | |
| Without the development of cyanosis (pale type) | Defects of the interventricular and interatrial septa |
| Patent ductus arteriosus | |
| Pulmonary stenosis | |
| Coarctation of the aorta | |
| With the development of cyanosis (blue) | Transposition of the great vessels |
| Common ventricle | |
| Tetralogy of Fallot | |
| Purchased | |
| Mitral valve (between the left atrium and ventricle) | Mitral stenosis |
| Mitral regurgitation | |
| Tricuspid valve (between the right atrium and ventricle) | Tricuspid valve stenosis |
| Tricuspid valve insufficiency | |
| Aortic valve (between the left ventricle and the aorta) | Aortic stenosis |
| Aortic insufficiency | |
| Pulmonary valve | Pulmonary valve stenosis |
| Pulmonary valve insufficiency | |
Stenosis
- narrowing of the valve opening, which causes difficulty in blood flow.
Failure
- inability of the valves to close tightly. In people with valve stenosis, valve insufficiency develops over time - this is called combined PS.
Septal disorders:
A condition in which the septum between the chambers of the heart is damaged:
- atrial septum -
“extra” blood enters the right atrium and causes it to enlarge; - interventricular
- blood flows from the right to the left ventricle, expanding its boundaries.
Changes are found in 2 out of 1000 newborns. Perhaps the most favorable form, since small defects can heal on their own.
Coarctation of the aorta:
Narrowing of the lumen of the main vessel in the area of the isthmus - the transition of the arch to the descending part. The defect causes disruption of the blood supply to organs. This form of pathology accounts for 10% of all defects. Often combined with disruption of interchamber septa. A serious condition requiring medical attention immediately after birth.
Pulmonary valve stenosis:
At the site of the valves from the right ventricle to the pulmonary artery, a narrowing occurs. The heart requires more effort to pump blood. 10% of the total number of defects.
Transposition of the great vessels:
Rare pathology (about 5%). In this case, the main vessels “change places.” Arterial blood flows through the veins, and venous blood through the arteries.
Tetralogy of Fallot:
The most severe form. Consists of four violations simultaneously:
- the opening between the left and right ventricles;
- pulmonary stenosis – narrowing of the pulmonary trunk;
- enlargement of the right ventricle;
- Aortic displacement is the exit of the aorta from the heart in an atypical location.
catalogue of articles
MSE and disability in congenital heart disease
Medical and social examination and disability in congenital heart disease
MSE and disability in congenital heart defects
CONGENITAL HEART DEFECTS are abnormalities in the development of the heart, manifested by disruption of the formation of normal hemodynamics after the birth of a child.
ICD X headings: Q 20—Q 26.
Epidemiology: the frequency among newborns is 0.8-1% in the countries of the European continent; In Russia, from 40 to 45 thousand children are born annually with congenital heart defects.
Etiology and pathogenesis. In 90% of cases, congenital heart defects develop as a result of disturbances in the intrauterine development of the fetus and exposure to teratogenic factors (infections, drugs, chemicals, adverse environmental influences, etc.) during the period of embryogenesis (2-8 weeks of pregnancy), when the formation of the fetus occurs. and organogenesis of the cardiovascular system. In 5% of cases, these defects are part of a syndrome with multiple damage to organs and systems caused by chromosomal aberrations, and in 3.5% - a mutation of single genes, i.e., hereditary. Violation of organogenesis of the cardiovascular system leads to the development of various anatomical defects: communications between the right and left chambers of the heart or great vessels, anomalies of the valvular apparatus of the heart and great vessels. The size and location of the defect determine hemodynamic disturbances and the degree of their severity, which determines the clinical picture of the defect.
Clinical picture. Depending on hemodynamic disturbances, all defects are divided into defects with depletion or enrichment of the pulmonary circulation, with depletion of the systemic circulation, without hemodynamic disturbances, as well as with and without cyanosis, which is caused by an arteriovenous or venoarterial shunt. Heart defects with enrichment of the pulmonary circulation without cyanosis include open
ductus arteriosus, ASD and VSD, atrioventricular communication; with cyanosis: Eisenmenger complex, transposition of the great vessels, common truncus arteriosus; with depletion of the pulmonary circulation without cyanosis - isolated stenosis of the pulmonary trunk, with cyanosis: Fallot's disease, tricuspid atresia, transposition of the great vessels with stenosis of the pulmonary trunk, Ebstein's disease, common false truncus arteriosus; with depletion of the systemic circulation - isolated stenosis of the aortic valve and coarctation of the aorta; without hemodynamic disturbances - true and false dextrocardia, anomaly in the position of the aortic arch and its branches, a small VSD in the muscular part.
All congenital defects occur with a certain periodicity: the stage of primary adaptation, the stage of relative compensation and the terminal phase. In the primary adaptation phase, the child’s body adapts to the hemodynamic features caused by the defect. However, adaptation and compensation reactions in a young child are in a state of unstable equilibrium, so decompensation easily occurs with the development of heart failure. At the age of 2-3 years, disturbances in hemodynamics and gas exchange in the child are somewhat compensated: subjective complaints decrease, the physical and psychomotor development of the child improves (the stage of relative compensation, which continues for several years). The terminal phase occurs when all the compensatory capabilities of the body are exhausted, dystrophic and degenerative changes develop in the myocardium and parenchymal organs. For details of the clinical course of each defect, see the relevant articles.
Complications: CH.
Laboratory and instrumental methods confirming the diagnosis:
1) X-ray examination of the chest organs;
2) ECG, EchoCG, FCG;
3) functional tests (according to N.A. Shalkova).
Treatment: conservative treatment (providing emergency care in catastrophic situations, treatment of complications and concomitant diseases), timely referral for consultation with a surgeon. It is advisable to carry out planned surgical treatment in stage II of the defect (phase of relative compensation, 3-12 years), however, with the development of signs of HF in phase I, emergency surgery, often palliative, is necessary in order to carry out radical surgery in phase II, but sometimes radical surgery is immediately performed for emergency indications in phase I, for example, with an open ductus arteriosus or VSD. After radical surgery, the rehabilitation period is 12 months, followed by evaluation of the outcome of the operation.
The prognosis depends on the location of the defect and the size of the defect, on concomitant diseases.
Disability criteria: signs of HF stage IB and higher; rehabilitation period after radical surgery.
Rehabilitation: medical rehabilitation (conservative treatment, solution to the issue of surgical intervention), social adaptation in the family.
Views. 4971
| Rating.
3.5
/
2
Symptoms of heart defects in newborns and children
Usually the pathology is detected by a neonatologist in the first days of a baby’s life:
- cyanosis (blue discoloration) or grayness of the skin;
- tachypnea - rapid shallow breathing;
- widening of the nostrils when inhaling;
- grunting while inhaling;
- swelling of the legs, abdomen, face;
- breathing problems when feeding.
In a less severe form, it manifests itself at a growing age:
- fatigue during exertion;
- shortness of breath, pain in the heart area when playing sports;
- swelling of the hands, ankles, feet.
The earlier the clinical manifestations appear, the more difficult the process.
Important! Note to parents
Regardless of whether a child has a heart pathology or not, it is necessary to undergo regular medical examinations.
It is especially important to make an appointment with a pediatric cardiologist before starting sports. There are disorders in which the cardiovascular system can cope with them through compensatory force. Diseases go undetected for years.
When playing sports, the load on the cardiovascular system increases many times over. Compensatory mechanisms in this mode are often insufficient, which is manifested by dizziness, loss of consciousness, and can cause a life-threatening condition for the child.
This does not mean that playing sports is strictly contraindicated. The type of sport and load must be determined by a doctor.
If a child is diagnosed with a heart defect, medical supervision when playing sports is mandatory. A medical examination by a pediatric cardiologist, pediatrician, or cardiac surgeon is required.
Diagnosis of heart defects in children
During the initial examination, a pediatrician, neonatologist or pediatric cardiologist conducts an examination and auscultation of possible heart murmurs. The presence of swelling, shortness of breath, heart rhythm disturbances, and problems with physical or intellectual development are checked. Based on the results of the inspection, the question of the necessary examination is decided.
Cardiac echocardiography (EchoCG) – combines cardiac ultrasound and cardiogram. The method determines the rhythmogram and structural changes in the heart. EchoCG is an informative method.
Radiology shows the actual size of the heart, its chambers and the relationship of the organ to the size of the chest.
Coronary angiography – a catheter is inserted through the veins or arteries in the arm, groin, or neck (vein only) and reaches the heart. Then a contrast agent is passed through it. This method determines the contractile function of the heart.
Medical equipment uses expert-class equipment from world-famous manufacturers.
The task of the Children's Medical Department is to provide a full range of medical care from prevention to treatment, when symptoms of a defect appear from birth to 18 years.
In our children's department, appointments are conducted by doctors who have undergone special training to identify health problems in children and infants, taking into account all age-related characteristics.
Pediatric doctors at the Paracelsus Clinic work according to the principles of evidence-based medicine (international protocols drawn up on the basis of clinical trials). This minimizes the likelihood of a false diagnosis.
Parents play a big role in the early diagnosis of heart defects in children. The direction in which the preliminary examination will be carried out depends on how closely the parents monitor the health of their child and how correctly they can describe his condition to the doctor.
How to register a disability: about passing a medical and social examination
The decision to recognize a person as disabled is made by federal state institutions of medical and social examination based on the results of the examination. However, the Moscow Department of Labor and Social Protection receives many questions about how to register disability. We describe the algorithm of actions.
A referral for a medical and social examination (MSE) can be obtained from medical organizations, as well as from bodies providing pensions, from social protection bodies if the citizen has medical documents confirming impairment of body functions due to diseases, consequences of injuries or defects. Only the attending physician, knowing the diagnosis, results of treatment, rehabilitation and habilitation of the patient, determines whether there are signs of disability, so it is best to contact him for a referral for medical examination.
To pass the ITU, the corresponding application and necessary documents are submitted to the ITU office at the place of residence. Information on the addresses of divisions of the Bureau of Medical and Social Expertise in cities and regions can be found on the website.
List of documents for examination at the Bureau of Medical and Social Expertise:
- Consent of the citizen (his legal or authorized representative);
- An identification document (passport or other identification document), for foreign citizens and stateless persons permanently residing in the territory of the Russian Federation - additionally a “residence permit”; the refugee certificate is presented in person, for non-resident citizens - a certificate of registration at the place of residence;
- A referral for a medical and social examination issued by a medical organization or a social protection authority, or a pension authority;
- Report on an industrial accident in form N-1 (certified copy);
- Act on occupational disease (certified copy);
- For those discharged from military service - a certificate of illness drawn up by the Military Military Commission (certified copy, the original must be presented in person);
- Conclusion of the interdepartmental expert council on the causal relationship of the disease, disability with exposure to radioactive factors (certified copy, original presented in person);
- Certificate of participant in the liquidation of the consequences of the accident at the Chernobyl nuclear power plant or living in the exclusion or resettlement zone (copy, original presented in person);
- A copy of the work record;
- Medical or military medical documents indicating the citizen’s state of health (outpatient card, hospital extracts, consultant reports, examination results, Red Army or military record book, certificate of injury, etc.);
- Professional and production characteristics from the last place of work.
During the examination, bureau specialists will study the submitted documents, as well as social, everyday, professional and other aspects of the candidate’s life.
A person recognized as disabled receives a certificate of disability indicating the assigned group, as well as an individual rehabilitation or habilitation program (IPRA).
If, based on the results of the examination, a person is not recognized as disabled, then, at the request of the applicant, he is issued a certificate of the results of the medical examination. You can appeal the decision of the ITU within a month from the date of the examination by contacting the bureau that conducted the ITU, in writing on paper or electronically on the State Services website. The bureau also operates a hotline for medical and social examination issues.
We remind you:
Re-examination of people with disabilities of group I is carried out once every 2 years, groups II and III - once a year, and children with disabilities - once during the period for which the child is classified as a “disabled child”.
Important:
During the period from October 2, 2021 to March 1, 2021 inclusive, the “Temporary Procedure for Recognizing a Person as Disabled” (Temporary Procedure) is in effect. Medical and social examination is carried out in absentia .
Recognition of a citizen as a disabled person whose re-examination period begins during the period of validity of the Temporary Order, in the absence of a referral to medical examination, is carried out by extending the previously established disability group (category “disabled child”), the cause of disability, as well as the development of a new individual rehabilitation or habilitation program for a disabled person (child). -disabled person), including previously recommended rehabilitation or habilitation measures.
Disability is extended for a period of 6 months and is established from the date until which the disability was established during the previous examination.
Extension of disability for a citizen who, during a previous examination, was assigned the category of “disabled child” before reaching the age of 18 years and whose re-examination period begins during the period of validity of the Temporary Order, is carried out by establishing disability group I, II or III for a period of 6 months in accordance with the conclusion federal state institution of medical and social examination on the severity of persistent disorders of body functions resulting from diseases, consequences of injuries or defects, information about which is available in the protocol of the citizen’s MSA at the federal state institution of medical and social examination at the last examination.
Extension of disability is carried out without requiring the citizen (his legal or authorized representative) to submit an application for medical examination. In this case, the written consent of the citizen is not required.
Press service of the Department of Labor and Social Protection of the Population of Moscow